Introduction
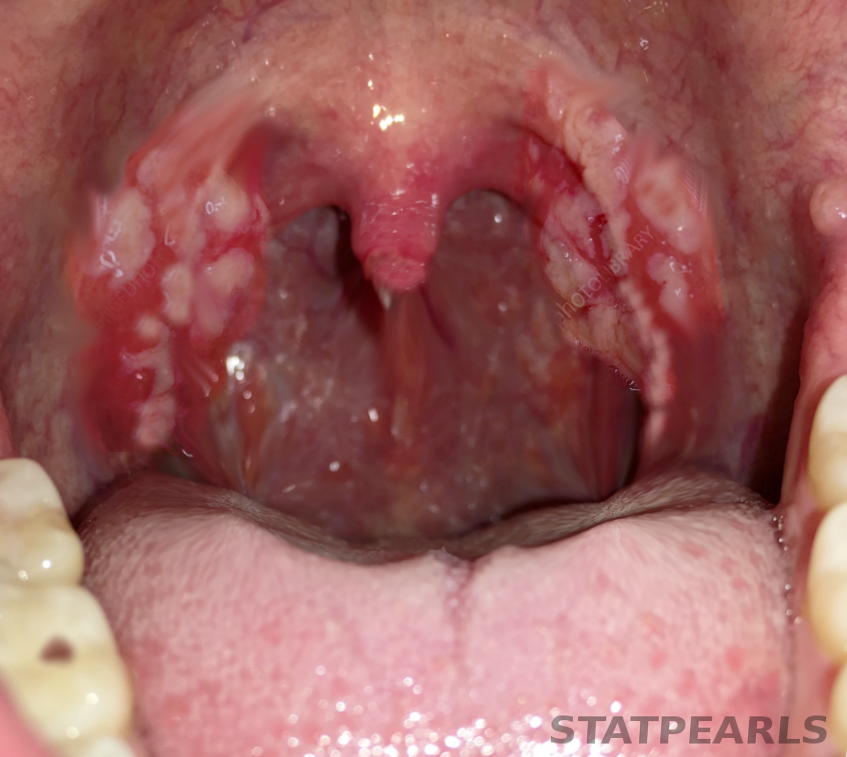
Tonsillitis is inflammation of the palatine tonsils and typically presents with sore throat, odynophagia, fever, and erythematous or exudative tonsils. This condition causes frequent healthcare visits worldwide, comprising approximately 1.3% of outpatient encounters.[1] The palatine tonsils in the lateral oropharynx between the palatoglossal and palatopharyngeal arches comprise lymphoid tissue and are a key component of the Waldeyer ring.[2][3] These structures serve as a first-line immunologic barrier against inhaled or ingested pathogens.[2][3][4] See Image. Tonsillitis.
Acute tonsillitis is typically infectious in origin and diagnosed clinically. Viral pathogens are responsible for 70% to 95% of cases, while bacterial pathogens—particularly Streptococcus pyogenes (group A Streptococcus [GAS])—account for 5% to 15% of adult cases and 15% to 30% of pediatric cases, especially in children aged 5 to 15.[5][6] Timely differentiation between viral and bacterial tonsillitis is essential to guide appropriate antimicrobial use and reduce unnecessary antibiotic prescriptions. This distinction is crucial, as streptococcal tonsillitis can lead to complications such as peritonsillar abscess, acute rheumatic fever, and poststreptococcal glomerulonephritis.[7][8]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Tonsillitis is primarily caused by infectious agents, with viral pathogens accounting for most cases (approximately 70%–95%).[5][6] Common viral etiologies include rhinovirus, respiratory syncytial virus, adenovirus, coronavirus, Epstein–Barr virus (EBV), cytomegalovirus, and human immunodeficiency virus.[9] These viruses manifest as part of broader upper respiratory tract infections, although systemic viruses like EBV may produce more severe or prolonged illness.[5][6]
Although less common, bacterial causes of tonsillitis are clinically significant due to their potential for complications. Group A beta-hemolytic Streptococcus, or S pyogenes, is the most prevalent bacterial pathogen, particularly in children aged 5 to 15.[10][11] Other implicated organisms include Staphylococcus aureus, Streptococcus pneumoniae, Haemophilus influenzae, Fusobacterium necrophorum (notably in adolescents and young adults), and Streptococcus dysgalactiae.[11][12]
Less common bacterial pathogens include Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Neisseria gonorrhoeae, particularly in sexually active individuals.[10] Corynebacterium diphtheriae should be considered in unvaccinated individuals. Mycobacterium tuberculosis has also been implicated in chronic or recurrent tonsillitis, particularly in high-risk populations.[8][13][14] Recurrent tonsillitis is often polymicrobial, with biofilm-forming organisms such as S aureus and H influenzae contributing to its persistence.[15] Alterations in the tonsillar microbiota and reduced microbial diversity (dysbiosis) have also been associated with recurrence.[13][16]
Epidemiology
Tonsillitis is a common cause of outpatient visits, accounting for approximately 2% of ambulatory encounters in the United States.[17] While it can occur year-round, incidence peaks in winter and early spring.[17][18] Group A beta-hemolytic Streptococcus (GABHS) is the leading bacterial cause of tonsillitis in certain age groups, accounting for 15% to 30% of cases in children aged 5 to 15 and 5% to 15% in adults.
