Introduction
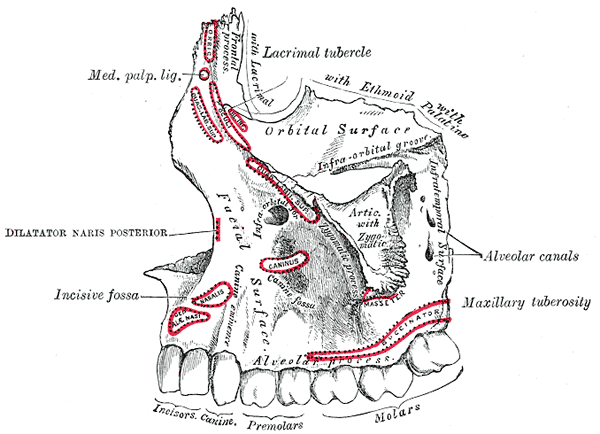
The right and left maxillary bones fuse at the midline to form the maxilla, a midfacial structure that supports the viscerocranium, the set of bones forming the facial skeleton. The maxilla is a paired, pyramidal bone composed of a body and 4 processes: alveolar, frontal, zygomatic, and palatine (see Image. Left Maxilla and Upper Jaw).[1] This bone contributes to the formation of the oral and nasal cavities and the orbit, and it houses the upper teeth (see Image. Lateral and Frontal Views of the Maxilla).[2][3] Forces generated during mastication are transmitted to the cranium through the frontal and zygomatic processes. The maxillary sinus, the most voluminous of the paranasal sinuses, lies within the body of the maxilla.
Injury to the maxilla can disrupt mastication, speech, and respiration. Surgical access to this bone requires careful navigation around the orbit, nasal cavity, and paranasal sinuses, underscoring its relevance in reconstructive and orthognathic procedures. Familiarity with maxillary anatomy and function allows clinicians to localize pathology, guide intervention, and minimize complications.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The maxillary bone articulates superiorly with the frontal bone, laterally with the zygomatic bone, and posteriorly with the palatine bone. Inferiorly, the alveolar process anchors the upper teeth.[4] Anteriorly, the maxilla forms the inferior and lateral margins of the pyriform aperture and articulates medially with the nasal bones along the anterior border of the frontal process.
Body
The body of the maxilla is pyramidal and houses the maxillary sinus, the largest among the paranasal sinuses. This segment has 4 surfaces, anterior, posterior, superior, and medial, each with distinct anatomical landmarks (see Table 1. Anatomical Features of the Maxillary Body).
Table 1. Anatomical Features of the Maxillary Body
|
Surface |
Location |
Anatomical Features |
|
Anterior |
Faces forward; forms the facial surface of the maxilla |
Infraorbital foramen: Below the infraorbital margin; transmits the infraorbital nerve and vessels |
|
Canine eminence: Prominence corresponding to the root of the maxillary canine |
||
|
Incisive fossa: Lies medial to the canine eminence |
||
|
Canine fossa: Depression lateral to the canine eminence |
||
|
Anterior nasal spine: Midline projection at the base of the nasal aperture |
||
|
Nasal notch: Forms part of the lateral boundary of the piriform aperture |
||
|
Posterior |
Faces backward and slightly laterally; forms the anterior wall of the infratemporal fossa |
Maxillary tuberosity: Rounded prominence behind the last molar; attachment site for the medial pterygoid muscle |
|
Posterior superior alveolar canals: Openings for nerves and vessels to molars and the maxillary sinus |
||
|
Superior |
Faces upward; forms most of the floor of the orbit |
Infraorbital groove: Starts at the posterior part of the orbital surface |
|
Infraorbital canal: Continuation of the groove, ending at the infraorbital foramen |
||
|
Orbital margin: Forms part of the inferior orbital rim |
||
|
Medial |
Faces medially; forms part of the lateral wall of the nasal cavity |
Greater palatine canal: Transmits palatine nerves and vessels |
|
Lacrimal groove: Groove for the nasolacrimal duct |
