Introduction
The thyroid gland is a midline anterior cervical structure, overlying the C5 to T1 vertebral levels. This gland functions as an endocrine organ, producing thyroid hormone and calcitonin, thereby regulating metabolism, growth, and serum calcium concentrations.
Multiple disease processes can involve the thyroid. Altered hormone production results in hypothyroidism or hyperthyroidism. The gland is susceptible to inflammatory conditions such as thyroiditis, autoimmune disorders such as Graves disease, and malignancies that include papillary thyroid carcinoma, follicular carcinoma, and medullary thyroid carcinoma.[1][2] The thyroid also has important anatomical relationships, lying adjacent to the parathyroid glands, recurrent laryngeal nerves (RLNs), and regional vasculature.
Understanding thyroid anatomy and function enables clinicians to recognize and treat endocrine, inflammatory, and neoplastic conditions that affect this gland. Familiarity with this organ's anatomical relationships also aids in minimizing complications during surgical procedures involving the neck.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The thyroid gland weighs approximately 25 g in adults and has an average volume of 6.6 ml.[3] The gland lies within the middle (visceral) compartment of the neck, an anatomical space bounded anteriorly by the strap muscles and posteriorly by the deep cervical fascia, which also encloses the esophagus, pharynx, and trachea.[4] This compartment extends superiorly to the hyoid bone and inferiorly to the arch of the aorta.
The thyroid consists of 2 typically symmetrical lobes connected by the isthmus, which crosses the upper trachea at the level of the 2nd and 3rd tracheal rings. A pyramidal extension is often present on either lobe, referred to as the "tubercle of Zuckerkandl." Despite these common features, the thyroid exhibits considerable morphologic variation.
The organ lies posterior to the sternothyroid and sternohyoid muscles, enveloping the cricoid cartilage and tracheal rings, and inferior to the laryngeal thyroid cartilage. The thyroid generally spans the vertebral levels C5 to T1.[5] This gland is anchored to the trachea by a consolidation of connective tissue known as the lateral suspensory ligament, or Berry ligament, which secures each lobe to the trachea.[6]
Laterally, the thyroid is covered by the sternothyroid muscle. Medially, the organ abuts the larynx and trachea. Posteriorly, the gland lies adjacent to the carotid sheath and partially overlaps the common carotid artery.
Embryology
The parenchyma of the thyroid gland originates from endoderm. Development begins at the foramen cecum, a pit located at the junction of the anterior 2/3 and posterior 1/3 of the tongue.[7] Early in gestation, the thyroid forms as a bilobed diverticulum that descends anterior to the pharynx. This structure continues its descent anterior to the hyoid bone and laryngeal cartilages. By the 7th week of development, the thyroid reaches its definitive position, midline and anterior to the upper trachea. The thyroglossal duct maintains a transient connection between the developing thyroid and the base of the tongue, which typically involutes and disappears thereafter.
The ultimobranchial body, derived from the ventral portion of the 4th pharyngeal pouch, incorporates into the dorsal aspect of the developing thyroid. This structure gives rise to the gland's parafollicular cells (C cells), which contribute to calcitonin production.