In contrast, viral pathogens predominate in children younger than 5, and GABHS is uncommon in those younger than 2.[17] A recent trend in some regions shows a rise in hospital admissions for severe or complicated tonsillitis, potentially linked to declining tonsillectomy rates following the adoption of stricter surgical criteria.[17] Recurrent tonsillitis, defined as 5 or more episodes annually, is associated with significant morbidity and reduced quality of life.[19]
History and Physical
Tonsillitis typically presents with the sudden onset of sore throat, fever, odynophagia, and pharyngeal erythema. Additional symptoms may include malaise, headache, halitosis, and a muffled ("hot potato") voice.[19]
Key Physical Examination Findings
- Tonsillar erythema, hypertrophy, or purulent exudates [20]
- Tender anterior cervical lymphadenopathy
- Palatal petechiae
- Fever >38 °C/100.4 °F
- Absence of cough (supports bacterial etiology)[20]
- Uvular deviation (may indicate peritonsillar abscess)
Posterior cervical lymphadenopathy and splenomegaly suggest EBV infection, while a fine, sandpaper-like (scarlatiniform) rash may indicate GAS pharyngitis. Trismus, asymmetric tonsillar enlargement, or external neck swelling should raise suspicion for complications such as peritonsillar or deep neck space abscess.[19]
Historical Clues of Diagnostic Value
The clinical history should assess:
- Duration and severity of symptoms
- Presence of viral features (eg, cough, rhinorrhea, conjunctivitis)
- History of recurrent tonsillitis or similar episodes
- Immunocompromised status or chronic illnesses
- Recent sexual activity if sexually transmitted infections are suspected [19]
Evaluation
Tonsillitis is primarily diagnosed clinically, though structured scoring systems and microbiological testing can help distinguish bacterial from viral etiologies.[6][20] Tools such as the Centor and FeverPAIN (fever in the past 24 hours, purulence, attend rapidly [within 3 days], inflamed tonsils, and no cough or coryza) scores improve diagnostic accuracy and guide the need for further testing or antibiotic therapy.
Clinical Scoring Tools
The Centor score is a clinical tool used to estimate the likelihood of GAS pharyngitis based on criteria such as tonsillar exudates, tender anterior cervical lymphadenopathy, fever, and absence of cough (see Table. The Centor Score). Each positive finding contributes 1 point; a higher score increases the probability of bacterial infection and can guide decisions on testing or empiric antibiotic treatment.[21]
Table. The Centor Score
|
Criteria |
Points |
|
Fever >38 °C/100.4 °F |
+1 |
|
Tonsillar exudates or swelling |
+1 |
|
Tender anterior cervical lymphadenopathy |
+1 |
|
Absence of cough |
+1 |
The McIsaac modification of the Centor score adjusts the original criteria by incorporating patient age, improving its applicability across a broader population (see Table. McIsaac Modification). This modification increases diagnostic accuracy, particularly in children and older adults. The total score helps determine the likelihood of streptococcal infection and whether testing or treatment is warranted (see Table. Interpretation of McIsaac Score).
Table. McIsaac Modification
|
Age Adjustment (Years) |
Points |
|
3–14 |
+1 |
|
15–44 |
0 |
|
≥45 |
−1 |
Table. Interpretation of McIsaac Score
|
Score |
Clinical Recommendation |
|
0–1 |
No further testing or antibiotics needed |
|
2–3 |
Consider rapid antigen detection test or throat culture |
|
≥4 |
Recommend diagnostic testing and consider empiric antibiotic therapy |
The FeverPAIN score, commonly used in the United Kingdom, evaluates 5 criteria: fever, purulence, rapid symptom onset, inflamed tonsils, and absence of cough; this aligns with the National Institute for Health and Care Excellence guidelines and promotes rational antibiotic use.[7]
Microbiological Testing
Microbiological confirmation helps differentiate bacterial from viral tonsillitis, especially in suspected cases of group GABHS infection. Accurate identification of the causative agent supports targeted treatment and helps prevent unnecessary antibiotic use.
- Rapid antigen detection test Rapid antigen detection test (RADT) offers high specificity (88%–100%) but variable sensitivity (61%–95%) in children. A positive result supports the diagnosis of streptococcal pharyngitis, while a negative result in high-suspicion pediatric cases should be followed by further testing.
- Throat culture Considered the gold standard for diagnosing GABHS, particularly in children with negative RADT results but high clinical suspicion. Per the Infectious Diseases Society of America guidelines, cultures are essential before initiating antibiotics.[6][22][23]
Testing considerations for tonsillitis should consider patient age, clinical presentation, and risk factors. Routine testing is generally not recommended in children under 3 years due to the low risk of streptococcal complications such as rheumatic fever.[6] Monospot or EBV serology is useful in suspected infectious mononucleosis. Nucleic acid amplification test or culture for Neisseria gonorrhoeae or Chlamydia trachomatis should be considered in sexually active individuals. Human immunodeficiency virus and rapid plasma reagin testing may be warranted in patients with atypical symptoms or high-risk exposures.[24]
Laboratory and Imaging Studies
Laboratory and imaging studies are not routinely required for uncomplicated tonsillitis, but may be warranted in select cases to assess for complications or alternative diagnoses. These investigations can help identify systemic involvement, confirm suspected pathogens, or evaluate for deep neck space infections. Clinical judgement should guide their use based on severity, duration, and associated findings.
- Laboratory tests: Routine blood work, such as a complete blood count or metabolic panel, is typically unnecessary in uncomplicated tonsillitis. However, these tests may help evaluate patients with systemic toxicity or dehydration, or when considering alternative diagnoses.
- Imaging studies: Imaging is reserved for cases where complications are suspected.
- Peritonsillar abscess
- Retropharyngeal or deep neck space infections
- Signs of airway compromise (eg, stridor, drooling, trismus)
Computed tomography (CT) of the neck is the preferred modality, offering high sensitivity for detecting deep space infections and delineating abscess extent. In some cases, ultrasound may be considered an initial modality, especially in children or when CT is not readily available.
Treatment / Management
Managing tonsillitis depends on the underlying etiology, severity of symptoms, and risk of complications. Most cases are viral and self-limiting, requiring only supportive care. Bacterial infections, particularly those caused by GAS, may warrant antibiotic therapy to reduce symptom duration and prevent complications.