||
|
Conchal crest: Articulates with the inferior nasal concha |
Alveolar Process
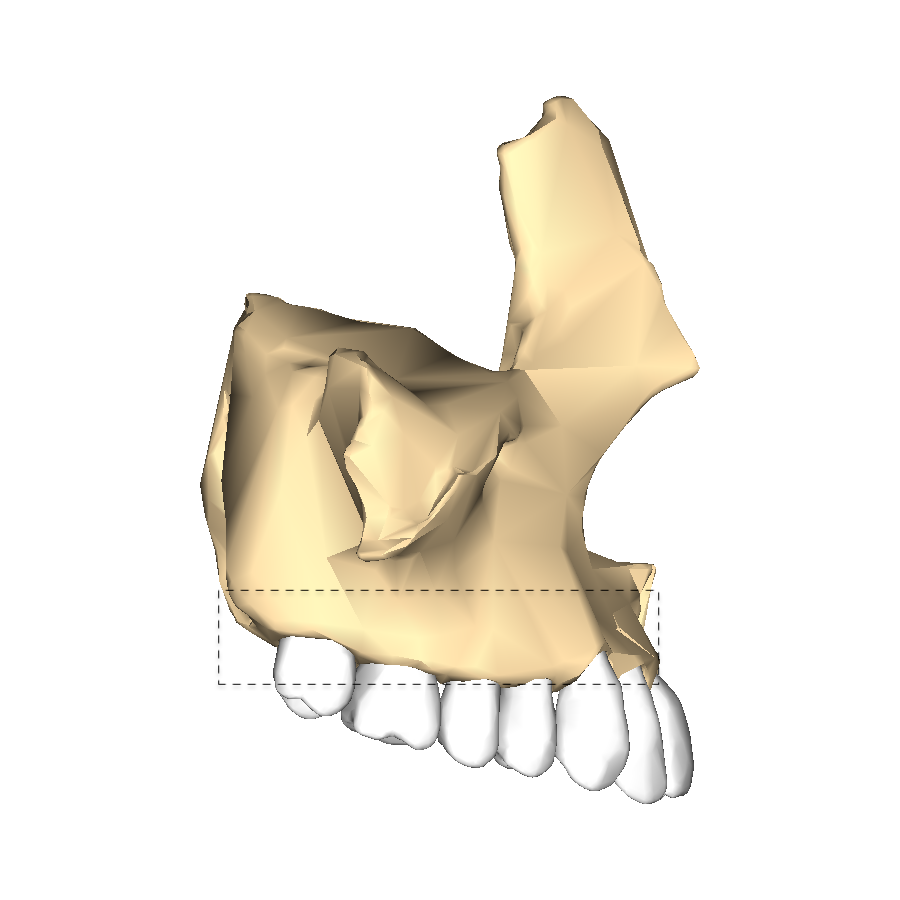
The alveolar process is horseshoe-shaped, curving anteriorly. This structure occupies the most inferior plane, situated below the hard palate, and extends posteriorly beneath the maxillary sinuses, terminating at the maxillary tuberosity (see Image. Alveolar Process of the Maxilla). The alveolar arteries and nerves and the periodontal ligament pass through channels within the alveolar process to vascularize, innervate, and anchor the upper teeth.[5] Tooth roots are embedded in alveoli, the bony sockets within this process.
Palatine Process
The palatine process is a thick, horizontal projection that forms 2/3 of the hard palate and the floor of the nasal cavity. Fusion of the right and left maxillary bones occurs at the midline through the palatine processes, forming the median maxillary suture (see Image. Palatine Process of the Maxilla). The palatine process also contributes to the anterior nasal floor and the inferior margin of the pyriform aperture.
The incisive canal, located in the anterior hard palate, connects the nasal and oral cavities and transmits the nasopalatine nerve and sphenopalatine artery. A small mucosal protrusion, the incisive papilla, overlies the opening (see Image. Inferior View of the Maxilla).[6] Anterior extension of the palatine process contributes to the formation of the anterior nasal spine.
Zygomatic Process
The zygomatic process projects laterally from the maxilla, forming the superolateral border of the maxillary sinus. This structure lies above the 1st maxillary molar and articulates inferiorly with the alveolar process and superomedially with the frontal process (see Image. Zygomatic Process of the Maxilla). The zygomatic process reinforces the structural integrity of the midface together with the alveolar process.[7]
Laterally, the zygomatic process articulates with the zygomatic bone and defines the malar eminence and facial width. On the anterior surface, lateral to the zygomatic process and medial to the pyriform aperture, is the canine fossa, a depression on the anterior aspect of the maxilla.[8] The zygomaticoalveolar crest, located inferior to the zygomatic process and superior to the alveolar process, forms another depression and serves as a reference point in the classification of maxillary fractures.
Frontal Process
The frontal process extends superiorly and medially from the body of the maxillary bone (see Image. Frontal Process of the Maxilla). Articulation occurs superiorly with the frontal bone and medially with the nasal bones. The frontal process forms the anterior wall of the nasolacrimal groove. Structural contributions to the central and inferior portion of the forehead and nasal bridge arise from articulations of the frontal process with the frontal and nasal bones.[9][10]
Maxillary Sinus
The hollow body of the maxilla encloses the maxillary sinus, the largest of all paranasal sinuses, with an adult volume of approximately 15 mL.[11][12] A pyramidal shape mirrors that of the maxilla itself, with the base formed by the medial wall facing the lateral nasal wall and the apex directed laterally toward the zygomatic arch. The sinus spans from the premolar region anteriorly to the level of the 3rd molar posteriorly.
