Definition/Introduction
Calcium is an essential mineral that supports key cellular functions, particularly in the nervous, cardiovascular, and musculoskeletal systems.[1] This mineral acts as a secondary messenger in intracellular signal transduction pathways and plays a critical role in action potential generation, neurotransmitter release, and enzyme activity.[2] Most of the calcium in the body is located in bones and teeth, whereas 1% to 2% circulates in serum, where it is primarily bound to serum proteins and other anions.[3] Severe derangements in calcium homeostasis can result in life-threatening pathology.[1] Prompt identification of such abnormalities through a detailed history, a physical examination, and laboratory testing facilitates timely patient treatment.
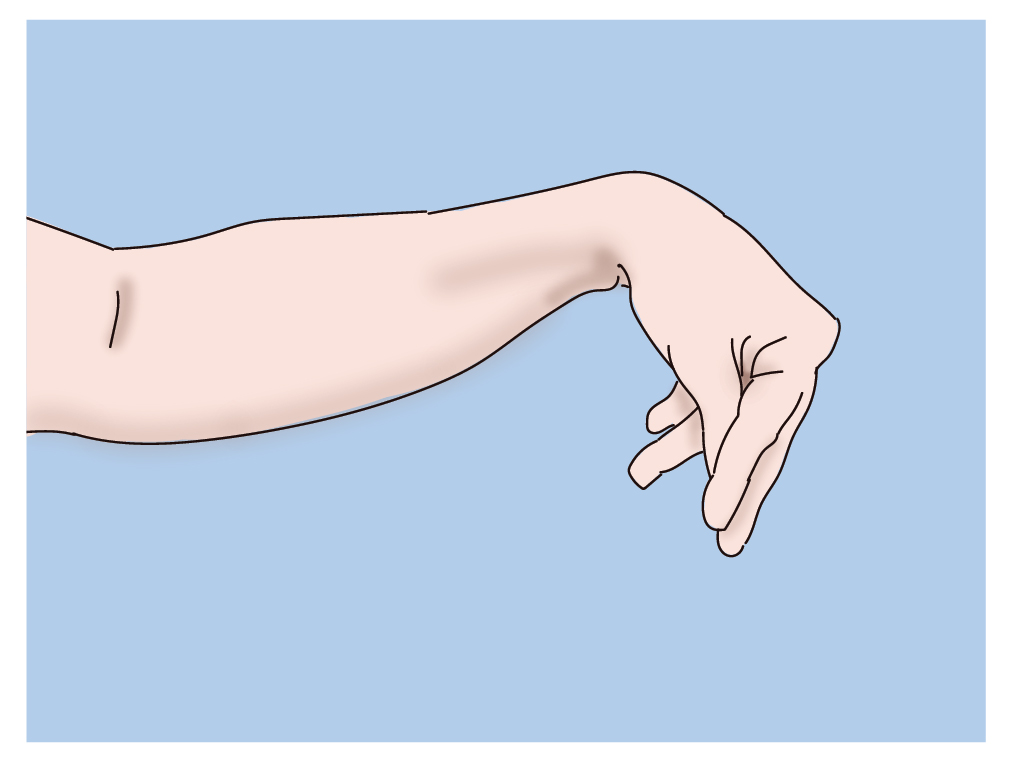
Hypocalcemia is associated with a state of neuromuscular excitability, which may be observed on physical examination. In 1861, French clinician Armand Trousseau first described the Trousseau sign of latent tetany. This sign is characterized by the occurrence of carpopedal spasms upon inflation of a sphygmomanometer cuff to 20 mmHg above a patient's systolic blood pressure for 2 to 3 minutes. The Trousseau sign is highly suggestive of hypocalcemia.[4] This sign typically manifests as flexion of the wrist and metacarpophalangeal joints, accompanied by hyperextension of the proximal and distal interphalangeal joints. This sign is also known as the main d'accoucheur ("hand of the obstetrician") due to its resemblance to a hand position used when delivering a baby. The Trousseau sign has also been observed in patients with hypomagnesemia, hypophosphatemia, and hypokalemia.[4][5]
The Trousseau sign of tetany should not be confused with Trousseau syndrome, a distinct condition characterized by recurrent, migratory superficial thrombophlebitis associated with underlying adenocarcinoma. Although both are named after Armand Trousseau, this activity focuses on the Trousseau sign of latent tetany and its clinical relevance.
