Introduction
Subungual hematomas result from bleeding beneath the nail due to nail bed injury (see Image. Subungual Hematoma). Patients typically report pain and nail discoloration. Direct blows or crush injuries to the distal phalanx, such as pinching a finger in a doorway, often cause this damage. Accumulating blood increases pressure on the nail bed, causing significant pain. Associated injuries include distal phalanx fractures, nail avulsion, or fingertip avulsions. Simple trephination, which involves creating a small hole in the nail, typically relieves most hematomas.[1][2][3][4] Larger hematomas or those with suspected underlying nail bed lacerations require removal of the nail plate and direct repair of the nail bed. Prompt assessment and intervention provide pain relief and reduce the risk of long-term complications, including nail dystrophy and infection.[5]
Physical Examination
The entire nail structure should be examined for disruption of the nail fold, and the whole finger should be assessed for motor function, sensation, and circulation. The extensor mechanism of the distal interphalangeal joint should be evaluated by holding the middle phalanx and testing the strength of extension by applying resistance to the motion. A decrease in strength compared to the contralateral side indicates mallet finger injury. Circulation should be tested by assessing capillary refill distal to the injury. In some patients, such as small children, a digital nerve block may be performed to facilitate examination and reduce discomfort. A thorough neurovascular assessment is essential to rule out associated injuries that may require urgent surgical intervention.[6]
Testing
Three-view radiographs should be obtained to evaluate for underlying fractures, as distal tuft fractures are commonly associated with them. Point-of-care ultrasound may be used to identify nail bed lacerations and underlying distal tuft fractures that suggest the need for a more involved repair. This imaging modality has emerged as a valuable tool, providing real-time visualization and aiding in decision-making regarding nail plate removal and formal nail bed repair, particularly when clinical suspicion for significant nail bed laceration is high.[7]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
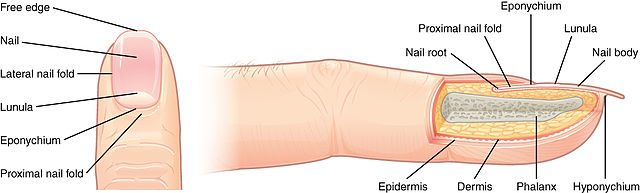
The complete nail structure, called the "perionychium," is composed of the following (see Image. Nail Anatomy):
- Nail fold: Skin that frames and protects the sides and base of the nail
- Paronychium: Dorsal skin of the fingertip
- Hyponychium: Keratinized distal end of the nail bed in contact with the fingertip skin
- Nail bed: Tissue beneath the nail plate, composed of the germinal and sterile matrices, supporting nail growth
- Nail: Hard, protective keratin plate covering the dorsal surface of the fingertip
The germinal matrix, located on the ventral floor of the proximal nail fold, produces approximately 90% of nail cells and extends to the lunula, the crescent-shaped lighter portion of the nail. The sterile matrix, highly vascularized and situated on the ventral floor of the distal nail bed, contributes layers of cells that secure the nail to the nail bed. A thorough understanding of nail unit anatomy is essential for recognizing the risks of immediate and delayed complications after trauma, including permanent nail deformity resulting from severe damage to the germinal matrix.
Indications
Current recommendations for managing acute subungual hematomas within 48 hours of injury support trephination, a procedure in which a hole is created in the nail to evacuate the hematoma. Earlier guidelines recommended nail plate removal for hematomas involving more than 50% of the nail surface, or more than 25% in the presence of an associated fracture. However, results from multiple studies have demonstrated that trephination yields comparable cosmetic outcomes and complication rates in most cases.[8][9][10][11][12]
Evidence increasingly suggests that nail avulsion and repair, even for large hematomas without displaced fractures or significant nail fold disruption, may not improve outcomes and could potentially increase procedural risk. The emphasis has shifted toward conservative management for uncomplicated cases, regardless of hematoma size, with a priority on pain relief and patient comfort. Nail plate removal and formal nail bed repair are indicated only in the presence of a significant nail bed laceration, displaced distal phalanx fracture, or nail avulsion involving the nail fold.