The roof of the sinus contributes to the orbital floor and houses the infraorbital canal, which transmits the infraorbital neurovascular bundle. This bundle exits the skull through the infraorbital foramen, located approximately 1 cm below the infraorbital rim.[13] The floor of the sinus lies just superior to the alveolar process and often approaches the roots of the molars. The lowest point is typically near the 1st molar. Vertical position varies with age, ranging from level with the nasal floor to approximately 1 cm below it.
The medial wall forms part of the lateral nasal wall and contains 2 key structures. The maxillary sinus ostium, located anterosuperiorly, drains into the ethmoid infundibulum and opens into the middle meatus of the nasal cavity. The nasolacrimal duct, originating in the medial orbital wall, descends through the anterior maxillary sinus and drains into the inferior meatus of the nasal cavity.
Anatomical variants may include extension of the sinus toward the zygomatic process superolaterally or the maxillary tuberosity inferolaterally. Other variations include hypoplasia, antral septation dividing the cavity, or bony exostoses.[14]
Embryology
Maxillofacial development begins in the 4th week of gestation, with the formation of 5 facial prominences around the stomodeum, the primordial mouth and topographical center of the face.[15] Contributions from the 1st pharyngeal arch and neural crest cells give rise to the 5 prominences: paired maxillary, paired mandibular, and the frontonasal prominence.[15][16][17] The stomodeum is bordered cranially by the frontonasal prominence, laterally by the maxillary prominence, and inferolaterally by the mandibular prominence. The maxillary prominences develop into the secondary palate, most of the maxilla, and the lateral upper lip (see Image. Anterior Surface of the Maxilla at Birth).[18][19]
By the end of the 4th week, the lower portion of the frontonasal prominence gives rise to the nasal placodes, which divide into paired medial and lateral nasal processes, separated by the nasal groove. At the end of the 6th week, the medial nasal processes fuse to form the philtrum. At the end of the 8th week, fusion of the medial nasal and maxillary processes forms the intermaxillary segment, which gives rise to the upper lip and the primary palate. Formation of the primary palate occurs through a deeper portion of the intermaxillary segment known as the median palatine process. The lateral nasal processes become the nasal alae.
Development of the secondary palate begins during the 6th week of gestation. Outgrowths of the maxillary processes, known as palatal shelves, initially grow vertically on either side of the tongue. By the 7th week, the shelves assume a horizontal orientation as mandibular elongation and tongue descent create sufficient space. Midline fusion of the palatal shelves forms the secondary palate and continues anteriorly with the primary palate and superiorly with the nasal septum. Replacement of palatal mesenchyme with muscle and bone follows, differentiating into the hard and soft palate. Posterior development of the nasopalatine canal results in the formation of the incisive canal at the junction between the primary and secondary palates. Completion of palatal fusion occurs by the 10th week, with full anatomical formation achieved by the 12th week of embryonic development.
Blood Supply and Lymphatics
Arterial supply to the maxilla arises primarily from branches of the maxillary artery, a terminal branch of the external carotid artery. This vessel originates posterior to the mandibular ramus and enters the pterygopalatine fossa, terminating as the pterygopalatine artery. Three segments characterize the maxillary artery: mandibular, pterygoid, and pterygopalatine.
The pterygopalatine segment serves as the principal source of blood supply to the maxilla. This segment gives rise to the posterior superior alveolar, infraorbital, descending palatine, and sphenopalatine arteries. The posterior superior alveolar artery supplies the maxillary molars, the associated gingiva, and the maxillary sinus. The infraorbital artery provides vascular supply to the lacrimal sac, upper anterior teeth, and sinus mucosa.
Further branches of the descending palatine artery, the greater and lesser palatine arteries, vascularize the hard and soft palate, the pharyngeal wall, and the palatine tonsils. The sphenopalatine artery supplies the lateral nasal wall, the nasal septum, and the conchae.[20][21][22]
Nerves
Innervation of the maxilla occurs through the maxillary nerve, the 2nd division of the trigeminal nerve, the 5th and largest cranial nerve.[23][24] The trigeminal nerve originates at the trigeminal ganglion and functions primarily as a sensory nerve.
After exiting the cranium via the foramen rotundum, the maxillary nerve enters the pterygopalatine fossa and gives rise to multiple branches. Sensory input to maxillary structures is conveyed by the infraorbital (ION), posterior superior alveolar (PSA), middle superior alveolar (MSA), anterior superior alveolar (ASA), palatine, and nasopalatine (NPN) nerves.
The ION, a direct continuation of the maxillary nerve, courses anteriorly through the infraorbital canal, where the MSA and ASA nerves emerge to innervate the upper anterior teeth and premolars. Additional branches supply the superior and medial walls of the maxillary sinus. Upon exiting via the infraorbital foramen, the nerve distributes sensory fibers to the lower eyelid, nose, cheek, and upper lip.