Blood Supply and Lymphatics
The thyroid gland receives a rich arterial supply from the superior and inferior thyroid arteries, which perfuse the upper and lower regions of the gland, respectively. The superior thyroid artery arises as the 1st branch of the external carotid artery, typically near the level of the superior horn of the thyroid cartilage. This blood vessel descends almost vertically, accompanied by its paired vein, posterior to the sternothyroid muscle, and reaches the superior pole of the thyroid lobe. Distally, this artery gives rise to the infrahyoid, sternocleidomastoid, superior laryngeal, and cricothyroid branches. The superior laryngeal artery travels with the internal laryngeal nerve as it pierces the thyrohyoid membrane. The cricothyroid artery anastomoses with its contralateral counterpart across the midline.[8]
The inferior thyroid artery originates from the thyrocervical trunk, which arises from the anterosuperior surface of the subclavian artery. This vessel branches near the medial border of the anterior scalene muscle and courses medially toward the posterior surface of the thyroid gland.[9] The artery typically reaches the lateral lobe at the junction of the lower 3rd of the outer border. The largest branch of the inferior thyroid artery is the ascending cervical artery, which must be distinguished from the main trunk of the inferior thyroid artery during surgical dissection.[10]
An additional artery, the thyroid ima artery, is present in approximately 10% of individuals. The origin of this blood vessel is highly variable, as it may diverge from the brachiocephalic trunk, aortic arch, right common carotid artery, subclavian artery, pericardiacophrenic artery, thyrocervical trunk, transverse scapular artery, or internal thoracic artery. However, the thyroid ima artery most commonly arises from the brachiocephalic trunk and supplies the isthmus and anterior surface of the thyroid gland.[11]
Venous drainage of the thyroid occurs through the superior, middle, and inferior thyroid veins. The superior and middle veins follow a tortuous course before draining into the internal jugular vein bilaterally. The inferior thyroid vein typically drains into the subclavian or brachiocephalic veins, just posterior to the manubrium (see Image. Thyroid Arteries, Veins, and Muscles).[12]
Lymphatic drainage involves the prelaryngeal, pretracheal, paratracheal, and lower deep cervical lymph nodes. The paratracheal and lower deep cervical nodes primarily receive drainage from the isthmus and inferior lateral lobes. The superior aspect of the gland drains into the superior pretracheal and cervical nodes.
Nerves
The autonomic nervous system provides the primary innervation of the thyroid gland. Parasympathetic input is delivered by branches of the vagus nerve, while sympathetic fibers arise from the superior, middle, and inferior cervical ganglia of the sympathetic trunk.[13] Although the autonomic nervous system does not regulate hormone production or secretion, it modulates thyroidal vascular tone.
Muscles
Several muscles form important landmarks in the surgical anatomy of the neck and thyroid region. The platysma is the most superficial, enclosed by the superficial cervical fascia and extending from the superficial fascia of the deltoid and clavicle to the mandible and face. The sternocleidomastoid, located anterolateral to the thyroid gland, defines the anterior boundary of the posterior cervical triangle and spans obliquely from the mastoid process to the clavicle and sternum. The digastric muscle originates at the mandibular tubercle, passes deep to the hyoid bone, and inserts onto the mastoid tip. The infrahyoid or strap muscles comprise 4 paired muscles on the anterolateral surface of the thyroid gland and facilitate gross laryngeal movement during swallowing and vocalization.
The omohyoid lies deep to the sternocleidomastoid and extends from the hyoid bone to the lateral clavicle. The sternohyoid occupies a superficial position over the thyroid gland, extending from the hyoid to the sternum. The sternothyroid spans from the oblique line of the thyroid cartilage to the sternum and lies directly over the anterior thyroid surface. The thyrohyoid runs from the oblique line of the thyroid cartilage to the hyoid bone. The inferior pharyngeal constrictor originates from the thyroid and cricoid cartilages and inserts onto the pharyngeal raphe, contacting the superior medial aspect of the thyroid lobe.[14]
Physiologic Variants
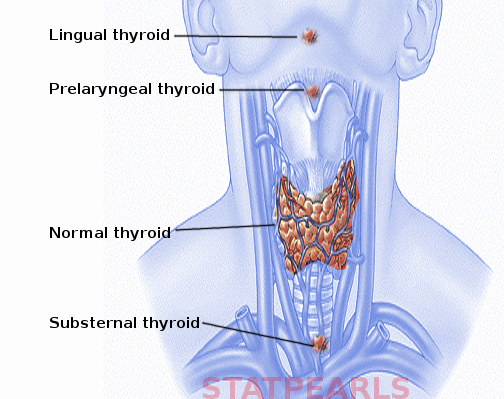
Ectopic thyroid tissue may occur anywhere along the embryologic migratory pathway, with documented locations ranging from the tongue to the diaphragm (see Image. Ectopic Thyroid). The prevalence of ectopic thyroid tissue ranges from 1 per 100,000 to 1 per 300,000 individuals.[15][16] The most frequent site is the lingual thyroid at the base of the tongue.[17]
A pyramidal lobe may project superiorly from the isthmus as a vestigial remnant of the thyroglossal duct. This variant occurs in 28% to 55% of individuals, most often arising from the left side.[18] The pyramidal lobe may exist bilaterally or as a separate structure from the main gland.
