Ultrasound-Guided Fascia Iliaca Compartment Block
Ultrasound-Guided Fascia Iliaca Compartment Block
Introduction
Pain management is an integral part of providing care in the emergency setting. Lower extremity pain from hip fractures, burns, and other trauma is a common presenting complaint. Pain management can be complex due to medication side effects, patient preferences, and other patient characteristics that can make intravenous analgesia less desirable. Opioid medications can be associated with respiratory depression, hypotension, mental status changes, and vomiting. Non-steroidal anti-inflammatory drugs (NSAIDs) can increase bleeding risk and exacerbate underlying gastrointestinal (GI) problems. Acetaminophen alone is often not sufficient for severe pain. Hip fractures, in particular, can cause considerable pain and frequently occur in elderly adults with multiple comorbidities, which makes analgesia challenging.
A fascia iliaca compartment block can provide superior analgesia with minimal side effects. This block can be deployed quickly after a small amount of training and can be executed with high success rates under ultrasound guidance. In a study by Monzon et al, patients who received a fascia iliaca compartment block for a hip fracture had significantly reduced pain levels.[1] The pain was initially rated at an average of 8.5 on a 10-point scale but decreased to an average of 2.3 at 2 hours postinjection. In a study by Stevens et al, patients who underwent a fascia iliaca compartment block used significantly less morphine over 24 hours than the control group, which used morphine alone.[2] An additional advantage is the duration of effect, which has been seen for 8 to 10 hours following a single shot block. Another randomized placebo-controlled trial showed that pain relief was superior at all time points measured in the fascia iliac compartment block group as compared with a group utilizing morphine only. Median total morphine consumption in the compartment block group was 0 mg due to excellent analgesia after only a compartment block. Similar results were seen in a study by Lopez et al for femoral shaft fractures. Emergency department-specific studies using ultrasound guidance have shown 76% mean reduction of pain score in patients with hip fractures at 120 minutes.[3][4]
Notably, some physicians now prefer to use a pericapsular nerve group (PENG) block over the fascia iliaca block technique. Some studies suggest that the PENG technique provides superior pain control. Either method provides an important opiate sparing alternative for pain management in these patients.[5][6]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