Supportive Care
Most cases of tonsillitis are viral and self-limiting, requiring only symptomatic management. Recommended measures include adequate hydration, rest, and analgesics such as acetaminophen or nonsteroidal anti-inflammatory drugs.[25][26] Throat lozenges and warm salt-water gargles may provide additional relief. Topical agents like viscous lidocaine are occasionally used, though supporting evidence remains limited.[27] Herbal remedies and zinc gluconate have demonstrated inconsistent benefits and are generally not recommended.[27]
Adjunctive Corticosteroids
A single dose of corticosteroids (eg, dexamethasone) may accelerate symptom resolution and provide short-term pain relief, particularly in patients with severe odynophagia.[28] Use should be individualized, especially in patients with diabetes or immunocompromised states, where potential risks may outweigh the benefits.[28] (A1)
Antibiotic Therapy
Antibiotics are indicated for confirmed or strongly suspected bacterial tonsillitis, most commonly caused by GAS.[29] First-line regimens include:
- Penicillin V or amoxicillin for 10 days
- Azithromycin, clarithromycin, or first-generation cephalosporins for patients with nonanaphylactic penicillin allergies [23][29][30] (A1)
While antibiotics may shorten symptom duration by approximately 16 hours, their primary benefit is the prevention of complications such as peritonsillar abscess and acute rheumatic fever, particularly in high-risk populations (eg, Indigenous Australians or underserved communities).[31][32] Potential risks include gastrointestinal upset, Clostridioides difficile infection, antibiotic resistance, and increased healthcare costs.[27][30] Chronic GAS carriers typically do not require treatment due to low transmission and complication risks.[33] Current Centers for Disease Control and Prevention and American College of Physicians guidelines recommend antibiotic therapy only when GAS is confirmed by rapid antigen detection testing or throat culture.[33] A delayed prescription or watchful waiting approach may be appropriate in low-risk cases.(A1)
Chronic Versus Recurrent Tonsillitis
Chronic tonsillitis is associated with an increased risk of developing immunoglobulin A nephropathy and may also be linked to Helicobacter pylori infection, suggesting broader systemic and local health implications.[34][35] Persistent inflammation and immune activation in chronic tonsillitis may contribute to these extra-tonsillar effects. Recurrent tonsillitis is often defined as 5 or more episodes annually.[36][37][38] Evaluation should include assessment for underlying conditions such as immunodeficiency. Medical therapy guidelines are as follows:(A1)
- Clindamycin or amoxicillin-clavulanate may be superior to penicillin in eradicating GAS in recurrent cases.[39]
- Prophylactic antibiotics such as long-acting benzathine penicillin or low-dose azithromycin can reduce recurrence frequency. Azithromycin is often preferred in children due to better adherence.[19][39][40][41]
Surgical Management
Tonsillectomy is indicated in patients with recurrent or chronic tonsillitis when the frequency or severity of episodes significantly impacts quality of life.[42] This surgery may also be considered when a patient is unresponsive to medical therapy or complications such as peritonsillar abscess recur. The Paradise criteria are evidence-based guidelines for determining eligibility for tonsillectomy in children with recurrent throat infections due to GAS. To meet the Paradise criteria for tonsillectomy, a child should have:
- ≥7 episodes of throat infection in 1 year, or
- ≥5 episodes annually for 2 consecutive years, or
- ≥3 episodes annually for 3 consecutive years [11] (B2)
Each episode must be well-documented and meet specific clinical features, including:
- Sore throat plus 1 or more of the following:
- Fever ≥38.3 °C (101 °F)
- Cervical lymphadenopathy (tender or >2 cm nodules)
- Tonsillar exudate
- Positive test for GABHS
The American Academy of Otolaryngology–Head and Neck Surgery notes that tonsillectomy offers short-term benefits, including reduced sore throat episodes and fewer school or work absences.[11] However, evidence supporting long-term benefits remains limited. The National Trial of Tonsillectomy in Adults trial demonstrated that adults undergoing tonsillectomy for 3 to 5 episodes per year experienced significantly fewer sore throat days and improved quality of life compared to those managed conservatively.[20] However, these benefits were offset by increased postoperative risks, most notably hemorrhage.(A1)
The Centers for Disease Control and Prevention and the American College of Physicians advise against tonsillectomy solely to reduce the frequency of GAS pharyngitis in adults.[19] Surgical decisions should be individualized, considering symptom severity, recurrence rate, and patient preferences. Judicious antibiotic use and adherence to evidence-based surgical criteria are essential to minimize complications, limit antimicrobial resistance, and reduce healthcare burden. Patient education and clinician awareness are critical to supporting guideline-concordant care and improving outcomes.
Guideline-Based Recommendations
Current clinical guidelines underscore the importance of accurate diagnosis, responsible antibiotic use, and clearly defined surgical indications to manage tonsillitis. These recommendations aim to balance effective treatment with preventing overtreatment and associated risks.
Infectious Diseases Society of America, 2012 Update on Streptococcal Pharyngitis
This guideline outlines best practices for diagnosing and managing GAS pharyngitis and recommends microbiological confirmation using RADT or throat culture before initiating antibiotic therapy. Penicillin or amoxicillin is recommended as first-line treatment.
European Society for Clinical Microbiology and Infectious Diseases, 2012 Guideline for Acute Sore Throat
The European Society for Clinical Microbiology and Infectious Diseases promotes an evidence-based approach, using clinical scoring systems such as Centor or FeverPAIN in conjunction with RADT to guide antibiotic prescribing. Antibiotic use is discouraged in low-risk cases, and the modest benefit of antibiotics in more severe presentations is stressed.
American Academy of Otolaryngology–Head and Neck Surgery, 2019 Clinical Practice Guideline: Tonsillectomy in Children (Update)
This updated guideline delivers evidence-based recommendations for tonsillectomy in pediatric patients. Preoperative, intraoperative, and postoperative management, focusing on indications such as recurrent throat infections and obstructive sleep-disordered breathing, are addressed. The guideline also highlights the importance of shared decision-making between clinicians and caregivers.
Differential Diagnosis
The clinical presentation of tonsillitis can overlap with several other conditions affecting the oropharynx and upper respiratory tract. A thorough evaluation is essential to distinguish tonsillitis from other infectious, inflammatory, or systemic causes of pharyngitis (see Table. Differential Diagnosis of Tonsillitis). Accurate diagnosis ensures appropriate management and helps avoid unnecessary antibiotic use or missed pathology.