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Hypocalcemia is associated with neuromuscular excitability, which may manifest as the Trousseau sign during a physical examination. Hypocalcemia lowers the depolarization threshold for neurons by increasing membrane permeability to sodium, thereby facilitating the easier firing of action potentials in response to stimuli. Inflation of a sphygmomanometer cuff above a patient's systolic blood pressure for several minutes causes ischemia of tissues distal to the cuff. As cellular ischemia also lowers neuronal depolarization thresholds, sustained arterial occlusion by the sphygmomanometer cuff further increases neuronal excitability. This increase promotes the discharge of action potentials that manifest as muscle spasms and tetany distal to the cuff.
The sensitivity and specificity of the Trousseau sign in hypocalcemia are reported to be 94% and 99%, respectively.[6][7] A positive sign has been noted in up to 1% to 4% of healthy individuals without hypocalcemia.[7]
Important confounders associated with a positive Trousseau sign must be noted. The Trousseau sign may also be observed in the setting of hypomagnesemia, hypophosphatemia, hypokalemia, and metabolic alkalosis, as these processes also lower the depolarization threshold for neurons.[4][8] Metabolic alkalosis promotes protein binding of ionized calcium, decreasing the concentration of free calcium in serum. In these cases, hypocalcemia is sometimes present concurrently. A positive Trousseau sign has also been observed intraoperatively during tourniquet placement, with subsequent carpopedal spasm, in patients with normal serum calcium levels and no noted hyperventilation, suggesting metabolic alkalosis as an etiology. Removal of the tourniquet resulted in the resolution of the carpal spasm.[4]
The Trousseau and Chovstek signs are often discussed together as physical examination findings associated with hypocalcemia. The Chvostek sign is elicited by mechanical stimulation in the location of the facial nerve, resulting in facial muscle spasms. The Trousseau sign is considered to be more specific for hypocalcemia. Similar to the Trousseau sign, the Chovstek sign may also be present in individuals with normal calcium levels.[9]
Clinical Significance
The Trousseau sign of latent tetany is associated with hypocalcemia. Low serum calcium has widespread effects on the body, some of which can be life-threatening. Neurologic and muscular manifestations include weakness, muscle spasms, tetany, paresthesias of the mouth and digits, confusion, hallucinations, and seizures. Cardiac involvement may manifest as QT prolongation with or without torsades de pointes, ventricular arrhythmias, and heart failure.[10][11] Patients may complain of nausea, vomiting, or constipation. Patients with chronic hypocalcemia may have dry or hyperpigmented skin, brittle hair, osteodystrophy, rickets, osteomalacia, dental degeneration, or cataracts. The identification of signs and symptoms of hypocalcemia should prompt the measurement of serum electrolytes, including calcium, and a workup for an underlying etiology if it is not already known.
The normal range for serum calcium is 8.5 to 10.5 mg/dL, with levels below 8.5 mg/dL indicating hypocalcemia. The most common causes of hypocalcemia are vitamin D deficiency or hypoparathyroidism.[12][13] Vitamin D deficiency may result from either a nutritional deficit or a deficiency of renal 1-alpha-hydroxylase, which converts vitamin D to its metabolically active form.[14] Hypoparathyroidism is most often a sequel of thyroidectomy, parathyroidectomy, or other radical neck surgery that damages or removes parathyroid tissue.[15] Removal of previously hyperactive parathyroid glands may result in hungry bone syndrome caused by osteoblast-mediated calcium, phosphate, and magnesium uptake that outpaces osteoclast-mediated bone resorption.[1] Hypoparathyroidism may also result from autoimmune destruction, genetic malformation, or infiltrative disease of parathyroid tissue. Acquired parathyroid gland insufficiency, calcitriol resistance, or vitamin D insufficiency can lead to hypocalcemia by disrupting the parathyroid-vitamin D axis.