Sensory innervation of the lower extremity is primarily provided by the femoral, obturator, lateral femoral cutaneous, and sciatic nerves. All except the sciatic nerve originate from the lumbar plexus; the sciatic nerve receives contributions from the sacral plexus. Understanding the anatomy and distribution of these nerves is critical for adequate regional anesthesia, particularly when performing a fascia iliaca compartment block.
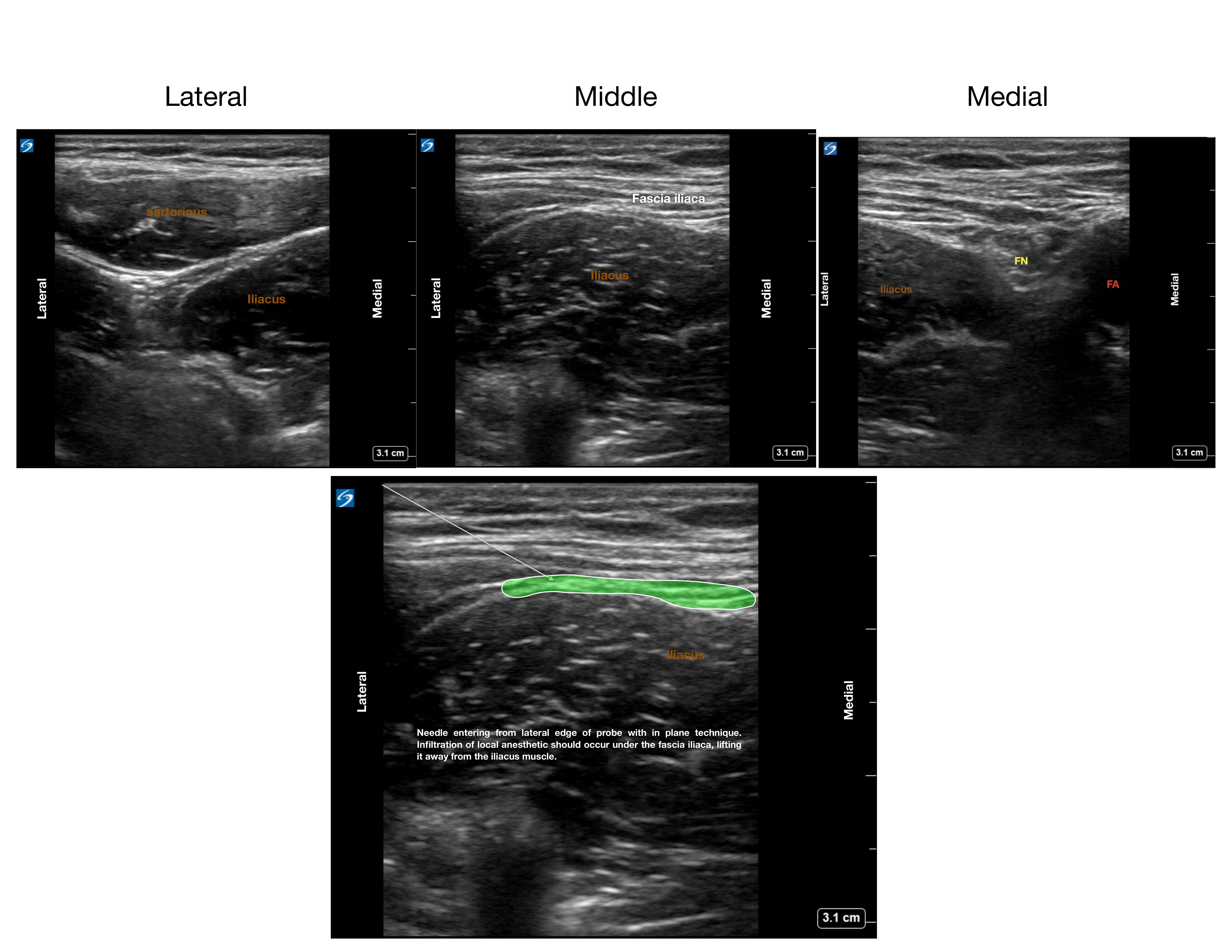
The femoral nerve, the largest of the 4, lies just lateral to the femoral artery and superficial to the iliacus muscle, separated from the artery by the fascia iliaca (see Image. Anatomy Fascia Iliaca and Ideal Needle Positioning). This nerve is often visualized on ultrasound by emergency physicians during femoral vein cannulation. The obturator nerve courses through the psoas muscle and passes behind the common iliac vessels, providing sensation to a small region of the medial thigh. This nerve may be inconsistently blocked with a fascia iliaca compartment block. The lateral femoral cutaneous nerve, which supplies sensation to the lateral thigh, travels behind the lateral portion of the inguinal ligament. The sciatic nerve, innervating the posterior thigh, is not affected by an anteriorly placed anesthetic, as it lies deep in the posterior compartment.
The fascia iliaca is the second fascial layer encountered on ultrasound after the fascia lata when imaging the proximal thigh, and it lies anterior to the iliacus, psoas, and pectineus muscles. In blind techniques, clinicians may feel 2 distinct “pops” as the needle passes through the fascia lata and then the fascia iliaca. The femoral vessels and sartorius muscle are located between these 2 fascial layers. A properly performed fascia iliaca compartment block can anesthetize the femoral, lateral femoral cutaneous, genitofemoral, and sometimes the obturator nerve, making it an effective regional anesthesia option for anterior hip and thigh procedures.
Indications
This compartment block can be used for any painful trauma or procedures in the lower extremity within the nerve distribution mentioned above. This block is useful when opioid analgesics are not ideal or are contraindicated, and can also be combined with opioids for pain that is difficult to control. Specific indications studied include hip fractures, femoral shaft fractures, and burns.