Table. Differential Diagnosis of Tonsillitis
|
Condition |
Clinical Features |
|
Viral pharyngitis |
|
|
GAS pharyngitis |
|
|
Infectious mononucleosis (EBV) |
|
|
Non–group A Streptococci (C&G) |
|
|
Mycoplasma/ Chlamydophila pneumoniae |
|
|
Allergic or irritant pharyngitis |
|
|
Epiglottitis |
|
|
Peritonsillar abscess (Quinsy) |
|
|
Retropharyngeal abscess |
|
|
Ludwig angina |
|
|
Diphtheria |
|
|
Primary HIV infection |
|
|
Syphilitic chancre |
|
|
Tuberculosis |
|
|
Herpangina |
|
|
Oropharyngeal candidiasis |
|
Prognosis
The prognosis of acute tonsillitis is generally excellent, especially in otherwise healthy individuals. Most cases, particularly viral, are self-limiting and resolve within 2 to 8 days. Fever typically subsides within 2 to 3 days, and supportive care is sufficient for most patients.[5][6] In bacterial tonsillitis caused by GABHS, prompt antibiotic therapy shortens symptom duration, reduces transmissibility, and helps prevent complications such as acute rheumatic fever and peritonsillar abscess.[47] Timely treatment is essential in high-risk populations to minimize morbidity and long-term sequelae.
While not usually life-threatening, recurrent tonsillitis can significantly impair quality of life, causing frequent school or work absences and sleep disturbances. Patients who meet criteria and undergo tonsillectomy may experience symptomatic relief, although the long-term benefits can be variable.[48] Nonsuppurative complications of GABHS, such as acute rheumatic fever and poststreptococcal glomerulonephritis, have become rare in high-income countries due to early antibiotic treatment. However, they remain a concern in low-resource settings.[49]
If symptoms persist or worsen despite standard treatment, clinicians must consider alternative or coexisting diagnoses such as:
- Infectious mononucleosis
- Human immunodeficiency virus
- Tuberculosis
- Gonorrhea
- Syphilis
- Kawasaki disease
- Deep space infections (eg, peritonsillar or retropharyngeal abscess, Lemierre syndrome)
When tonsillitis is appropriately managed, the outcome is excellent, whether viral or bacterial. Complications are uncommon in modern clinical practice with proper diagnostic evaluation and treatment.
Complications
While tonsillitis is usually self-limited with a favorable prognosis, local and systemic complications can occur, particularly when caused by GABHS or delayed treatment.[45] Early recognition and appropriate management are essential to prevent adverse outcomes and ensure optimal patient recovery.
Local Complications
Local complications of tonsillitis arise when infection extends beyond the tonsillar tissue into adjacent structures. Though uncommon with timely treatment, these complications can be serious and require prompt recognition and intervention.
- Peritonsillar abscess (quinsy)
- This is the most common suppurative complication of tonsillitis, characterized by pus accumulation between the tonsillar capsule and pharyngeal constrictor muscle.[41][50] This condition typically presents with unilateral sore throat, trismus, uvular deviation, and a muffled “hot potato” voice. Most cases are polymicrobial, with risk factors including smoking and prior tonsillitis. Treatment involves needle aspiration, incision, drainage, and antibiotics and corticosteroids.[51][47] In a few instances, patients develop suppurative tonsillitis and necrotizing tonsillitis caused by S pyogenes superinfection in a patient with EBV-associated mononucleosis.[52][53] The Pediatric Appropriate Antibiotic Therapy–1 is the first validated patient-reported tool to assess symptom severity, duration, and treatment efficacy in peritonsillar abscess from the patient’s perspective.[54][55]
- Deep space infections
- Airway Obstruction
- This is seen predominantly in children with significant tonsillar hypertrophy, leading to partial or complete airway compromise.[60]
- Tonsillar hemorrhage
- This rare event results from erosion into nearby blood vessels, often triggered by trauma, inflammation, or infection.[60]
Systemic Complications
Systemic complications of tonsillitis occur when the infection triggers immune-mediated responses or spreads beyond the oropharynx. Though rare in high-resource settings, conditions such as acute rheumatic fever and poststreptococcal glomerulonephritis remain important considerations, particularly in untreated or high-risk individuals.
- Acute rheumatic fever
- This is an autoimmune complication of GABHS pharyngitis, typically affecting children aged 5 to 18. Clinical signs include migratory arthritis, carditis (especially mitral valve involvement), Sydenham chorea, subcutaneous nodules, and erythema marginatum. While uncommon in high-income countries, it remains prevalent in resource-limited settings.[46]
- Poststreptococcal glomerulonephritis
- This is an immune-mediated renal condition following GABHS infection. Presents with hematuria, edema, hypertension, and low complement levels. Prognosis is generally favorable in children, but outcomes may worsen in older individuals.[24]
- Lemierre syndrome
- This syndrome is a rare but serious condition caused by Fusobacterium necrophorum, involving septic thrombophlebitis of the internal jugular vein. This condition typically presents with fever, neck pain, and signs of septic emboli, most commonly to the lungs. Complications can include ARDS, osteomyelitis, and meningitis.[49]
- Scarlet fever
- This toxin-mediated illness from GABHS is characterized by a fine sandpaper-like rash and a “strawberry” tongue and may coexist with streptococcal tonsillitis.[45]
- Acute myopericarditis
- Though rare, this condition has been reported in young males with severe bacterial tonsillitis, particularly those presenting with chest pain.[47]
- Other rare complications
- These include sepsis, necrotizing fasciitis, superior sagittal sinus thrombosis, and Guillain-Barré syndrome, particularly in immunocompromised individuals.[60]
Deterrence and Patient Education
Effective patient education is a cornerstone in managing tonsillitis, particularly in curbing unnecessary antibiotic use and alleviating the overall burden on healthcare systems. Clinicians should communicate that most cases of tonsillitis are viral and self-limiting, resolving without the need for antimicrobial therapy.[45] Using structured clinical decision tools, such as the Centor and McIsaac criteria, can help stratify the likelihood of GAS infection. These tools also support shared decision-making by providing a clear rationale for diagnostic testing or withholding antibiotics.[45]
While antibiotics may modestly reduce symptom duration in GAS tonsillitis (typically by less than 24 hours), their primary benefit lies in preventing complications such as peritonsillar abscess and acute rheumatic fever, which have become uncommon in high-income countries.[45] Nevertheless, patients must be informed of the potential risks associated with antibiotic use, including gastrointestinal side effects, allergic reactions, Clostridioides difficile infection, and antimicrobial resistance.[45]
Pearls and Other Issues
Key facts to keep in mind about tonsillitis include the following:
- Tonsillitis is most commonly viral, and supportive care remains the cornerstone of treatment. Avoid unnecessary antibiotics in low-risk individuals.