Three superior alveolar nerves—posterior, middle, and anterior—contribute to the innervation of the upper dentition and maxillary sinus. The PSA nerve arises in the pterygopalatine fossa before the maxillary nerve enters the infraorbital canal. This nerve descends along the maxillary tuberosity and enters the posterior superior alveolar foramina on the infratemporal surface of the maxilla, supplying the maxillary molars and posterior wall of the maxillary sinus. Branches from the PSA nerve anastomose with the MSA and ASA nerves to form the superior dental plexus.
The MSA nerve branches from the ION within the infraorbital canal and courses along the posterolateral wall of the maxillary sinus to innervate the premolars and contribute to posterior sinus wall sensation. The ASA nerve arises from the anterior 3rd of the ION and descends through the anterior wall of the maxilla, innervating the maxillary incisors, the anterior wall of the maxillary sinus, and the lateral nasal wall.
The palatine nerve arises from the sphenopalatine ganglion and divides into the greater palatine (GPN) and lesser palatine (LPN) nerves. The GPN, the anterior division, exits the greater palatine foramen opposite the 3rd molar and innervates the hard palate and palatal gingiva. In addition to palatal innervation, the GPN also supplies the inferior wall and ostium of the maxillary sinus.
The NPN also originates from the sphenopalatine ganglion. Entry into the nasal cavity occurs through the sphenopalatine foramen, followed by a course along the nasal roof, providing innervation to the roof and septum. The nerve then descends along the nasal septum, enters the canal of Stensen, and traverses the incisive canal to reach the anterior hard palate via the incisive foramen. Innervation is directed to the palatal mucosa and palatal gingiva adjacent to the canine teeth.[25]
Table 2. Sensory Innervation of the Maxilla
|
Nerve |
Origin and Pathway |
Innervation |
|
ION |
A direct extension of the maxillary nerve (cranial nerve V2) Gives rise to the MSA and ASA nerves and exits via the infraorbital foramen |
Innervates the upper teeth, maxillary sinus, lower eyelid, nose, cheek, and upper lip |
|
PSA |
Emerges in the pterygopalatine fossa Branches directly from the maxillary nerve |
Innervates the maxillary molars and the posterior portion of the maxillary sinus |
|
MSA |
Branch of the ION |
Innervates the premolars and the posterolateral wall of the maxillary sinus |
|
ASA |
Branch of the ION |
Innervates the incisors, the anterior wall of the maxillary sinus, and the lateral nasal wall |
|
Palatine |
Branches from the sphenopalatine ganglion |
The GPN innervates the hard palate and lower wall of the maxillary sinus. The LPN innervates the soft palate. |
|
NPN |
Branch of the sphenopalatine ganglion |
Innervates the nasal septum and anterior hard palate via the incisive foramen |
Muscles
Muscles of the midface include the nasalis, levator labii superioris alaeque nasi (LLSAN), levator labii superioris (LLS), zygomaticus minor, zygomaticus major, levator anguli oris (LAO), buccinator, and orbicularis oris. Among these muscles, only the nasalis, LLSAN, LLS, and LAO originate from the maxilla. All midfacial muscles receive motor innervation from the facial nerve.
The nasalis arises from the maxilla and lateral nasal sidewall, sending fibers across the nasal dorsum to meet the contralateral muscle. Contraction of the nasalis dilates the nostrils during deep inspiration. The LLSAN originates from the upper frontal process of the maxilla and extends inferiorly to insert into the orbicularis oris, contributing to lip eversion, nasal ala dilation, and accentuation of the nasolabial fold. The LLS originates near the infraorbital foramen on the inferior orbital margin and inserts into the orbicularis oris, functioning primarily to evert the upper lip and deepen the nasolabial fold. The LAO arises from the canine fossa and inserts at the modiolus, the muscular convergence at the oral commissure. Contracting this muscle elevates the commissure, participates in smiling, and influences the position of the nasolabial fold.[26]
Surgical Considerations
Blood Supply
The infraorbital and posterior superior alveolar arteries form an arterial arcade surrounding the maxillary sinus. Careful planning is required during surgical procedures involving the maxilla, especially sinus or dental interventions, to avoid arterial injury and minimize bleeding. A detailed understanding of maxillary artery anatomy is also essential in the management of posterior epistaxis, which accounts for approximately 5% of epistaxis cases. Targeted treatment may involve endoscopic ligation or electrocauterization of the sphenopalatine and palatine arteries to control persistent bleeding.