Contraindications
The contraindications to this procedure include:
- The patient's unwillingness to consent to the procedure
- Known allergy to local anesthetics
- Local anesthetic injection, which has already approached the maximum dosage
- Previous femoral bypass surgery
- Local infection at the injection site
- Anticoagulation (relative)
Equipment
The following equipment is needed to perform this compartment block:
- Portable ultrasound machine with a linear high-frequency transducer
- Surgical marking pen
- Sterile probe covers
- Antiseptic solution
- Spinal needle or nerve block specific needle
- 30-gauge short needle
- 3-mL syringe
- 20- to 60-mL syringe
- Long-acting local anesthetic
- Cardiac monitor with continuous pulse oximetry
- Intralipid and plan for local anesthetic toxicity response
- Cardiopulmonary resuscitation equipment, including pertinent medications and airway management items, is immediately available
Personnel
Past literature has supported the effectiveness of regional anesthesia by both anesthesiologists and emergency physicians. More recent studies have shown that resident physicians can reliably perform a fascia iliaca compartment block after minimal amounts of training. A study published in the Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine has shown that prehospital emergency medical services (EMS) nurses can also demonstrate competency in a fascia iliaca compartment block using a blind technique.
Preparation
Preparation is necessary for achieving a successful and safe compartment block. As with any other procedure, the risks and benefits of the proposed procedure should be explained to the patient in a way that is easy for them to understand. Time should be taken to answer any questions they may have. Written consent should be obtained at that time. If deemed appropriate, a small dose of an anxiolytic may assist in relieving any preprocedure anxiety and facilitate proper positioning and cooperation. A detailed neurovascular exam of the lower extremity should be obtained before the start of the procedure. The site of the planned compartment block should be marked with a surgical marking pen and initialed by the provider intending to complete the procedure. The equipment and supplies necessary for completing the procedure should be collected and set up in the room.
Technique or Treatment
The authors have utilized the following techniques and found them to be effective. The authors recognize that various successful strategies have been employed to perform this block, and alternative techniques may be equally appropriate.
- Explain the procedure and obtain written consent as noted above.
- Document a detailed neurovascular exam.
- Ensure all needed supplies are at the bedside.
- Perform the timeout procedure with an additional clinician or nurse.
- Administer a small dose of intravenous anxiolytic if appropriate and deemed necessary.
- Identify the neurovascular bundle utilizing ultrasound with the probe marker to the patient's right and mark the femoral artery with the surgical marking pen.
- Place sterile gloves, and with the help of an assistant, apply a sterile probe cover to the ultrasound.
- Clean the area using an antiseptic solution in the usual sterile fashion and place small sterile drapes.
- Again, identify the femoral vessels with ultrasound and then slide the probe laterally, away from the neurovascular bundle. This is done while at all times keeping the fascia iliaca in view.
- Place a small amount of 1% lidocaine using the 30-gauge short needle to form a skin wheal in the intended area of injection.
- Fill a large syringe connected to a spinal needle or nerve block needle with long-acting local anesthetic. Be sure not to exceed the maximum dosing of local anesthetic. The authors have found that 20 mL of 0.5% bupivacaine mixed with 10 mL of sodium chloride solution is generally safe and effective for an average-sized adult.
- Insert the needle in the area of the previously created skin wheal in an in-plane technique. The needle tip should be in constant view under dynamic ultrasound guidance. Advance the needle until the fascia iliaca has just been punctured.
- Withdraw/aspirate to ensure that there is no blood return, indicating entrance into a vessel.
- Carefully inject a small amount of anesthetic and observe the separation of the fascia iliaca from the underlying muscle planes. Continue to inject and aspirate every 5 mL to ensure correct placement. The anesthetic should flow easily into the space with minimal resistance. There should never be any blood return when checking aspiration. The provider may periodically elect to move the transducer more medially to view the anesthetic surrounding the femoral nerve directly. If this is done, the injection should pause, and the needle should be held in place without any advancement or retraction until the ultrasound is moved back to view the needle tip.
- During the procedure, the clinician should frequently evaluate the cardiac monitor for any signs of ectopy. If any ectopy is noted, the injection should immediately cease. Additionally, the clinician may want to ask the patient about any symptoms of local anesthetic toxicity, such as lightheadness, dizziness, perioral numbness, or tingling. This assessment should be repeated at the end of the procedure. If any signs of local anesthetic toxicity are observed, help should be requested, and Intralipid should be considered.
- Following the procedure, a repeat neurovascular exam should be documented in the procedure note. The clinician should note the time of the block in their procedure note and mark it with a surgical marking pen at the site of injection.
