Introduction
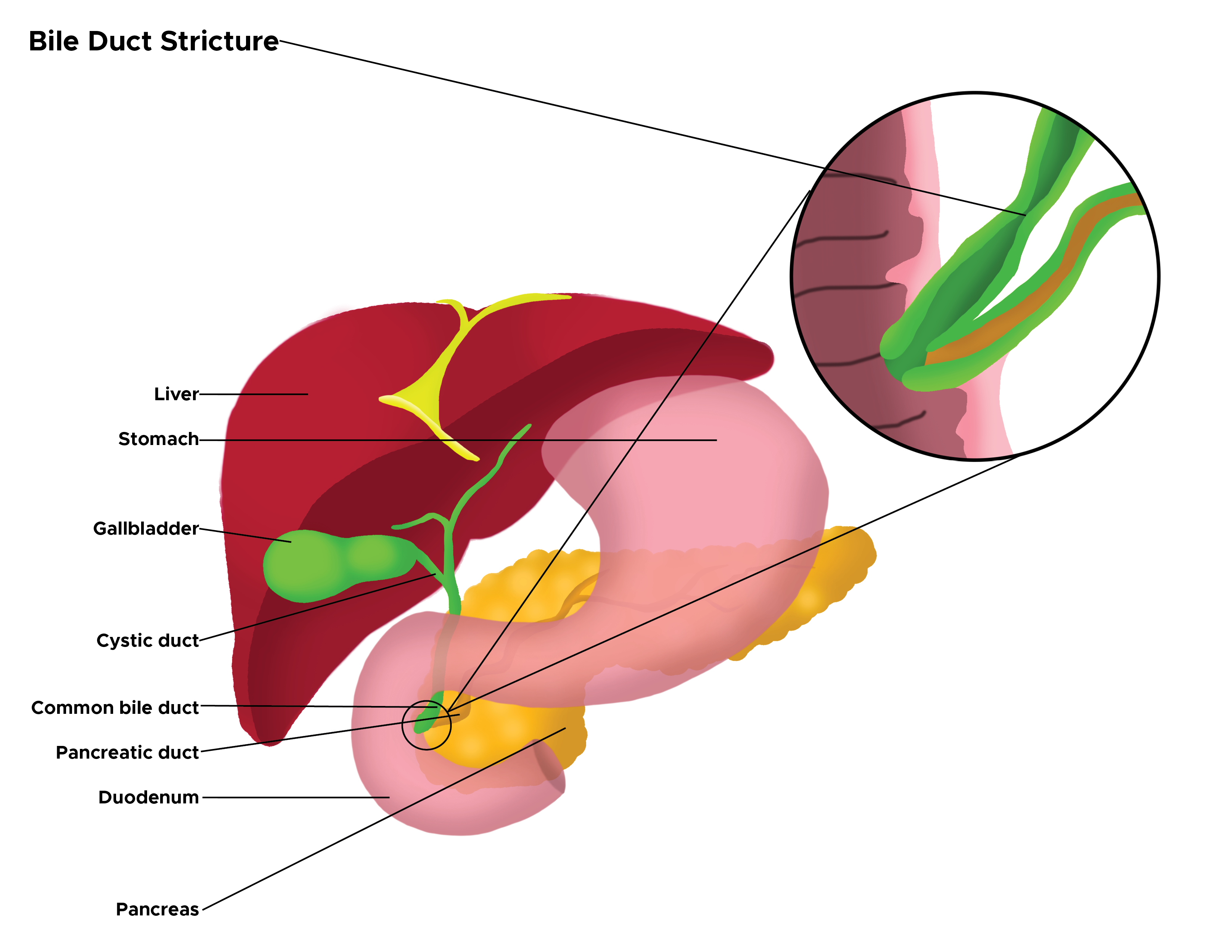
Biliary strictures refer to narrowed intrahepatic or extrahepatic biliary ductal system segments. When narrowed, they impede the normal antegrade flow of bile, causing proximal dilatation, resulting in clinical and pathological sequelae of biliary obstruction. Patients with chronic biliary strictures present a unique challenge when malignancy is suspected. Diagnosing and managing patients with biliary strictures potentially encompasses an interprofessional approach, including interventional endoscopists, surgeons, and interventional radiologists.[1] See Image. Illustration of Bile Duct Stricture.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Bile duct strictures can be congenital or acquired. [2] [3] Acquired strictures are further classified as either benign or malignant. [4] A wide range of benign acquired conditions cause bile duct strictures, contributing to 30% of biliary strictures, including iatrogenic strictures, which comprise the majority of benign biliary strictures. [5] Misidentification of the bile duct as the cystic duct during laparoscopic cholecystectomy leads to bile duct injury, which may be partial or complete. The long-term sequelae of these injuries lead to the formation of benign biliary strictures. [6]
The incidence of injury may be decreased by obtaining an intraoperative cholangiogram, especially in cases of gangrenous cholecystitis or empyema of the gallbladder. [7] [8] The Critical View of Safety, a technique helping surgeons to identify the cystic duct and artery, is utilized to minimize bile duct injuries and associated morbidity from bile leaks and strictures. [9] Understanding the anatomy of the blood supply to the bile duct is paramount to its repair. [10] Pancreatic ductal adenocarcinoma and cholangiocarcinoma are the most common causes of malignant strictures.