Nerves
The superior alveolar nerves provide sensory innervation to the mucosa and walls of the maxillary sinus. The anatomical course of these nerves creates an anterior zone, particularly near the canine fossa, where bone removal may be performed with minimal risk of nerve injury. This region is critical during the Caldwell-Luc procedure, which accesses the maxillary sinus through the anterior wall to treat chronic sinusitis or remove pathological tissue.[27]
Lymphatics
Sentinel lymph node biopsy plays a pivotal role in staging and guiding the treatment of oral maxillary cancers. The first echelon of lymphatic drainage typically involves cervical lymph nodes in levels I to III, though the parapharyngeal nodes may also be involved in select cases.[28]
Clinical Significance
Detailed knowledge of maxillary anatomy is essential when addressing midface trauma. The Le Fort classification system, introduced by René Le Fort in 1901, is the standard framework for describing midfacial fracture patterns. This system outlines 3 principal types of fractures based on predictable lines of weakness in the facial skeleton.
Le Fort I fractures involve a horizontal separation of the maxilla. The fracture extends posteriorly from the pyriform aperture, traversing the zygomaticoalveolar crest and maxillary tuberosities, and terminates in the pterygopalatine fossa. This pattern effectively detaches the hard palate and alveolar process from the midfacial skeleton.
Le Fort II fractures follow a pyramidal pattern. The fracture originates at the nasofrontal suture, extends through the frontomaxillary suture and orbital floor, and passes through the maxillary sinus. Inferiorly, the fracture reaches the zygomaticoalveolar crest bilaterally and continues caudally through the maxillary tuberosities into the pterygoid processes. Superiorly, the fracture extends through the nasal septum. This pattern separates the maxilla, nasal bones, and septum from both the cranial base and the lateral midface.
Le Fort III fractures are complete craniofacial dissociation. The fracture begins at the nasofrontal suture and extends through the medial orbital wall and floor to the inferior orbital fissure. The bone disruption continues laterally through the zygomaticofrontal suture and descends bilaterally through the zygomatic arches. From the nasofrontal region, the fracture also extends caudally through the ethmoid bone and the perpendicular plate of the palatine bone, involving the pterygoid process and vomer, and terminates in the palatine fossa. This pattern results in the complete separation of the facial skeleton from the cranial base.
Implant placement in the posterior maxilla poses unique challenges due to its anatomical complexity. This region is characterized by proximity to the maxillary sinus, wide extraction sockets, multirooted teeth, and a higher risk of socket wall compromise. Additionally, the predominance of trabecular bone in the posterior maxilla results in lower bone density, which can impair primary implant stability and affect long-term success.[29] Effective surgical planning requires a detailed understanding of these anatomical constraints to minimize procedural risks and optimize outcomes.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
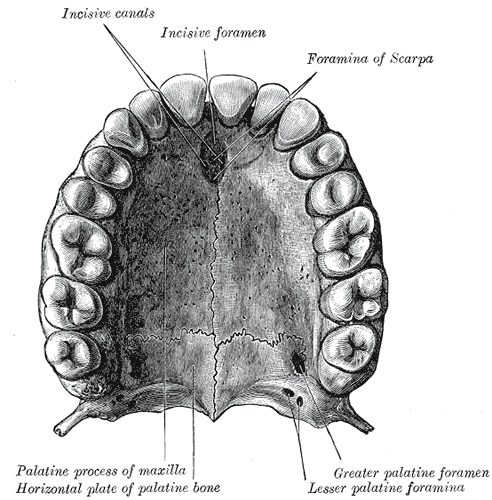
Inferior View of the Maxilla. The illustration shows the palatine process, horizontal plate of the palatine bone, alveolar arch, and associated foramina, including the incisive, Scarpa, greater palatine, and lesser palatine foramina, as well as the incisive canals.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
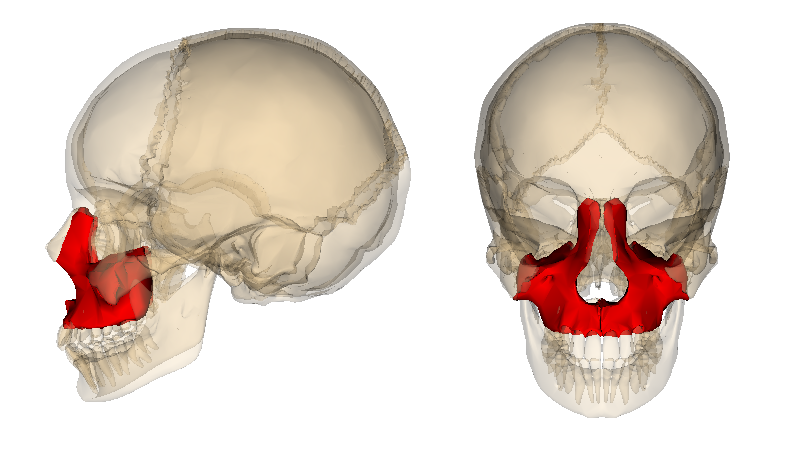
Lateral and Frontal Views of the Maxilla. The maxilla is highlighted in red on these skulls. The left image shows the lateral view of the left maxilla. The right image shows the frontal view.