Additional morphologic variations are frequently observed.[19] The isthmus may be prominent, narrowed, or absent altogether. Asymmetry and size variation between lateral lobes are commonly observed.
Surgical Considerations
Several critical anatomical relationships must be considered during total thyroidectomy, thyroid lobectomy, or excision of a thyroglossal duct cyst.[20][21] Preoperative chest radiography or mediastinal computed tomography is indicated when anatomic distortion or substernal thyroid extension is suspected. Slight neck extension on the operating table improves surgical access to the cervical region. A curvilinear skin incision, typically positioned 1 to 2 fingerbreadths above the clavicle, provides appropriate exposure. The incision follows a natural skin crease or lies parallel to one.
Recurrent Laryngeal Nerve
Two nerves of surgical importance that course near the thyroid gland are the right and left RLNs. These nerves typically run along the lateral aspect of the thyroid gland in proximity to the inferior thyroid artery. Intraoperative identification and preservation of the RLNs are essential to prevent nerve injury. The nerves may be exposed inferior to the inferior thyroid artery or after mobilizing the superior and inferior poles of the gland.
Each RLN is most susceptible to injury along its distal 2 to 3 cm, where it is frequently obscured by the tubercle of Zuckerkandl, a posterior pyramidal projection of each thyroid lobe, and the Berry ligament. Retraction of the tubercle of Zuckerkandl medially often reveals the RLN, which typically courses just medial to the tubercle and remains concealed without careful dissection. The distal RLN is more reliably visualized during total lobectomy than during subtotal lobectomy, where full exposure is not always feasible.
An anatomic variant, the nonrecurrent laryngeal nerve or a direct vagal branch, is identified on the right side in approximately 1% of individuals, often after retraction of the tubercle of Zuckerkandl. Additional variability includes RLN bifurcation or trifurcation near the laryngeal entry point. Every branch within the Berry ligament must be preserved to avoid inadvertent transection or clamping.
Thermal injury from electrocautery applied too close to the nerve poses another risk, even in the absence of direct trauma. Such injury often presents without immediate visual cues, making intraoperative vigilance essential.
Superior Laryngeal Nerve
Dissection of the superior pole of the thyroid gland may expose the superior laryngeal nerve (SLN), which frequently courses adjacent to the superior thyroid artery. High ligation of the artery increases the risk of injuring the SLN, particularly its external branch. Approximately 20% of patients are vulnerable to SLN injury when the superior thyroid vessels are clamped, divided, and ligated en masse. Dividing the artery as it enters the thyroid capsule minimizes this risk. Most surgeons do not require direct visualization of the SLN during dissection.
Beyond mechanical trauma, excessive use of electrocautery can result in thermal injury and paresis. Electrocautery must not be used for hemostasis near the cricothyroid or inferior pharyngeal constrictor muscles due to the risk of heat transmission to adjacent nerves. Bipolar cautery, while more precise, still warrants caution. The anterior suspensory ligament may adhere to the cricothyroid muscle. Dissection in this region requires care to avoid muscle injury.
Cervical Sympathetic Trunk
Injury to the cervical sympathetic trunk is uncommon. However, the risk increases during mobilization of the carotid sheath to access retroesophageal goiters or malignant extensions.
Clinical Significance
Diseases and anomalies of the thyroid gland and subsequent surgeries can result in various presentations and complications that bear clinical significance.[22] A thorough understanding of thyroid anatomy and pathology guides accurate diagnosis and appropriate intervention.
Hyperthyroidism
Excess thyroid hormone production may arise from autoimmune or neoplastic processes. Graves disease accounts for most cases and involves autoantibodies targeting the thyroid-stimulating hormone receptor.[23] Common symptoms include heat intolerance, excessive sweating, tachycardia, palpitations, anxiety, unintentional weight loss, tremor, menstrual irregularities, and ocular findings such as exophthalmos and diplopia. Treatment depends on comorbidities, disease severity, and patient preference, and may include pharmacological or surgical approaches.