Benign causes include:
- Iatrogenic
- Cholecystectomy [11]
- Pancreaticoduodenectomy: Incidence of 4%, especially when there are small-caliber thin-walled ducts [1]
- Liver transplantation [12]
- Due to radiation therapy
- Secondary sclerosing cholangitis due to 5-fluorouracil or bevacizumab chemotherapy (these usually affect the intrahepatic ducts) [13]
- Chronic pancreatitis
- Primary sclerosing cholangitis
- Acute cholangitis
- Blunt and penetrating abdominal trauma
- Autoimmune diseases: Sarcoidosis, immunoglobulin G4 pancreatitis, or eosinophilic cholangitis
- Mirizzi syndrome
- Ischemic cholangiopathy
- Ischemic due to vasculitis
- Systemic mastocytosis
- Langerhans cell histiocytosis
-
Infectious:
- Oriental cholangiohepatitis (due to Ascaris lumbricoides and Clonorchis sinensis infections)
- Acquired immunodeficiency syndrome cholangiopathy
-
Mycobacterium tuberculosis (rare) [14]
- Portal cholangiography (obstruction due to compression of the biliary tree by a portal vein thrombus and portosystemic collateral vessels)
- Biliary inflammatory pseudotumors [3]
Malignant causes (more common than benign biliary strictures):
- Pancreatic head cancer
- Cholangiocarcinoma
- Ampullary carcinoma
- Gallbladder carcinoma
- Hepatocellular carcinoma
- Lymphoma
- Metastasis to regional solid organs and lymph nodes [15]
Epidemiology
Globally, the incidence of biliary strictures is increasing primarily because of iatrogenic bile duct injuries resulting from the widespread practice of laparoscopic cholecystectomy. The estimated rate of biliary injuries is about 0.7% after laparoscopic cholecystectomy. Most of these injuries are minor injuries or bile leaks. Biliary strictures are rare in the pediatric age group.[16] There is no published difference in the incidence or prevalence of biliary strictures in males compared to females. However, some risk factors, like chronic pancreatitis, are more common in males who more often drink alcohol and smoke.