Less common etiologies of hypocalcemia include various iatrogenic and systemic disease processes. Medications such as bisphosphonates, cisplatin, loop diuretics, phosphates, phenytoin, phenobarbital, glucocorticoids, rifampin, and omeprazole may lower serum calcium levels.[16] Chronic kidney disease, cancer with osteoblastic metastases, metabolic alkalosis, acute pancreatitis, pseudohypoparathyroidism, and pregnancy are associated with hypocalcemia. Sepsis may lead to hypocalcemia by disrupting the parathyroid-vitamin D axis.[14] Hypocalcemia may occur in the setting of hemorrhagic shock due to calcium chelation by sodium citrate, a preservative used in packed red blood cell units.[17] A similar process can occur in patients undergoing continuous renal replacement therapy, where citrate is commonly used as an anticoagulant, particularly in cases where traditional anticoagulants are contraindicated.[1] In both rhabdomyolysis and tumor lysis syndrome, serum calcium is bound to excessive phosphate ions released into the serum due to cell destruction, decreasing the level of free serum calcium.[18][19]
The treatment of hypocalcemia includes calcium supplementation along with addressing the underlying pathology. Concurrent electrolyte derangements should also be corrected. Empiric calcium administration is recommended for patients undergoing massive blood transfusions due to anticipated hypocalcemia.
Nursing, Allied Health, and Interprofessional Team Interventions
Vital signs are typically obtained at the beginning of a patient encounter, often by a nurse, certified nursing assistant, or medical assistant. The Trousseau sign may be first noted by the allied healthcare professional obtaining a patient's vital signs rather than by the clinician. Recognition and reporting of the sign to the patient's clinician may be the only opportunity for the issue to be addressed, particularly if a patient does not report other signs or symptoms concerning for hypocalcemia. When hypocalcemia is suspected, clinicians may consider eliciting the Trousseau sign, as it offers relatively high sensitivity and specificity for diagnosing the condition. All team members must be aware that the absence of the Trousseau sign does not exclude hypocalcemia and that other metabolic derangements may also cause this finding.
Media
(Click Image to Enlarge)
References
Murray SL, Wolf M. Calcium and Phosphate Disorders: Core Curriculum 2024. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2024 Feb:83(2):241-256. doi: 10.1053/j.ajkd.2023.04.017. Epub 2023 Dec 13 [PubMed PMID: 38099870]
Sukumaran P, Nascimento Da Conceicao V, Sun Y, Ahamad N, Saraiva LR, Selvaraj S, Singh BB. Calcium Signaling Regulates Autophagy and Apoptosis. Cells. 2021 Aug 18:10(8):. doi: 10.3390/cells10082125. Epub 2021 Aug 18 [PubMed PMID: 34440894]
Matikainen N, Pekkarinen T, Ryhänen EM, Schalin-Jäntti C. Physiology of Calcium Homeostasis: An Overview. Endocrinology and metabolism clinics of North America. 2021 Dec:50(4):575-590. doi: 10.1016/j.ecl.2021.07.005. Epub [PubMed PMID: 34774235]
Level 3 (low-level) evidenceBeecher SM, Bollard SM, Beausang ES. Idiopathic Carpal Spasm (Trousseau's Sign) After Intraoperative Arm Tourniquet Inflation in an Intubated Patient. Cureus. 2020 Apr 4:12(4):e7543. doi: 10.7759/cureus.7543. Epub 2020 Apr 4 [PubMed PMID: 32377491]