Wikimedia commons. Public Domain. https://commons.wikimedia.org/wiki/File:Maxilla_image.png#/media/File:Maxilla_image.png
(Click Image to Enlarge)
(Click Image to Enlarge)
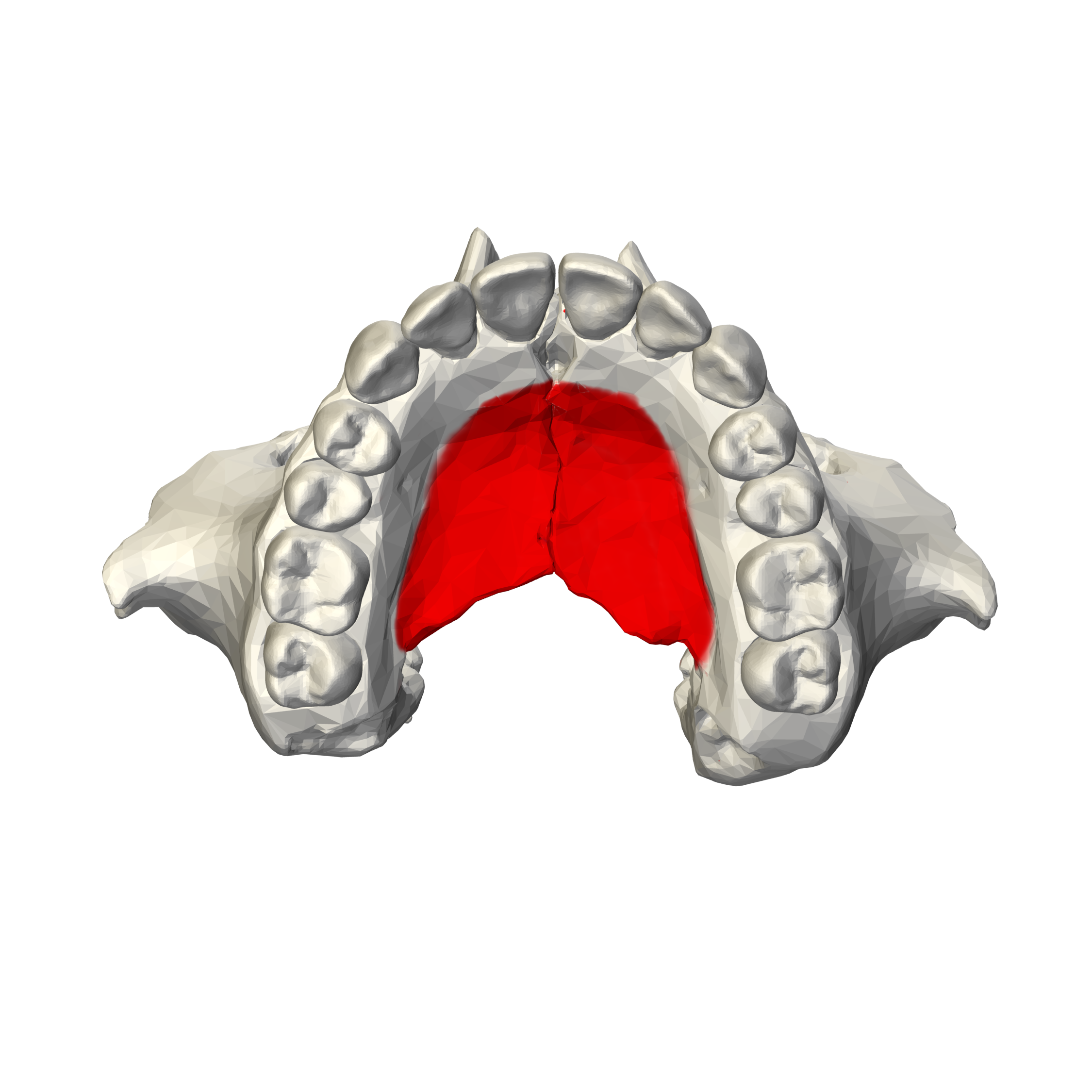
Palatine Process of the Maxilla. Inferior view of the skull highlighting the palatine process in red. This bony plate forms the anterior portion of the hard palate and contributes to the floor of the nasal cavity.
By Polygon. Data were generated by Database Center for Life Science(DBCLS)[2]. - Polygon data are from BodyParts3D[1], CC BY-SA 2.1 jp, https://commons.wikimedia.org/w/index.php?curid=33259893
(Click Image to Enlarge)

Zygomatic Process of the Maxilla. A portion of the skull is shaded in red to highlight the zygomatic process. This lateral projection forms part of the zygomaticomaxillary complex near the cheek.