Pathophysiology
Biliary strictures are characterized by narrowing of a bile duct segment associated with proximal ductal dilatation, except in primary or secondary sclerosing cholangitis, where sclerosis prevents the ducts from dilating. Obstruction of bile flow leads to elevation of serum bilirubin levels with clinical and laboratory features of obstructive jaundice. Stasis of bile is a significant risk factor for ascending cholangitis.[17] Magnetic resonance cholangiopancreatography or endoscopic retrograde cholangiopancreatography shows that benign strictures have tapered margins with smooth and symmetric borders. On the other hand, malignant strictures have shouldering of the margins with irregular and asymmetric borders.[12] Malignant strictures typically involve a longer duct segment than benign strictures. Malignant strictures appear to enhance contrast-enhanced cross-sectional imaging.[17]
Histopathology
Generally, histopathological findings in biliary strictures depend on the etiological agent or mechanism. For example, in the case of primary sclerosing cholangitis, histopathology reveals intrahepatic or extrahepatic bile duct inflammation and fibroobliteration.[4] In assessing biliary strictures, histological appraisal with aspiration cytology or tissue biopsy is required to rule out malignancy.[17]
History and Physical
The clinical presentation depends on the location and cause of the stricture.[12] Biliary strictures can be asymptomatic with an unremarkable physical examination. Nevertheless, some patients with biliary strictures present with features of biliary obstruction, including jaundice, pruritus, pale stools, and dark urine.[18] Constitutional symptoms, such as weight loss, fever, nausea, vomiting, and malaise, may also be present. Patients may present with an acute abdomen secondary to cholangitis or a hepatic abscess as complications of the bile duct stricture.[19] A history of fever and leukocytosis suggests an infectious cause or as a result of a stricture. A history of weight loss, abdominal or back pain, and worsening performance status is more suggestive of a malignant etiology.[20] A previous history of hepatobiliary surgery, autoimmune disease, pancreatitis, cholelithiasis, or chemotherapy should be elicited as it can be pivotal in determining the underlying diagnosis.[12]
Physical examination may show specific clinical features, such as a Murphy sign, suggesting biliary stone disease. A Courvoisier sign (a palpable and enlarged but nontender gallbladder) or a palpable abdominal mass elsewhere in the right upper quadrant of the abdomen may point toward pancreatic or biliary malignancy. A Courvoisier sign, however, is not specifically a sign of malignancy, and it may be elicited due to an obstructing distal common bile duct stone or pancreatitis.
Evaluation
The evaluation of biliary strictures is performed using a multi-pronged approach.[21] Contributory laboratory findings are mainly drawn from a liver function test, a coagulation profile, and a complete blood count. Liver function tests typically reveal elevated levels of conjugated bilirubin, alkaline phosphatase, and gamma-glutamyl transferase. Transaminases may or may not be significantly elevated. The prothrombin time and International Normalized Ratio can be prolonged if there is biliary obstruction due to vitamin K malabsorption. Immunological studies may be obtained to assess specific autoimmune etiologies of biliary strictures. Apt diagnosis and further management are based on the correlation of laboratory data and imaging findings with epidemiologic and clinical data.
Deranged liver function tests and coagulation profiles may help to determine the algorithm of subsequent imaging and minimally invasive studies.[20][22] Likewise, when present, certain immunological markers help in accurate diagnosis and management. For example, immunoglobulin (Ig)G4-associated sclerosing cholangitis presents as hilar or distal common bile duct strictures associated with IgG4-related autoimmune pancreatitis. Both of these disease entities are responsive to steroid therapy.[5][12] Antinuclear antibodies and rheumatoid arthritis factors may help support this diagnosis.
Assay of serum carbohydrate antigen or cancer antigen (CA) 19-9 is often elevated in patients with suspected pancreatic ductal adenocarcinoma or cholangiocarcinoma, so it can help with diagnosis and follow-up in some patients with these diagnoses. Of note, the elevation of this marker is not specific to biliary malignancy, can be abnormal in cirrhosis, cholangitis, pancreatitis, gallstones, other malignancies, and hyperbilirubinemia due to any cause of biliary obstruction. For this reason, this marker is best drawn when other diagnostic studies strongly suggest biliary cancer or when monitoring the response to treatment after cancer has been diagnosed. The CA 19-9 level is more likely to be abnormal with larger tumors.