Complications
The overall complication rates for this procedure are low. In an emergency department study of 63 adult patients who underwent single fascia iliac compartment block by resident physicians after 5 minutes of instruction, no systemic complications were found, and only 2 local hematomas occurred.[7] Even when the procedure was performed blindly by EMS nurses in the prehospital setting, there were no complications noted in a study enrolling 100 patients.[8] The distance at which the skin is punctured from the neurovascular bundle minimizes the risk of intravascular injection or nerve transection. Intravascular injection or nerve damage is exceedingly rare.
Clinical Significance
The fascia iliaca compartment block is clinically significant as an effective, relatively low-risk regional anesthesia technique for providing analgesia to the hip, thigh, and knee, particularly in patients with hip fractures, femoral shaft fractures, or undergoing hip arthroplasty. Effective pain management is essential in the emergency setting, particularly for lower extremity injuries such as hip fractures. Traditional pharmacologic approaches, including opioids, NSAIDs, and acetaminophen, present limitations due to adverse effects, contraindications, or insufficient relief. This block offers a targeted, opiate-sparing technique that can provide rapid and sustained analgesia.[9] Administered under ultrasound guidance, this procedure has demonstrated high success rates, minimal complications, and significant reductions in pain scores and morphine use.[10][11] By targeting the femoral, lateral femoral cutaneous, and obturator nerves—often with minimal risk of motor blockade—it reduces reliance on systemic opioids, thereby minimizing complications such as respiratory depression, delirium, and constipation, especially in elderly or medically fragile patients. This block is especially valuable for older adults with comorbidities, in whom systemic analgesics may carry added risk. Useful in preoperative, intraoperative, and postoperative settings, it improves patient comfort, mobility, and rehabilitation participation while supporting enhanced recovery protocols. The ultrasound-guided approach increases accuracy, decreases complication rates, and allows use in settings ranging from the emergency department to perioperative care, making it a versatile tool in multimodal analgesia strategies.
Enhancing Healthcare Team Outcomes
Delivering high-quality, patient-centered care with ultrasound-guided fascia iliaca compartment block requires a blend of technical expertise, strategic planning, and interprofessional collaboration. Physicians and advanced practitioners must possess strong ultrasound interpretation skills, precise needle placement techniques, and the ability to adapt their approach to varied patient anatomies and clinical situations. Nurses play a pivotal role in preparing the patient, assisting with sterile technique, and providing real-time monitoring of vitals and comfort throughout the procedure. Pharmacists contribute by guiding local anesthetic selection, dose optimization, and ensuring compatibility with the patient’s comorbidities and concurrent medications. The shared strategy centers on integrating the fascia iliaca compartment block into multimodal pain management protocols, thereby reducing opioid reliance, minimizing systemic side effects, and improving mobility outcomes, particularly in older adults with hip fractures or other lower extremity injuries.
Effective interprofessional communication is critical at every stage—from initial patient assessment to post-procedure monitoring—to ensure safety, consistency, and efficiency. Structured pre-procedure briefings and postprocedure debriefings enhance clarity, anticipate potential complications, and streamline workflow. Clear handoff communication ensures that all team members are aware of the block’s administration, expected analgesic duration, and any follow-up assessments needed. Coordinated care planning allows timely mobilization, rehabilitation, and discharge, directly impacting patient satisfaction and recovery trajectories. When executed with skill and teamwork, ultrasound-guided fascia iliaca compartment block not only delivers superior analgesia but also exemplifies high-functioning, collaborative care that prioritizes patient outcomes and safety. Educating clinical staff on procedural techniques, safety protocols, and contraindications fosters improved patient safety, faster recovery, and enhanced team performance in the management of acute lower extremity pain.[12]