By Polygon. Data were generated by Database Center for Life Science(DBCLS)[2]. - Polygon data are from BodyParts3D[1], CC BY-SA 2.1 jp, https://commons.wikimedia.org/w/index.php?curid=33227060
(Click Image to Enlarge)

Frontal Process of the Maxilla. A red-shaded portion of the skull highlights the frontal process. This vertical projection ascends medially to articulate with the frontal and nasal bones.
By Polygon. Data were generated by Database Center for Life Science(DBCLS)[2]. - Polygon data are from BodyParts3D[1], CC BY-SA 2.1 jp, https://commons.wikimedia.org/w/index.php?curid=33174192
References
Okay DJ, Genden E, Buchbinder D, Urken M. Prosthodontic guidelines for surgical reconstruction of the maxilla: a classification system of defects. The Journal of prosthetic dentistry. 2001 Oct:86(4):352-63 [PubMed PMID: 11677528]
Level 2 (mid-level) evidenceDalgorf D, Higgins K. Reconstruction of the midface and maxilla. Current opinion in otolaryngology & head and neck surgery. 2008 Aug:16(4):303-11. doi: 10.1097/MOO.0b013e328304b426. Epub [PubMed PMID: 18626247]
Level 3 (low-level) evidenceKühnel TS, Reichert TE. Trauma of the midface. GMS current topics in otorhinolaryngology, head and neck surgery. 2015:14():Doc06. doi: 10.3205/cto000121. Epub 2015 Dec 22 [PubMed PMID: 26770280]
Chen HS, Hsiao SY, Lee KT. Analysis of Facial Skeletal Morphology: Nasal Bone, Maxilla, and Mandible. BioMed research international. 2021:2021():5599949. doi: 10.1155/2021/5599949. Epub 2021 May 24 [PubMed PMID: 34124250]
Saffar JL, Lasfargues JJ, Cherruau M. Alveolar bone and the alveolar process: the socket that is never stable. Periodontology 2000. 1997 Feb:13():76-90 [PubMed PMID: 9567924]
Level 3 (low-level) evidenceLake S, Iwanaga J, Kikuta S, Oskouian RJ, Loukas M, Tubbs RS. The Incisive Canal: A Comprehensive Review. Cureus. 2018 Jul 30:10(7):e3069. doi: 10.7759/cureus.3069. Epub 2018 Jul 30 [PubMed PMID: 30280065]
Sadrameli M, Mupparapu M. Oral and Maxillofacial Anatomy. Radiologic clinics of North America. 2018 Jan:56(1):13-29. doi: 10.1016/j.rcl.2017.08.002. Epub 2017 Oct 10 [PubMed PMID: 29157543]
Bentsianov B, Blitzer A. Facial anatomy. Clinics in dermatology. 2004 Jan-Feb:22(1):3-13 [PubMed PMID: 15158538]
Danesh-Sani SA, Loomer PM, Wallace SS. A comprehensive clinical review of maxillary sinus floor elevation: anatomy, techniques, biomaterials and complications. The British journal of oral & maxillofacial surgery. 2016 Sep:54(7):724-30. doi: 10.1016/j.bjoms.2016.05.008. Epub 2016 May 25 [PubMed PMID: 27235382]
Ogle OE, Weinstock RJ, Friedman E. Surgical anatomy of the nasal cavity and paranasal sinuses. Oral and maxillofacial surgery clinics of North America. 2012 May:24(2):155-66, vii. doi: 10.1016/j.coms.2012.01.011. Epub 2012 Mar 2 [PubMed PMID: 22386856]
Valenzuela-Fuenzalida JJ, Baez-Flores B, Sepúlveda RÁ, Medina CM, Pérez R, López E, Sanchis J, Orellana Donoso M, Silva JL, Rodriguez MC, Iwanaga J. Anatomical variations and abnormalities of the maxillary region and clinical implications: A systematic review and metaanalysis. Medicine. 2023 Sep 22:102(38):e34510. doi: 10.1097/MD.0000000000034510. Epub [PubMed PMID: 37747000]
Level 1 (high-level) evidenceWhyte A, Boeddinghaus R. The maxillary sinus: physiology, development and imaging anatomy. Dento maxillo facial radiology. 2019 Dec:48(8):20190205. doi: 10.1259/dmfr.20190205. Epub 2019 Aug 13 [PubMed PMID: 31386556]
Haghnegahdar A, Khojastepour L, Naderi A. Evaluation of Infraorbital Canal in Cone Beam Computed Tomography of Maxillary Sinus. Journal of dentistry (Shiraz, Iran). 2018 Mar:19(1):41-47 [PubMed PMID: 29492415]