Endoscopic ultrasound-guided fine needle aspiration cytology is highly sensitive and specific in diagnosing malignant biliary strictures, particularly when associated with a mass. Still, it is ineffective in ruling out malignancy.[5] Endoscopic ultrasound-guided fine needle aspiration or tissue sampling at endoscopic retrograde cholangiopancreatography (ERCP) doesn't carry the risk of spreading malignant cells, which is a concern with a percutaneous needle biopsy. Ductal dilatation is a major feature of imaging for biliary strictures.[1] Imaging of suspected biliary strictures can begin with a transabdominal ultrasound, which detects biliary dilatation and is highly sensitive for detecting biliary obstruction and the level of obstruction. However, it has a low yield for the detection of strictures. Malignant biliary strictures typically cause more severe ductal dilation than benign strictures.[5][12]
Computed tomography (CT) scan has higher sensitivity than trans-abdominal ultrasound for biliary malignancy, and its utility can be improved with the use of a multidetector CT scan and CT-pancreatic protocol in providing more information on tumor vascular encroachment and biliary tree obstruction. CT can also detect complications from biliary obstruction, such as cholangitis and abscesses.[1] Magnetic resonance cholangiopancreatography (MRCP) can provide a high-quality cholangiogram, thus establishing the location and extent of biliary strictures. This provides a cross-sectional and 3-dimensional reconstruction of the biliary tree.[4] MRCP helps guide endoscopic therapy, especially if ERCP is contraindicated. MRCP does not use radiation, thus making it a superior option over a multi-detector CT scan. However, its sensitivity and specificity (which can be improved by diffusion-weighted imaging) are comparable to those of ERCP.[1][4]
ERCP can determine the etiology, provide tissue samples for cytology and histology, and facilitate therapeutic interventions, including dilatation and stenting of obstructing biliary (and pancreatic) strictures. However, because of the relatively high risk of post-ERCP pancreatitis, MRCP has replaced ERCP when only a diagnostic study is needed. ERCP is limited to therapeutic interventions. Emerging technologies useful in assessing the etiology of biliary strictures include confocal laser endomicroscopy[23], fluorescent in-situ hybridization (FISH),[24] direct peroral cholangioscopy,[25] and intraductal ultrasound.[4][15][26]2
Treatment / Management
Medical management of biliary strictures is restricted mainly to addressing complications from biliary obstruction, reducing the serum bilirubin to improve absorption of fat, and, in some cases, treating the underlying cause. Therefore, analgesics, empiric antibiotics, hemodynamic support with intravenous fluids with or without vasopressors, and inotropes are instituted where applicable.[27] These efforts are often supportive and in preparation for definitive therapy.[28] Other forms of medical treatment could be aimed at the prevention of further complications like excessive bleeding due to a coagulopathy, as well as deep vein thrombosis and sepsis in the early postoperative period.
The goal of the interventions includes reestablishing ductal patency and avoiding additional procedures.[12][18] There are varying options for operative or interventional management. These options can be accomplished endoscopically, surgically, or percutaneously. The stricture's etiology, location, and the patient's hemodynamic stability and nutritional status could determine the timing and type of intervention required.[28] The Bismuth classification can further guide the most appropriate approach since it offers a guide to determining the level at which healthy biliary tissue is available for repair and anastomosis.[12] Likewise, the Strasberg classification system, which incorporates the presence of a bile leak and lateral injuries into consideration, can also be useful in some cases in choosing the best intervention.[18] Additionally, preoperative determination of malignancy is pivotal to treatment planning. In general, endoscopic treatment is the first line of treatment for biliary strictures,[29] but interventional radiology and surgery are required in some cases. Common interventions for biliary strictures include the options shown below, but managing other specific causes of biliary strictures is outside the scope of this article.
Hydrostatic Balloon Dilatation
- The preferred approach for the management of benign biliary stricture [12]
- Sphincterotomy and hydrostatic balloon dilatation are done for both malignant and benign strictures, including those resulting from primary sclerosing cholangitis [4]
- Commonly performed endoscopically at ERCP, usually to facilitate the placement of one or more stents
- Alternatively, percutaneous transhepatic biliary drainage tracts can be used for access during dilatation [30] (B3)
Stenting
- Usually performed endoscopically, but can be done percutaneously
- Used in the management of both malignant and benign biliary strictures
- Used to reduce hyperbilirubinemia or to drain infected bile in patients with cholangitis before definitive surgery [22]
- Useful for palliation of inoperable malignant strictures
- Plastic, uncovered self-expandable metal stent (SEMS), or retrievable covered SEMS can be used alone or in combination, depending on the clinical indication [18]
- A percutaneous transhepatic biliary drainage catheter may be placed to palliate hyperbilirubinemia in patients with cancer who either have inoperable disease or until completion of neoadjuvant therapy.