- GABHS is the primary bacterial cause; Centor or McIsaac criteria guide testing and antibiotic decisions.
- RADTs have high specificity but variable sensitivity; in high-suspicion cases, particularly in children, follow up with a throat culture.
- Consider EBV (infectious mononucleosis) in adolescents and young adults with significant fatigue, posterior cervical lymphadenopathy, or hepatosplenomegaly.
- Watch for complications such as peritonsillar abscess, retropharyngeal abscess, Lemierre syndrome, and airway compromise—these require urgent escalation of care.
- Corticosteroids (eg, dexamethasone) can offer rapid symptom relief in severe cases but should be used judiciously, particularly in patients with diabetes or immunosuppression.
- Antibiotics modestly reduce symptom duration and primarily serve to prevent rheumatic fever, glomerulonephritis, and suppurative complications in high-risk populations.
- Recurrent tonsillitis should prompt evaluation for surgical referral; tonsillectomy is considered based on established frequency thresholds and impact on quality of life.
- Patient education is essential. Discuss the expected disease course, treatment rationale, and signs of complications to reduce unnecessary return visits and promote adherence.
- Maintain a high index of suspicion for rare but serious diagnoses (eg, human immunodeficiency virus, tuberculosis, diphtheria, gonococcal pharyngitis) in appropriate clinical contexts or high-risk populations.
Enhancing Healthcare Team Outcomes
Effective management of tonsillitis relies on a coordinated interprofessional approach involving clinicians, nurses, pharmacists, radiologists, and specialists. Primary care clinicians serve as the initial point of contact, utilizing validated clinical tools (eg, Centor or McIsaac criteria) to differentiate viral from bacterial etiologies and guide appropriate antibiotic use. Shared decision-making is essential, particularly in discussing risks, benefits, and antibiotic stewardship.[45]
Nurses contribute through patient education, monitoring, and care coordination.[61] Pharmacists ensure appropriate antibiotic selection, dosing, and adherence counseling. Radiologists assist in identifying complications, such as deep neck space infections, through context-informed imaging interpretation. Specialist input—including otolaryngology, infectious disease, and nephrology—is warranted in recurrent or atypical cases.
Evidence of treatment effectiveness includes multiple large randomized controlled trials and Cochrane reviews supporting antibiotic use in confirmed GAS tonsillitis. The decision-to-treat model, including the Centor criteria, has been validated in several extensive studies for its diagnostic utility and risk stratification.[45][47] While high-level evidence supports these practices, rare conditions such as Lemierre syndrome and tuberculous tonsillitis are guided primarily by Level 5 evidence from case reports and expert opinion. Collaborative communication and role clarity across the care continuum are essential to achieving accurate diagnoses, timely interventions, and improved patient outcomes. Interdisciplinary coordination also helps minimize delays, reduce redundancies, and ensure that care is aligned with best practices and patient needs.
Media
(Click Image to Enlarge)
References
Meegalla N, Downs BW. Anatomy, Head and Neck, Palatine Tonsil (Faucial Tonsils). StatPearls. 2025 Jan:(): [PubMed PMID: 30855880]
Masters KG, Zezoff D, Lasrado S. Anatomy, Head and Neck, Tonsils. StatPearls. 2025 Jan:(): [PubMed PMID: 30969614]
Kocher JJ, Selby TD. Antibiotics for sore throat. American family physician. 2014 Jul 1:90(1):23-4 [PubMed PMID: 25077497]
Null M, Arbor TC, Agarwal M. Anatomy, Lymphatic System. StatPearls. 2025 Jan:(): [PubMed PMID: 30020619]
Bartlett A, Bola S, Williams R. Acute tonsillitis and its complications: an overview. Journal of the Royal Naval Medical Service. 2015:101(1):69-73 [PubMed PMID: 26292396]
Level 3 (low-level) evidenceSmith KL, Hughes R, Myrex P. Tonsillitis and Tonsilloliths: Diagnosis and Management. American family physician. 2023 Jan:107(1):35-41 [PubMed PMID: 36689967]
Putukian M, McGrew CA, Benjamin HJ, Hammell MK, Hwang CE, Ray JW, Statuta SM, Sylvester J, Wilson K. American Medical Society of Sports Medicine Position Statement: Mononucleosis and Athletic Participation. Clinical journal of sport medicine : official journal of the Canadian Academy of Sport Medicine. 2023 May 15:():. doi: 10.1097/JSM.0000000000001161. Epub 2023 May 15 [PubMed PMID: 37186809]
González-Andrade B, Santos-Lartigue R, Flores-Treviño S, Ramirez-Ochoa NS, Bocanegra-Ibarias P, Huerta-Torres FJ, Mendoza-Olazarán S, Villarreal-Treviño L, Camacho-Ortiz A, Villarreal-Vázquez H, Garza-González E. The carriage of interleukin-1B-31*C allele plus Staphylococcus aureus and Haemophilus influenzae increases the risk of recurrent tonsillitis in a Mexican population. PloS one. 2017:12(5):e0178115. doi: 10.1371/journal.pone.0178115. Epub 2017 May 24 [PubMed PMID: 28542534]