Lozano-Carrascal N, Salomó-Coll O, Gehrke SA, Calvo-Guirado JL, Hernández-Alfaro F, Gargallo-Albiol J. Radiological evaluation of maxillary sinus anatomy: A cross-sectional study of 300 patients. Annals of anatomy = Anatomischer Anzeiger : official organ of the Anatomische Gesellschaft. 2017 Nov:214():1-8. doi: 10.1016/j.aanat.2017.06.002. Epub 2017 Jul 29 [PubMed PMID: 28759740]
Level 2 (mid-level) evidenceWilson DB. Embryonic development of the head and neck: Part 3, The face. Head & neck surgery. 1979 Nov-Dec:2(2):145-53 [PubMed PMID: 264107]
Trevizan M, Consolaro A. Premaxilla: an independent bone that can base therapeutics for middle third growth! Dental press journal of orthodontics. 2017 Mar-Apr:22(2):21-26. doi: 10.1590/2177-6709.22.2.021-026.oin. Epub [PubMed PMID: 28658352]
Baxter DJ, Shroff MM. Developmental maxillofacial anomalies. Seminars in ultrasound, CT, and MR. 2011 Dec:32(6):555-68. doi: 10.1053/j.sult.2011.06.004. Epub [PubMed PMID: 22108218]
Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet (London, England). 2009 Nov 21:374(9703):1773-85. doi: 10.1016/S0140-6736(09)60695-4. Epub 2009 Sep 9 [PubMed PMID: 19747722]
Shkoukani MA, Lawrence LA, Liebertz DJ, Svider PF. Cleft palate: a clinical review. Birth defects research. Part C, Embryo today : reviews. 2014 Dec:102(4):333-42. doi: 10.1002/bdrc.21083. Epub 2014 Dec 10 [PubMed PMID: 25504820]
Alvernia JE, Hidalgo J, Sindou MP, Washington C, Luzardo G, Perkins E, Nader R, Mertens P. The maxillary artery and its variants: an anatomical study with neurosurgical applications. Acta neurochirurgica. 2017 Apr:159(4):655-664. doi: 10.1007/s00701-017-3092-5. Epub 2017 Feb 13 [PubMed PMID: 28191601]
Tanoue S, Kiyosue H, Mori H, Hori Y, Okahara M, Sagara Y. Maxillary artery: functional and imaging anatomy for safe and effective transcatheter treatment. Radiographics : a review publication of the Radiological Society of North America, Inc. 2013 Nov-Dec:33(7):e209-24. doi: 10.1148/rg.337125173. Epub [PubMed PMID: 24224604]
Otake I, Kageyama I, Mataga I. Clinical anatomy of the maxillary artery. Okajimas folia anatomica Japonica. 2011 Feb:87(4):155-64 [PubMed PMID: 21516980]
Walker HK, Hall WD, Hurst JW, Walker HK. Cranial Nerve V: The Trigeminal Nerve. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250225]
McKay GS. Commentary on paper: "A review of the mandibular and maxillary nerve supplies and their clinical relevance". Archives of oral biology. 2012 Apr:57(4):321-2. doi: 10.1016/j.archoralbio.2011.11.021. Epub 2011 Dec 20 [PubMed PMID: 22192853]
Level 3 (low-level) evidenceRodella LF, Buffoli B, Labanca M, Rezzani R. A review of the mandibular and maxillary nerve supplies and their clinical relevance. Archives of oral biology. 2012 Apr:57(4):323-34. doi: 10.1016/j.archoralbio.2011.09.007. Epub 2011 Oct 11 [PubMed PMID: 21996489]
Snider CC, Amalfi AN, Hutchinson LE, Sommer NZ. New Insights into the Anatomy of the Midface Musculature and its Implications on the Nasolabial Fold. Aesthetic plastic surgery. 2017 Oct:41(5):1083-1090. doi: 10.1007/s00266-017-0889-9. Epub 2017 May 15 [PubMed PMID: 28508263]
Datta RK, Viswanatha B, Shree Harsha M. Caldwell Luc Surgery: Revisited. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2016 Mar:68(1):90-3. doi: 10.1007/s12070-015-0883-y. Epub 2015 Jul 31 [PubMed PMID: 27066419]
Boeve K, Schepman KP, Vegt BV, Schuuring E, Roodenburg JL, Brouwers AH, Witjes MJ. Lymphatic drainage patterns of oral maxillary tumors: Approachable locations of sentinel lymph nodes mainly at the cervical neck level. Head & neck. 2017 Mar:39(3):486-491. doi: 10.1002/hed.24628. Epub 2016 Dec 22 [PubMed PMID: 28006085]
Alkhames HM, Ali RMM, Alzouri SS, Bayome M. Assessment of Posterior Maxillary Alveolar Bone for Immediate Implant Placement: A Quantitative and Qualitative Analysis. European journal of dentistry. 2024 Jul:18(3):877-882. doi: 10.1055/s-0043-1777049. Epub 2024 Feb 8 [PubMed PMID: 38331039]
Level 2 (mid-level) evidence