Surgery
- Resection and anastomosis have a role in some diagnoses depending on the underlying etiology of the stricture and whether the desired outcome is palliative or curative.[28] Surgical resection for this indication is associated with significant morbidity and high cost.[5]
- Bypass: Hepaticojejunostomy and choledochoduodenostomy are performed in some instances.[28]
- Mirizzi syndrome is managed by exploratory surgery with cholecystectomy and clearance of the impacted stone from the cystic duct or gallbladder neck.
Other Techniques
- Another technique is intraductal radiofrequency ablation for palliation of extrahepatic cholangiocarcinoma, a simpler and less risky alternative to intraluminal brachytherapy or photodynamic therapy.[31]
- Placement of biodegradable stents may be options.[17]
- Percutaneous large-bore catheterization with progressive dilatation up to 20 French is another technique.[32]
- Magnetic compression anastomosis: Magnets are placed on either side of a benign biliary stricture, on the distal side by ERCP, and on the proximal side by percutaneous transhepatic cholangiography. The magnetic attraction causes tissue compression, ischemic necrosis, and eventual recanalization.[33] The risk of re-stenosis is reduced by maintenance of the lumen with a stent or percutaneous internal drain for 6 months after initial recanalization.[34]
Differential Diagnosis
In diagnosing and managing biliary strictures, the most valuable and critical distinction that should be made is between benign and malignant etiology. This differentiation presents a major diagnostic and therapeutic challenge. Therefore, elaborate history taking, physical examination, and diagnostic workup should be completed.[15] Other techniques like fluorescence in situ hybridization, Kras/p53 mutation analysis, intraductal biopsies, and confocal laser endomicroscopy may be considered to improve the diagnostic yield.[5] A diagnosis of choledocholithiasis should also be considered in cases of suspected biliary strictures.
Prognosis
The mortality in patients with biliary structures depends on the underlying etiology. Biliary strictures due to chronic pancreatitis, trauma, or operative injury have a good prognosis. In contrast, those resulting from malignancy, treatment of malignancy (ie, strictures due to radiation therapy and chemotherapy), primary sclerosing cholangitis, and patients with human immunodeficiency virus cholangiopathy usually have a less favorable prognosis.
Complications
The consequences of chronic biliary obstruction can complicate biliary strictures.[29] These complications include:
- Recurrent episodes of cholangitis
- Gram-negative septicemia
- Biliary stone formation
- Hepatic abscesses
- Secondary biliary cirrhosis
- End-stage liver disease
- Cholangiocarcinoma
Other complications could result from interventional procedures, and these may include:
- Pancreatitis
- Cholangitis
- Bleeding
- Biliary perforation
- Additionally, there are reports of distal migration of biliary stents leading to duodenal perforation.[35] Tumor ingrowth can also complicate stents, rendering them non-functional.[29] Covered SEMS are more prone to migration, while uncovered SEMS have a greater risk of tumor ingrowth.
Consultations
Biliary strictures frequently present a challenge in terms of diagnosis, necessitating interdisciplinary collaboration. Likewise, patients with benign strictures may have a protracted, complicated course calling for multiple consultations.[29] Therefore, teams caring for patients with biliary strictures may comprise:
- Gastrointestinal endoscopists
- Interventional radiologists
- Hepatobiliary surgeons
- Medical oncologists
- Diagnostic radiologists
- Surgical oncologists
- Nurses with experience in managing ostomies and drains
Deterrence and Patient Education
Patients drinking alcohol should be counseled against the practice, especially those with chronic pancreatitis, whose diagnosis is linked to drinking. Patients who have biliary stents placed should be educated about recognizing symptoms and signs of blocked stents causing biliary obstruction, cholangitis, and possible sepsis (including abdominal pain, jaundice, pruritus, fever, chills, and sweats). Those with external drains should be taught to flush them using aseptic measures. Lastly, the patient and their caregivers should be informed about the prognosis of their underlying disease.