Hypothyroidism
Insufficient thyroid hormone levels may lead to nonspecific or insidious symptoms. Common findings include weight gain, cold intolerance, constipation, dry skin, fatigue, menstrual disturbances, and depressed mood. Autoimmune destruction of follicular cells, often affecting women at rates up to 7 times higher than men, is a common cause. Hormone replacement and periodic monitoring result in effective long-term management.[24]
Goiter
Goiter refers to thyroid gland enlargement, ranging from mild asymmetry to massive growth that causes airway compression (see Image. Goiter in a Woman). Common etiologies include iodine deficiency, hyperthyroidism, and hypothyroidism.[25]
Consequences of Ectopic Thyroid Tissue
Ectopic thyroid tissue produces symptoms based on location. Lingual thyroid may cause dysphagia, bleeding, or respiratory distress. Suprahyoid and infrahyoid thyroid tissue often presents as a midline neck mass, resembling a thyroglossal duct cyst. Intraluminal thyroid tissue in the trachea or larynx can lead to airway obstruction, while esophageal involvement may cause dysphagia. Pyramidal lobes are typically asymptomatic, as are ectopic thyroid tissues located in the aorta, pericardium, or myocardium.
Media
(Click Image to Enlarge)
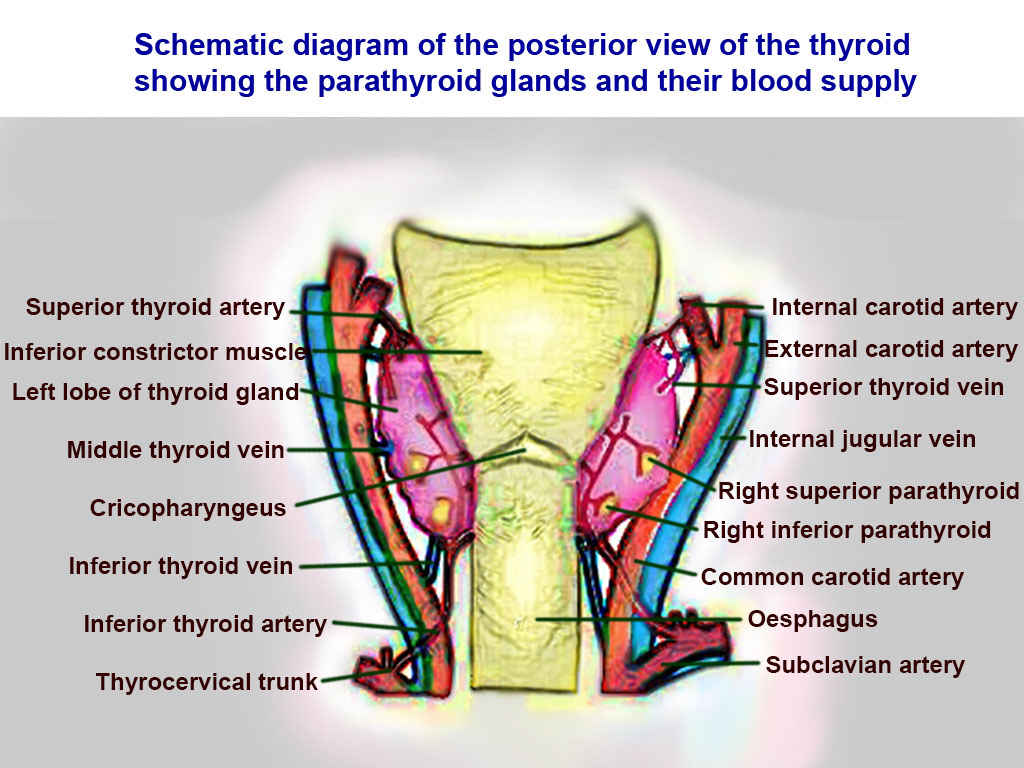
Thyroid Arteries, Veins, and Muscles. Posterior view of thyroid includes superior thyroid, inferior constrictor, left lobe of thyroid, middle thyroid vein, cricopharyngeaus, inferior thyroid vein, inferior thyroid vein, inferior thyroid artery, thyrocervical trunk, internal carotid, external carotid, superior thyroid, internal jugular, right superior parathyroid, right inferior parathyroid, common carotid, oesphagus, and subclavian.