Media
(Click Image to Enlarge)
References
Godoy Monzon D, Iserson KV, Vazquez JA. Single fascia iliaca compartment block for post-hip fracture pain relief. The Journal of emergency medicine. 2007 Apr:32(3):257-62 [PubMed PMID: 17394987]
Stevens M, Harrison G, McGrail M. A modified fascia iliaca compartment block has significant morphine-sparing effect after total hip arthroplasty. Anaesthesia and intensive care. 2007 Dec:35(6):949-52 [PubMed PMID: 18084988]
Level 1 (high-level) evidenceFoss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, Hougaard S, Kehlet H. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007 Apr:106(4):773-8 [PubMed PMID: 17413915]
Level 1 (high-level) evidenceHaines L, Dickman E, Ayvazyan S, Pearl M, Wu S, Rosenblum D, Likourezos A. Ultrasound-guided fascia iliaca compartment block for hip fractures in the emergency department. The Journal of emergency medicine. 2012 Oct:43(4):692-7. doi: 10.1016/j.jemermed.2012.01.050. Epub 2012 Apr 9 [PubMed PMID: 22494596]
Senthil KS, Kumar P, Ramakrishnan L. Comparison of Pericapsular Nerve Group Block versus Fascia Iliaca Compartment Block as Postoperative Pain Management in Hip Fracture Surgeries. Anesthesia, essays and researches. 2021 Oct-Dec:15(4):352-356. doi: 10.4103/aer.aer_119_21. Epub 2022 Mar 1 [PubMed PMID: 35422548]
Ying H, Chen L, Yin D, Ye Y, Chen J. Efficacy of pericapsular nerve group block vs. fascia iliaca compartment block for Hip surgeries: A systematic review and meta-analysis. Frontiers in surgery. 2023:10():1054403. doi: 10.3389/fsurg.2023.1054403. Epub 2023 Feb 10 [PubMed PMID: 36843984]
Level 1 (high-level) evidenceHøgh A, Dremstrup L, Jensen SS, Lindholt J. Fascia iliaca compartment block performed by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies in trauma and limb reconstruction. 2008 Sep:3(2):65-70. doi: 10.1007/s11751-008-0037-9. Epub 2008 Sep 2 [PubMed PMID: 18762870]
Dochez E, van Geffen GJ, Bruhn J, Hoogerwerf N, van de Pas H, Scheffer G. Prehospital administered fascia iliaca compartment block by emergency medical service nurses, a feasibility study. Scandinavian journal of trauma, resuscitation and emergency medicine. 2014 Jun 23:22():38. doi: 10.1186/1757-7241-22-38. Epub 2014 Jun 23 [PubMed PMID: 24957807]
Level 2 (mid-level) evidenceGasanova I, Alexander JC, Estrera K, Wells J, Sunna M, Minhajuddin A, Joshi GP. Ultrasound-guided suprainguinal fascia iliaca compartment block versus periarticular infiltration for pain management after total hip arthroplasty: a randomized controlled trial. Regional anesthesia and pain medicine. 2019 Feb:44(2):206-211. doi: 10.1136/rapm-2018-000016. Epub [PubMed PMID: 30700615]
Level 1 (high-level) evidenceSivakumar RK, Panneerselvam S, Cherian A, Rudingwa P, Menon J. Perineural vs. intravenous dexmedetomidine as an adjunct to bupivacaine in ultrasound guided fascia iliaca compartment block for femur surgeries: A randomised control trial. Indian journal of anaesthesia. 2018 Nov:62(11):851-857. doi: 10.4103/ija.IJA_397_18. Epub [PubMed PMID: 30532320]
Level 1 (high-level) evidenceMa YH, Wu J, Jia B, Xue JX, Wang TL. [Continuous fascia iliaca compartment block combined with oral analgesics for pre-operative pain control in elderly hip fracture patients]. Zhonghua yi xue za zhi. 2018 Mar 13:98(10):723-727. doi: 10.3760/cma.j.issn.0376-2491.2018.10.002. Epub [PubMed PMID: 29562394]
Aluisio AR, Teicher C, Wiskel T, Guy A, Levine A. Focused Training for Humanitarian Responders in Regional Anesthesia Techniques for a Planned Randomized Controlled Trial in a Disaster Setting. PLoS currents. 2016 Nov 16:8():. pii: ecurrents.dis.e75f9f9d977ac8adededb381e3948a04. doi: 10.1371/currents.dis.e75f9f9d977ac8adededb381e3948a04. Epub 2016 Nov 16 [PubMed PMID: 28018749]
Level 1 (high-level) evidence