Enhancing Healthcare Team Outcomes
Bile duct strictures may present with nonspecific signs and symptoms of obstructive jaundice, abdominal pain, nausea, vomiting, fever, and leukocytosis. The cause of bile duct strictures may be one of many possible benign and malignant diagnoses. The complexity of this disease process lies in the challenges of its diagnosis and subsequent management. Inaccurate diagnosis or delay in management can have devastating outcomes for the patient. The interprofessional team of specialists may include gastroenterologists, interventional radiologists, hepatobiliary surgeons, surgical oncologists, transplant surgeons, and nurses trained in managing ostomies and external drains.
The Society of American Gastrointestinal and Endoscopic Surgeons offers guidelines for the clinical application of laparoscopic biliary tract surgery (https://www.sages.org/publications/guidelines/guidelines-for-the-clinical-application-of-laparoscopic-biliary-tract-surgery), though these guidelines have not been revised since 2010. In the context of biliary strictures, the guidelines suggest that the factors associated with bile duct injury include surgeon experience, patient age, male sex, and acute cholecystitis. If significant bile duct injuries occur, outcomes are improved by early recognition and immediate referral to experienced hepatobiliary specialists for further treatment before the primary surgeon attempts any repair unless the primary surgeon has significant experience in biliary reconstruction. Nurses play a vital role during the recovery of such patients, helping in the timely recognition of common postoperative complications such as deep vein thrombosis and anastomotic leaks. The roles of the laboratory personnel and pharmacists are critical as well. The pharmacist may be involved in managing parenteral nutrition for critically ill patients.
Media
(Click Image to Enlarge)
References
Israr S, Rubalcava NS, Weinberg JA, Jones M, Gillespie TL. Management of Biliary Stricture Following Emergent Pancreaticoduodenectomy for Trauma: Report of Two Cases. Cureus. 2018 Jun 18:10(6):e2829. doi: 10.7759/cureus.2829. Epub 2018 Jun 18 [PubMed PMID: 30131922]
Level 3 (low-level) evidenceNarayan KS, Kumar M, Padhi S, Jain M, Ashdhir P, Pokharna RK. Tubercular biliary hilar stricture: A rare case report. The Indian journal of tuberculosis. 2018 Jul:65(3):266-267. doi: 10.1016/j.ijtb.2017.06.013. Epub 2017 Aug 12 [PubMed PMID: 29933873]
Level 3 (low-level) evidenceRodrigues T, Boike JR. Biliary Strictures: Etiologies and Medical Management. Seminars in interventional radiology. 2021 Aug:38(3):255-262. doi: 10.1055/s-0041-1731086. Epub 2021 Aug 10 [PubMed PMID: 34393335]
Tabibian JH, Baron TH. Endoscopic management of primary sclerosing cholangitis. Expert review of gastroenterology & hepatology. 2018 Jul:12(7):693-703. doi: 10.1080/17474124.2018.1483719. Epub 2018 Jun 18 [PubMed PMID: 29883229]
Singh A, Gelrud A, Agarwal B. Biliary strictures: diagnostic considerations and approach. Gastroenterology report. 2015 Feb:3(1):22-31. doi: 10.1093/gastro/gou072. Epub 2014 Oct 28 [PubMed PMID: 25355800]
Moghul F, Kashyap S. Bile Duct Injury. StatPearls. 2025 Jan:(): [PubMed PMID: 31536309]
Kowalski A, Kashyap S, Mathew G, Pfeifer C. Emphysematous Cholecystitis. StatPearls. 2025 Jan:(): [PubMed PMID: 28846291]
Kashyap S, Mathew G, King KC. Gallbladder Empyema. StatPearls. 2025 Jan:(): [PubMed PMID: 29083646]