Young P, Bravo MA, González MG, Finn BC, Quezel MA, Bruetman JE. [Armand Trousseau (1801-1867), his history and the signs of hypocalcemia]. Revista medica de Chile. 2014 Oct:142(10):1341-7. doi: 10.4067/S0034-98872014001000017. Epub [PubMed PMID: 25601121]
van Bussel BC, Koopmans RP. Trousseau's sign at the emergency department. BMJ case reports. 2016 Aug 1:2016():. doi: 10.1136/bcr-2016-216270. Epub 2016 Aug 1 [PubMed PMID: 27481262]
Level 3 (low-level) evidenceJesus JE, Landry A. Images in clinical medicine. Chvostek's and Trousseau's signs. The New England journal of medicine. 2012 Sep 13:367(11):e15. doi: 10.1056/NEJMicm1110569. Epub [PubMed PMID: 22970971]
Level 3 (low-level) evidenceWilliams A, Liddle D, Abraham V. Tetany: A diagnostic dilemma. Journal of anaesthesiology, clinical pharmacology. 2011 Jul:27(3):393-4. doi: 10.4103/0970-9185.83691. Epub [PubMed PMID: 21897517]
Level 3 (low-level) evidenceOmerovic S, Das JM. Chvostek Sign. StatPearls. 2025 Jan:(): [PubMed PMID: 31194466]
Chhabra ST, Mehta S, Chhabra S, Singla M, Aslam N, Mohan B, Wander GS. Hypocalcemia Presenting as Life Threatening Torsades de Pointes with Prolongation of QTc Interval. Indian journal of clinical biochemistry : IJCB. 2018 Apr:33(2):235-238. doi: 10.1007/s12291-017-0684-z. Epub 2017 Aug 1 [PubMed PMID: 29651218]
Nijjer S, Ghosh AK, Dubrey SW. Hypocalcaemia, long QT interval and atrial arrhythmias. BMJ case reports. 2010:2010():bcr0820092216. doi: 10.1136/bcr.08.2009.2216. Epub 2010 Jan 13 [PubMed PMID: 22242081]
Level 3 (low-level) evidenceFeingold KR, Ahmed SF, Anawalt B, Blackman MR, Boyce A, Chrousos G, Corpas E, de Herder WW, Dhatariya K, Dungan K, Hofland J, Kalra S, Kaltsas G, Kapoor N, Koch C, Kopp P, Korbonits M, Kovacs CS, Kuohung W, Laferrère B, Levy M, McGee EA, McLachlan R, Muzumdar R, Purnell J, Rey R, Sahay R, Shah AS, Singer F, Sperling MA, Stratakis CA, Trence DL, Wilson DP, Schafer AL, Shoback DM. Hypocalcemia: Diagnosis and Treatment. Endotext. 2000:(): [PubMed PMID: 25905251]
Pepe J, Colangelo L, Biamonte F, Sonato C, Danese VC, Cecchetti V, Occhiuto M, Piazzolla V, De Martino V, Ferrone F, Minisola S, Cipriani C. Diagnosis and management of hypocalcemia. Endocrine. 2020 Sep:69(3):485-495. doi: 10.1007/s12020-020-02324-2. Epub 2020 May 4 [PubMed PMID: 32367335]
Zaloga GP, Chernow B. The multifactorial basis for hypocalcemia during sepsis. Studies of the parathyroid hormone-vitamin D axis. Annals of internal medicine. 1987 Jul:107(1):36-41 [PubMed PMID: 3592447]
Goyal A, Anastasopoulou C, Ngu M, Singh S. Hypocalcemia. StatPearls. 2025 Jan:(): [PubMed PMID: 28613662]
Liamis G, Milionis HJ, Elisaf M. A review of drug-induced hypocalcemia. Journal of bone and mineral metabolism. 2009:27(6):635-42. doi: 10.1007/s00774-009-0119-x. Epub [PubMed PMID: 19730969]
Li K, Xu Y. Citrate metabolism in blood transfusions and its relationship due to metabolic alkalosis and respiratory acidosis. International journal of clinical and experimental medicine. 2015:8(4):6578-84 [PubMed PMID: 26131288]
Davis AM. Hypocalcemia in rhabdomyolysis. JAMA. 1987 Feb 6:257(5):626 [PubMed PMID: 3795440]
Level 3 (low-level) evidenceWilliams SM, Killeen AA. Tumor Lysis Syndrome. Archives of pathology & laboratory medicine. 2019 Mar:143(3):386-393. doi: 10.5858/arpa.2017-0278-RS. Epub 2018 Nov 30 [PubMed PMID: 30499695]