Contributed by T Silappathikaram
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Chaker L, Razvi S, Bensenor IM, Azizi F, Pearce EN, Peeters RP. Hypothyroidism. Nature reviews. Disease primers. 2022 May 19:8(1):30. doi: 10.1038/s41572-022-00357-7. Epub 2022 May 19 [PubMed PMID: 35589725]
Lee SY, Pearce EN. Hyperthyroidism: A Review. JAMA. 2023 Oct 17:330(15):1472-1483. doi: 10.1001/jama.2023.19052. Epub [PubMed PMID: 37847271]
Turcios S, Lence-Anta JJ, Santana JL, Pereda CM, Velasco M, Chappe M, Infante I, Bustillo M, García A, Clero E, Maillard S, Rodriguez R, Xhaard C, Ren Y, Rubino C, Ortiz RM, de Vathaire F. Thyroid volume and its relation to anthropometric measures in a healthy cuban population. European thyroid journal. 2015 Mar:4(1):55-61. doi: 10.1159/000371346. Epub 2015 Feb 26 [PubMed PMID: 25960963]
Norris CD, Anzai Y. Anatomy of Neck Muscles, Spaces, and Lymph Nodes. Neuroimaging clinics of North America. 2022 Nov:32(4):831-849. doi: 10.1016/j.nic.2022.07.027. Epub 2022 Sep 21 [PubMed PMID: 36244726]
Kapral N, Khot R. Thyroid anatomy and ultrasound evaluation. Techniques in vascular and interventional radiology. 2022 Jun:25(2):100818. doi: 10.1016/j.tvir.2022.100818. Epub 2022 Mar 10 [PubMed PMID: 35551809]
Mantalovas S, Sapalidis K, Manaki V, Magra V, Laskou S, Pantea S, Lagopoulos V, Kesisoglou I. Surgical Significance of Berry's Posterolateral Ligament and Frequency of Recurrent Laryngeal Nerve Injury into the Last 2 cm of Its Caudal Extralaryngeal Part(P1) during Thyroidectomy. Medicina (Kaunas, Lithuania). 2022 Jun 1:58(6):. doi: 10.3390/medicina58060755. Epub 2022 Jun 1 [PubMed PMID: 35744018]
Lesi OK, Thapar A, Appaiah NNB, Iqbal MR, Kumar S, Maharaj D, Saad Abdalla Al-Zawi A, Dindyal S. Thyroid Hemiagenesis: Narrative Review and Clinical Implications. Cureus. 2022 Feb:14(2):e22401. doi: 10.7759/cureus.22401. Epub 2022 Feb 20 [PubMed PMID: 35371763]
Level 3 (low-level) evidenceTzortzis AS, Antonopoulos I, Pechlivanidou E, Chrysikos D, Pappas N, Troupis T. Anatomical variations of the superior thyroid artery: A systematic review. Morphologie : bulletin de l'Association des anatomistes. 2023 Sep:107(358):100597. doi: 10.1016/j.morpho.2023.03.002. Epub 2023 Apr 13 [PubMed PMID: 37061377]
Level 1 (high-level) evidenceBunea MC, Rusali LM, Bratu IC, Tudorache S, Bordei P. Considerations on the origin of the inferior thyroid artery emerging from the subclavian artery determined by CT examination. Surgical and radiologic anatomy : SRA. 2023 Jun:45(6):721-727. doi: 10.1007/s00276-023-03140-9. Epub 2023 Apr 4 [PubMed PMID: 37014432]
Roman BR, Randolph GW, Kamani D. Conventional Thyroidectomy in the Treatment of Primary Thyroid Cancer. Endocrinology and metabolism clinics of North America. 2019 Mar:48(1):125-141. doi: 10.1016/j.ecl.2018.11.003. Epub [PubMed PMID: 30717897]
Bunea MC, Rusali LM, Tudorache SI, Bratu IC, Bordei P. Considerations on the morphology of the thyroid ima artery. Surgical and radiologic anatomy : SRA. 2024 Jan:46(1):91-99. doi: 10.1007/s00276-023-03268-8. Epub 2023 Nov 22 [PubMed PMID: 37991506]
Singh R. Variations of venous drainage of the thyroid gland and their surgical implications: a narrative review. Jornal vascular brasileiro. 2023:22():e20220163. doi: 10.1590/1677-5449.202201632. Epub 2023 Apr 11 [PubMed PMID: 37143504]