Antonopoulou MI, Manatakis DK. Critical View of Safety in Laparoscopic Cholecystectomy: A Word of Caution in Cases of Aberrant Anatomy. Surgery journal (New York, N.Y.). 2022 Jul:8(3):e157-e161. doi: 10.1055/s-0042-1744154. Epub 2022 Oct 18 [PubMed PMID: 36267420]
Level 3 (low-level) evidenceSeeras K, Qasawa RN, Kashyap S, Kalani AD. Bile Duct Repair. StatPearls. 2025 Jan:(): [PubMed PMID: 30252245]
Level 2 (mid-level) evidenceStrasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. Journal of the American College of Surgeons. 1995 Jan:180(1):101-25 [PubMed PMID: 8000648]
Level 2 (mid-level) evidenceShanbhogue AK, Tirumani SH, Prasad SR, Fasih N, McInnes M. Benign biliary strictures: a current comprehensive clinical and imaging review. AJR. American journal of roentgenology. 2011 Aug:197(2):W295-306. doi: 10.2214/AJR.10.6002. Epub [PubMed PMID: 21785056]
Kusakabe A, Ohkawa K, Fukutake N, Sakakibara M, Imai T, Abe Y, Takada R, Ikezawa K, Nawa T, Ashida R, Kimura T, Nagata S, Katayama K. Chemotherapy-Induced Sclerosing Cholangitis Caused by Systemic Chemotherapy. ACG case reports journal. 2019 Jul:6(7):e00136. doi: 10.14309/crj.0000000000000136. Epub 2019 Jul 17 [PubMed PMID: 31620533]
Level 3 (low-level) evidenceChadha VK, Bhalla BB, Ramesh SB, Gupta J, Nagendra N, Padmesh R, Ahmed J, Srivastava RK, Jaiswal RK, Praseeja P. Tuberculosis diagnostic and treatment practices in private sector: Implementation study in an Indian city. The Indian journal of tuberculosis. 2018 Oct:65(4):315-321. doi: 10.1016/j.ijtb.2018.06.010. Epub 2018 Jul 11 [PubMed PMID: 30522619]
Paranandi B, Oppong KW. Biliary strictures: endoscopic assessment and management. Frontline gastroenterology. 2017 Apr:8(2):133-137. doi: 10.1136/flgastro-2016-100773. Epub 2017 Feb 10 [PubMed PMID: 28261440]
Chapoy PR, Kendall RS, Fonkalsrud E, Ament ME. Congenital stricture of the common hepatic duct: an unusual case without jaundice. Gastroenterology. 1981 Feb:80(2):380-3 [PubMed PMID: 7450427]
Level 3 (low-level) evidenceMa MX, Jayasekeran V, Chong AK. Benign biliary strictures: prevalence, impact, and management strategies. Clinical and experimental gastroenterology. 2019:12():83-92. doi: 10.2147/CEG.S165016. Epub 2019 Feb 18 [PubMed PMID: 30858721]
Kapoor BS, Mauri G, Lorenz JM. Management of Biliary Strictures: State-of-the-Art Review. Radiology. 2018 Dec:289(3):590-603. doi: 10.1148/radiol.2018172424. Epub 2018 Oct 23 [PubMed PMID: 30351249]
Kopitnik NL, Kashyap S, Dominique E. Acute Abdomen. StatPearls. 2025 Jan:(): [PubMed PMID: 29083722]
Level 2 (mid-level) evidenceLorenz JM. Management of Malignant Biliary Obstruction. Seminars in interventional radiology. 2016 Dec:33(4):259-267 [PubMed PMID: 27904244]
Raza D, Singh S, Crinò SF, Boskoski I, Spada C, Fuccio L, Samanta J, Dhar J, Spadaccini M, Gkolfakis P, Maida MF, Machicado J, Spampinato M, Facciorusso A. Diagnostic Approach to Biliary Strictures. Diagnostics (Basel, Switzerland). 2025 Jan 30:15(3):. doi: 10.3390/diagnostics15030325. Epub 2025 Jan 30 [PubMed PMID: 39941254]
Pu LZ, Singh R, Loong CK, de Moura EG. Malignant Biliary Obstruction: Evidence for Best Practice. Gastroenterology research and practice. 2016:2016():3296801. doi: 10.1155/2016/3296801. Epub 2016 Feb 11 [PubMed PMID: 26981114]