Alves METF, Mello LF, Alves FRF. Acute Epstein-Barr Virus and SARS-CoV-2 Coinfection: A Case Report. Current health sciences journal. 2024 Jul-Sep:50(3):453-457. doi: 10.12865/CHSJ.50.03.14. Epub 2024 Sep 30 [PubMed PMID: 39574816]
Level 3 (low-level) evidenceMiller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gonzalez MD, Harrington A, Jerris RC, Kehl SC, Leal SM Jr, Patel R, Pritt BS, Richter SS, Robinson-Dunn B, Snyder JW, Telford S 3rd, Theel ES, Thomson RB Jr, Weinstein MP, Yao JD. Guide to Utilization of the Microbiology Laboratory for Diagnosis of Infectious Diseases: 2024 Update by the Infectious Diseases Society of America (IDSA) and the American Society for Microbiology (ASM). Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2024 Mar 5:():. pii: ciae104. doi: 10.1093/cid/ciae104. Epub 2024 Mar 5 [PubMed PMID: 38442248]
Pallon J, Rööst M, Sundqvist M, Hedin K. The aetiology of pharyngotonsillitis in primary health care: a prospective observational study. BMC infectious diseases. 2021 Sep 17:21(1):971. doi: 10.1186/s12879-021-06665-9. Epub 2021 Sep 17 [PubMed PMID: 34535115]
Level 2 (mid-level) evidenceAndersen C, Greve T, Reinholdt KB, Kjaerulff AMG, Udholm N, Khalid V, Madzak A, Duez C, Münch H, Pauli S, Danstrup CS, Petersen NK, Klug TE. Bacterial findings in patients referred to hospital for the treatment of acute tonsillitis with or without peritonsillar phlegmon. BMC infectious diseases. 2023 Jun 29:23(1):439. doi: 10.1186/s12879-023-08420-8. Epub 2023 Jun 29 [PubMed PMID: 37386401]
Wang Q, Du J, Jie C, Ouyang H, Luo R, Li W. Bacteriology and antibiotic sensitivity of tonsillar diseases in Chinese children. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2017 Aug:274(8):3153-3159. doi: 10.1007/s00405-017-4603-y. Epub 2017 May 27 [PubMed PMID: 28551703]
Ben Ammar C, Tbini M, Kamel HE, Riahi I, Ben Salah M. Tonsillar tuberculosis mimicking tonsillar carcinoma: A case report. International journal of surgery case reports. 2024 Aug:121():110032. doi: 10.1016/j.ijscr.2024.110032. Epub 2024 Jul 12 [PubMed PMID: 39002392]
Level 3 (low-level) evidenceKlagisa R, Racenis K, Broks R, Balode AO, Kise L, Kroica J. Analysis of Microorganism Colonization, Biofilm Production, and Antibacterial Susceptibility in Recurrent Tonsillitis and Peritonsillar Abscess Patients. International journal of molecular sciences. 2022 Sep 7:23(18):. doi: 10.3390/ijms231810273. Epub 2022 Sep 7 [PubMed PMID: 36142185]
Banigo A, Moinie A, Bleach N, Chand M, Chalker V, Lamagni T. Have reducing tonsillectomy rates in England led to increasing incidence of invasive Group A Streptococcus infections in children? Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2018 Jun:43(3):912-919. doi: 10.1111/coa.13095. Epub 2018 Apr 16 [PubMed PMID: 29505705]
Douglas CM, Lang K, Whitmer WM, Wilson JA, Mackenzie K. The effect of tonsillectomy on the morbidity from recurrent tonsillitis. Clinical otolaryngology : official journal of ENT-UK ; official journal of Netherlands Society for Oto-Rhino-Laryngology & Cervico-Facial Surgery. 2017 Dec:42(6):1206-1210. doi: 10.1111/coa.12850. Epub 2017 Mar 9 [PubMed PMID: 28199053]
Seidel DU, Bode S, Kostev K. Seasonal variation and demographic characteristics of acute tonsillitis and peritonsillar abscess in ENT practices in Germany (2019-2023). European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2025 Jan:282(1):317-326. doi: 10.1007/s00405-024-09034-9. Epub 2024 Oct 15 [PubMed PMID: 39404879]
Gottlieb M, Long B, Koyfman A. Clinical Mimics: An Emergency Medicine-Focused Review of Streptococcal Pharyngitis Mimics. The Journal of emergency medicine. 2018 May:54(5):619-629. doi: 10.1016/j.jemermed.2018.01.031. Epub 2018 Mar 6 [PubMed PMID: 29523424]
Ebell MH, Call M, Shinholser J, Gardner J. Does This Patient Have Infectious Mononucleosis?: The Rational Clinical Examination Systematic Review. JAMA. 2016 Apr 12:315(14):1502-9. doi: 10.1001/jama.2016.2111. Epub [PubMed PMID: 27115266]
Level 1 (high-level) evidenceJääskeläinen J, Renko M, Kuitunen I. The impact of national guidelines on the diagnostics of sore throat in children. BMC pediatrics. 2024 Aug 6:24(1):503. doi: 10.1186/s12887-024-04982-x. Epub 2024 Aug 6 [PubMed PMID: 39107694]
Shevale VB, Shinde RV, Patil SR. Bacteriological Profiles and Antimicrobial Susceptibility Patterns Among Isolates in Tonsillitis Patients Attending a Tertiary Care Hospital. Cureus. 2024 Oct:16(10):e72403. doi: 10.7759/cureus.72403. Epub 2024 Oct 25 [PubMed PMID: 39588446]