Level 3 (low-level) evidenceSaylam CY, Ozgiray E, Orhan M, Cagli S, Zileli M. Neuroanatomy of cervical sympathetic trunk: a cadaveric study. Clinical anatomy (New York, N.Y.). 2009 Apr:22(3):324-30. doi: 10.1002/ca.20764. Epub [PubMed PMID: 19173257]
Agcaoglu O, Sucu S, Toprak S, Tezelman S. Techniques for Thyroidectomy and Functional Neck Dissection. Journal of clinical medicine. 2024 Mar 26:13(7):. doi: 10.3390/jcm13071914. Epub 2024 Mar 26 [PubMed PMID: 38610679]
Gao M, He Q, Li L, Ji F, Ding Y, Sun Q, Qiu X. The clinicopathological features, treatment outcomes and follow-up results of 47 ectopic thyroid gland cases: a single-center retrospective study. Frontiers in endocrinology. 2023:14():1278734. doi: 10.3389/fendo.2023.1278734. Epub 2023 Nov 24 [PubMed PMID: 38075053]
Level 2 (mid-level) evidenceTsai A, Rafferty W, Ren S. Mediastinal ectopic thyroid tissue, an imitator of an enlarged lymph node with metastatic pulmonary neoplasia. Diagnostic cytopathology. 2021 Dec:49(12):E471-E474. doi: 10.1002/dc.24866. Epub 2021 Sep 7 [PubMed PMID: 34492168]
Patel S, Bhatt AA. Thyroglossal duct pathology and mimics. Insights into imaging. 2019 Feb 6:10(1):12. doi: 10.1186/s13244-019-0694-x. Epub 2019 Feb 6 [PubMed PMID: 30725193]
Ranade AV, Rai R, Pai MM, Nayak SR, Prakash, Krisnamurthy A, Narayana S. Anatomical variations of the thyroid gland: possible surgical implications. Singapore medical journal. 2008 Oct:49(10):831-4 [PubMed PMID: 18946620]
Al-Azzawi A, Takahashi T. Anatomical variations of the thyroid gland: An experimental cadaveric study. Annals of medicine and surgery (2012). 2021 Oct:70():102823. doi: 10.1016/j.amsu.2021.102823. Epub 2021 Sep 8 [PubMed PMID: 34691414]
Wiersinga WM. Graves' Disease: Can It Be Cured? Endocrinology and metabolism (Seoul, Korea). 2019 Mar:34(1):29-38. doi: 10.3803/EnM.2019.34.1.29. Epub [PubMed PMID: 30912336]
Rovira A, Nixon IJ, Simo R. Papillary microcarcinoma of the thyroid gland: current controversies and management. Current opinion in otolaryngology & head and neck surgery. 2019 Apr:27(2):110-116. doi: 10.1097/MOO.0000000000000520. Epub [PubMed PMID: 30844924]
Level 3 (low-level) evidenceNaytah M, Ibrahim I, da Silva S. Importance of incorporating intraoperative neuromonitoring of the external branch of the superior laryngeal nerve in thyroidectomy: A review and meta-analysis study. Head & neck. 2019 Jun:41(6):2034-2041. doi: 10.1002/hed.25669. Epub 2019 Feb 1 [PubMed PMID: 30706616]
Level 1 (high-level) evidenceDavies TF, Andersen S, Latif R, Nagayama Y, Barbesino G, Brito M, Eckstein AK, Stagnaro-Green A, Kahaly GJ. Graves' disease. Nature reviews. Disease primers. 2020 Jul 2:6(1):52. doi: 10.1038/s41572-020-0184-y. Epub 2020 Jul 2 [PubMed PMID: 32616746]
Klubo-Gwiezdzinska J, Wartofsky L. Hashimoto thyroiditis: an evidence-based guide to etiology, diagnosis and treatment. Polish archives of internal medicine. 2022 Mar 30:132(3):. pii: 16222. doi: 10.20452/pamw.16222. Epub 2022 Mar 3 [PubMed PMID: 35243857]
Etiopathology, clinical features, and treatment of diffuse and multinodular nontoxic goiters., Knobel M,, Journal of endocrinological investigation, 2016 Apr [PubMed PMID: 26392367]