Pilonis ND, Januszewicz W, di Pietro M. Confocal laser endomicroscopy in gastro-intestinal endoscopy: technical aspects and clinical applications. Translational gastroenterology and hepatology. 2022:7():7. doi: 10.21037/tgh.2020.04.02. Epub 2022 Jan 25 [PubMed PMID: 35243116]
Zoundjiekpon VD, Falt P, Zapletalova J, Vanek P, Kurfurstova D, Slobodova Z, Skanderova D, Korinkova G, Skalicky P, Lovecek M, Urban O. Fluorescence In Situ Hybridization in Primary Diagnosis of Biliary Strictures: A Single-Center Prospective Interventional Study. Biomedicines. 2023 Mar 2:11(3):. doi: 10.3390/biomedicines11030755. Epub 2023 Mar 2 [PubMed PMID: 36979734]
Subhash A, Buxbaum JL, Tabibian JH. Peroral cholangioscopy: Update on the state-of-the-art. World journal of gastrointestinal endoscopy. 2022 Feb 16:14(2):63-76. doi: 10.4253/wjge.v14.i2.63. Epub [PubMed PMID: 35316979]
Zhou S, Buxbaum J. Advanced Imaging of the Biliary System and Pancreas. Digestive diseases and sciences. 2022 May:67(5):1599-1612. doi: 10.1007/s10620-022-07389-9. Epub 2022 Feb 16 [PubMed PMID: 35171407]
Dadhwal US, Kumar V. Benign bile duct strictures. Medical journal, Armed Forces India. 2012 Jul:68(3):299-303. doi: 10.1016/j.mjafi.2012.04.014. Epub [PubMed PMID: 24532893]
Kukar M, Wilkinson N. Surgical Management of Bile Duct Strictures. The Indian journal of surgery. 2015 Apr:77(2):125-32. doi: 10.1007/s12262-013-0972-7. Epub 2013 Sep 20 [PubMed PMID: 26139967]
Wong MYW, Kaffes AJ. Benign Biliary Strictures: Narrowing the Differences Between Endoscopic and Surgical Treatments. Digestive diseases and sciences. 2018 Oct:63(10):2495-2496. doi: 10.1007/s10620-018-5212-3. Epub [PubMed PMID: 30054841]
Inui K, Yoshino J, Miyoshi H. Differential diagnosis and treatment of biliary strictures. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2009 Nov:7(11 Suppl):S79-83. doi: 10.1016/j.cgh.2009.08.027. Epub [PubMed PMID: 19896104]
Level 3 (low-level) evidenceWeismüller TJ. Role of Intraductal RFA: A Novel Tool in the Palliative Care of Perihilar Cholangiocarcinoma. Visceral medicine. 2021 Feb:37(1):39-47. doi: 10.1159/000513970. Epub 2021 Jan 7 [PubMed PMID: 33718482]
Ludwig JM, Webber GR, Knechtle SJ, Spivey JR, Xing M, Kim HS. Percutaneous Management of Benign Biliary Strictures with Large-Bore Catheters: Comparison between Patients with and without Orthotopic Liver Transplantation. Journal of vascular and interventional radiology : JVIR. 2016 Feb:27(2):219-225.e1. doi: 10.1016/j.jvir.2015.10.021. Epub 2015 Dec 17 [PubMed PMID: 26710970]
Jang SI, Choi J, Lee DK. Magnetic compression anastomosis for treatment of benign biliary stricture. Digestive endoscopy : official journal of the Japan Gastroenterological Endoscopy Society. 2015 Jan:27(2):239-49. doi: 10.1111/den.12319. Epub 2014 Oct 16 [PubMed PMID: 24905938]
Jang SI, Lee KH, Yoon HJ, Lee DK. Treatment of completely obstructed benign biliary strictures with magnetic compression anastomosis: follow-up results after recanalization. Gastrointestinal endoscopy. 2017 May:85(5):1057-1066. doi: 10.1016/j.gie.2016.08.047. Epub 2016 Sep 9 [PubMed PMID: 27619787]
Ferm S, Fisher C, Hassam A, Rubin M, Kim SH, Hussain SA. Primary Endoscopic Closure of Duodenal Perforation Secondary to Biliary Stent Migration: A Case Report and Review of the Literature. Journal of investigative medicine high impact case reports. 2018 Jan-Dec:6():2324709618792031. doi: 10.1177/2324709618792031. Epub 2018 Aug 2 [PubMed PMID: 30116760]
Level 3 (low-level) evidence