Tirago TD, Worku M, Nima TM, Ormago MD. Microbial Composition, Antibiotic Sensitivity Patterns, and Contributing Factors Among Children With Tonsillitis in Hawassa Town, Sidama, Ethiopia. International journal of microbiology. 2025:2025():6366378. doi: 10.1155/ijm/6366378. Epub 2025 Apr 16 [PubMed PMID: 40270984]
Stelter K. Tonsillitis and sore throat in children. GMS current topics in otorhinolaryngology, head and neck surgery. 2014:13():Doc07. doi: 10.3205/cto000110. Epub 2014 Dec 1 [PubMed PMID: 25587367]
Schams SC, Goldman RD. Steroids as adjuvant treatment of sore throat in acute bacterial pharyngitis. Canadian family physician Medecin de famille canadien. 2012 Jan:58(1):52-4 [PubMed PMID: 22267621]
ESCMID Sore Throat Guideline Group, Pelucchi C, Grigoryan L, Galeone C, Esposito S, Huovinen P, Little P, Verheij T. Guideline for the management of acute sore throat. Clinical microbiology and infection : the official publication of the European Society of Clinical Microbiology and Infectious Diseases. 2012 Apr:18 Suppl 1():1-28. doi: 10.1111/j.1469-0691.2012.03766.x. Epub [PubMed PMID: 22432746]
Sidell D, Shapiro NL. Acute tonsillitis. Infectious disorders drug targets. 2012 Aug:12(4):271-6 [PubMed PMID: 22338587]
Georgalas CC, Tolley NS, Narula PA. Tonsillitis. BMJ clinical evidence. 2014 Jul 22:2014():. pii: 0503. Epub 2014 Jul 22 [PubMed PMID: 25051184]
Level 1 (high-level) evidenceIckrath P, Morbach H, Schwaneck EC, Gehrke T, Scherzad A, Hagen R, Hackenberg S. [Recurrent infections of the upper aerodigestive tract in patients with primary immunodeficiency]. HNO. 2019 Nov:67(11):819-824. doi: 10.1007/s00106-019-0683-x. Epub [PubMed PMID: 31119330]
Morad A, Sathe NA, Francis DO, McPheeters ML, Chinnadurai S. Tonsillectomy Versus Watchful Waiting for Recurrent Throat Infection: A Systematic Review. Pediatrics. 2017 Feb:139(2):. doi: 10.1542/peds.2016-3490. Epub 2017 Jan 17 [PubMed PMID: 28096515]
Level 1 (high-level) evidenceMunck H, Jørgensen AW, Klug TE. Antibiotics for recurrent acute pharyngo-tonsillitis: systematic review. European journal of clinical microbiology & infectious diseases : official publication of the European Society of Clinical Microbiology. 2018 Jul:37(7):1221-1230. doi: 10.1007/s10096-018-3245-3. Epub 2018 Apr 13 [PubMed PMID: 29651614]
Level 1 (high-level) evidenceEl Hennawi DED, Geneid A, Zaher S, Ahmed MR. Management of recurrent tonsillitis in children. American journal of otolaryngology. 2017 Jul-Aug:38(4):371-374. doi: 10.1016/j.amjoto.2017.03.001. Epub 2017 Mar 3 [PubMed PMID: 28385329]
Wilson JA, O'Hara J, Fouweather T, Homer T, Stocken DD, Vale L, Haighton C, Rousseau N, Wilson R, McSweeney L, Wilkes S, Morrison J, MacKenzie K, Ah-See K, Carrie S, Hopkins C, Howe N, Hussain M, Mehanna H, Raine C, Sullivan F, von Wilamowitz-Moellendorff A, Teare MD. Conservative management versus tonsillectomy in adults with recurrent acute tonsillitis in the UK (NATTINA): a multicentre, open-label, randomised controlled trial. Lancet (London, England). 2023 Jun 17:401(10393):2051-2059. doi: 10.1016/S0140-6736(23)00519-6. Epub 2023 May 17 [PubMed PMID: 37209706]
Level 1 (high-level) evidenceNakayama T, Kaneko H, Suzuki Y, Okada A, Morita H, Fujiu K, Takeda N, Fukui A, Yokoo T, Takeda N, Yasunaga H, Nangaku M, Hayashi K. Chronic Tonsillitis and IgA Nephropathy: Findings From a Nationwide Japanese Cohort Study. American journal of kidney diseases : the official journal of the National Kidney Foundation. 2024 Nov:84(5):613-620.e1. doi: 10.1053/j.ajkd.2024.04.015. Epub 2024 Jun 19 [PubMed PMID: 38906505]
Thangaraj P, Sakthignanavel A, Kaliyamoorthy S, Thingujam S, Radhakrishnan V. Association of Helicobacter Pylori in Chronic Tonsillitis. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2024 Aug:76(4):3001-3006. doi: 10.1007/s12070-024-04569-z. Epub 2024 Mar 15 [PubMed PMID: 39130323]
Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, Martin JM, Van Beneden C, Infectious Diseases Society of America. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2012 Nov 15:55(10):e86-102. doi: 10.1093/cid/cis629. Epub 2012 Sep 9 [PubMed PMID: 22965026]
Level 1 (high-level) evidenceSylvester JE, Buchanan BK, Silva TW. Infectious Mononucleosis: Rapid Evidence Review. American family physician. 2023 Jan:107(1):71-78 [PubMed PMID: 36689975]
Guntinas-Lichius O, Geißler K. [Diagnosis and Treatment of recurrent acute Tonsillitis]. Laryngo- rhino- otologie. 2025 Apr:104(4):256-266. doi: 10.1055/a-2244-6640. Epub 2025 Apr 1 [PubMed PMID: 40168968]
Bernstein JA, Bernstein JS, Makol R, Ward S. Allergic Rhinitis: A Review. JAMA. 2024 Mar 12:331(10):866-877. doi: 10.1001/jama.2024.0530. Epub [PubMed PMID: 38470381]
Bridwell RE, Koyfman A, Long B. High risk and low prevalence diseases: Adult epiglottitis. The American journal of emergency medicine. 2022 Jul:57():14-20. doi: 10.1016/j.ajem.2022.04.018. Epub 2022 Apr 20 [PubMed PMID: 35489220]
Gupta G, McDowell RH. Peritonsillar Abscess. StatPearls. 2025 Jan:(): [PubMed PMID: 30137805]
Bohr C, Shermetaro C. Tonsillectomy and Adenoidectomy. StatPearls. 2025 Jan:(): [PubMed PMID: 30725627]
Sievert M, Miksch M, Hinken N, Mantsoupoulos K, Gostian AO, Thimsen V, Mueller SK, Balk M, Rupp R, Iro H, Koch M. Predictive factors for abscessing tonsillitis: a retrospective analysis. European review for medical and pharmacological sciences. 2023 Nov:27(21):10690-10696. doi: 10.26355/eurrev_202311_34349. Epub [PubMed PMID: 37975394]
Level 2 (mid-level) evidenceConte M, Vinci F, Muzzi E, Canuto A, Barbi E, Cozzi G. Magnetic resonance imaging accuracy before surgery in children with retropharyngeal abscesses. Journal of paediatrics and child health. 2022 Mar:58(3):504-507. doi: 10.1111/jpc.15761. Epub 2021 Oct 4 [PubMed PMID: 34605585]
Klug TE, Rusan M, Fuursted K, Ovesen T. Peritonsillar Abscess: Complication of Acute Tonsillitis or Weber's Glands Infection? Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2016 Aug:155(2):199-207. doi: 10.1177/0194599816639551. Epub 2016 Mar 29 [PubMed PMID: 27026737]
Walker MJ, Barnett TC, McArthur JD, Cole JN, Gillen CM, Henningham A, Sriprakash KS, Sanderson-Smith ML, Nizet V. Disease manifestations and pathogenic mechanisms of Group A Streptococcus. Clinical microbiology reviews. 2014 Apr:27(2):264-301. doi: 10.1128/CMR.00101-13. Epub [PubMed PMID: 24696436]
Level 3 (low-level) evidenceGahleitner C, Hofauer B, Stark T, Knopf A. Predisposing factors and management of complications in acute tonsillitis. Acta oto-laryngologica. 2016 Sep:136(9):964-8. doi: 10.3109/00016489.2016.1170202. Epub 2016 Apr 25 [PubMed PMID: 27109151]
Bell Z, Menezes AA, Primrose WJ, McGuigan JA. Mediastinitis: a life-threatening complication of acute tonsillitis. The Journal of laryngology and otology. 2005 Sep:119(9):743-5 [PubMed PMID: 16156922]
Klug TE, Greve T, Hentze M. Complications of peritonsillar abscess. Annals of clinical microbiology and antimicrobials. 2020 Jul 30:19(1):32. doi: 10.1186/s12941-020-00375-x. Epub 2020 Jul 30 [PubMed PMID: 32731900]
Rangen JK, Madsen MS, Kjærsgaard S. Peritonsillar abscess in a nine-week-old patient. Ugeskrift for laeger. 2024 Sep 23:186(39):. pii: V04240272. doi: 10.61409/V04240272. Epub [PubMed PMID: 39530443]
Johannesen KM, Bodtger U. Lemierre's syndrome: current perspectives on diagnosis and management. Infection and drug resistance. 2016:9():221-227 [PubMed PMID: 27695351]
Level 3 (low-level) evidenceMangerel J, Chung J, Lin YS, Derman A. Double trouble: Necrotizing tonsillitis in the setting of streptococcus pyogenes superinfection in a patient with Epstein-Barr virus. Radiology case reports. 2024 Dec:19(12):5967-5969. doi: 10.1016/j.radcr.2024.09.024. Epub 2024 Sep 17 [PubMed PMID: 39328937]
Level 3 (low-level) evidenceWang C, Duan L, Li P, Zhao W, Cao X. A case of suppurative tonsillitis as a complication of acute infectious mononucleosis. Science progress. 2025 Apr-Jun:108(2):368504251344169. doi: 10.1177/00368504251344169. Epub 2025 May 23 [PubMed PMID: 40405785]
Level 3 (low-level) evidenceKjærulff AMG, Fuglsang S, Klug TE. Peritonsillar abscess assessment tool. Danish medical journal. 2024 Jul 17:71(8):. pii: A01240060. doi: 10.61409/A01240060. Epub 2024 Jul 17 [PubMed PMID: 40116451]
Portillo-Medina A, Golet Fors M, Penella Prat A, Manos M, Videla S, González-Compta X. Recurrent peritonsillar abscess in adults: Incidence and risk factors in a prospective longitudinal cohort. Acta otorrinolaringologica espanola. 2024 Nov-Dec:75(6):361-366. doi: 10.1016/j.otoeng.2024.09.001. Epub 2024 Sep 19 [PubMed PMID: 39306078]
Jain H, Hohman MH, Sinha V. Retropharyngeal Abscess. StatPearls. 2025 Jan:(): [PubMed PMID: 28722903]
Almuqamam M, Gonzalez FJ, Kondamudi NP. Deep Neck Infections. StatPearls. 2023 Jan:(): [PubMed PMID: 30020634]
Isankova O, Safronovs J, Berke K, Taurmane L. Deep Neck Infections. Review of 111 cases. Otolaryngologia polska = The Polish otolaryngology. 2025 Jan 15:79(1):1-5. doi: 10.5604/01.3001.0054.8465. Epub [PubMed PMID: 39812309]
Level 3 (low-level) evidenceCharlton A, Simon R, Shanthakunalan K, Simons A. Deep neck space infections: a UK centre, two-year, retrospective review of 53 cases. The Journal of laryngology and otology. 2024 Dec:138(12):1161-1169. doi: 10.1017/S0022215124001117. Epub 2024 Oct 22 [PubMed PMID: 39434660]
Level 2 (mid-level) evidenceNieuwoudt I, Goussard P, Verster J, Dempers J. Tonsillar hypertrophy and prolapse in a child - is epiglottitis a predisposing factor for sudden unexpected death? BMC pediatrics. 2020 Jan 20:20(1):22. doi: 10.1186/s12887-020-1927-3. Epub 2020 Jan 20 [PubMed PMID: 31959132]
Han F, Wu F, Ma M. Specific Measures and Benefits of Comprehensive Nursing Model in Clinical Practice for Pediatric Purulent Tonsillitis. Alternative therapies in health and medicine. 2025 Jan 14:():. pii: AT10933. Epub 2025 Jan 14 [PubMed PMID: 38904631]