Contraindications
Trephination carries no absolute contraindications. However, certain cases warrant consideration of nail removal and nail bed repair to optimize cosmetic outcomes. Subungual hematoma accompanied by nail avulsion, a displaced distal phalanx fracture, or a proximal fracture involving the germinal matrix typically requires surgical consultation for nail removal and nail bed repair. Trephination offers no benefit in cases of nontraumatic subungual hematoma. Such cases may arise from underlying tumors, including junctional nevi, melanoma, or splinter hemorrhages. Distinguishing traumatic subungual hematomas from conditions that mimic them, such as glomus tumors, onychomycosis, or subungual exostosis, is crucial, as each requires a distinct diagnostic and therapeutic approach.[13][14]
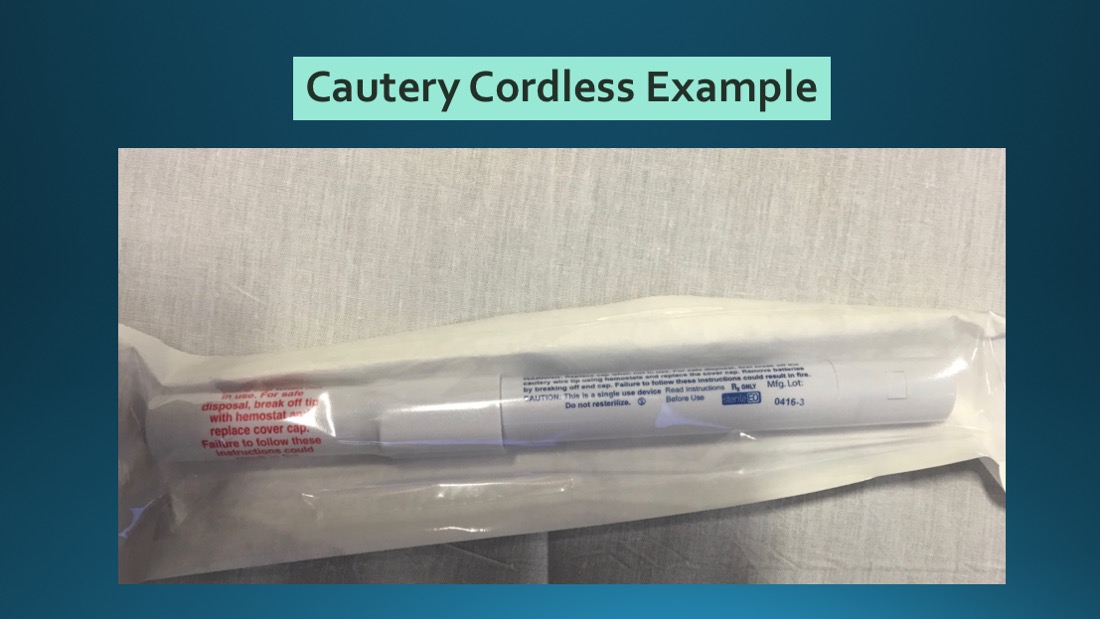
Equipment
Necessary supplies for this procedure include personal protective equipment, such as a face mask with eye shield and gloves. For a digital block, the required items are a 25-gauge needle, a 3-mL syringe, 1% lidocaine, a topical antiseptic, and gauze. Trephination may be performed using an electrocautery device or an 18-gauge needle (see Image. Cordless Cautery Device). In resource-limited settings, a heated paper clip may suffice. When nail plate removal and nail bed repair are indicated, additional instruments such as fine-tipped forceps, nail scissors, and fine absorbable sutures (eg, 6-0 or 7-0 chromic gut) should be prepared. Adherence to sterile technique is crucial in reducing the risk of procedural infection.
Personnel
The procedure may be performed by emergency medicine or primary care clinicians, as well as plastic and orthopedic surgeons. Nurses contribute significantly by assisting with preparation, ensuring patient comfort, and providing postprocedure education.[15]
Preparation
The affected digit should be cleaned using chlorhexidine or povidone-iodine solution. A digital block may be administered for patients with distal phalanx fractures, although it often causes more discomfort than the trephination itself. Informed consent must be obtained before the procedure commences. The patient should be informed that bleeding from the trephination site is expected and that potential complications include nail loss, hematoma reaccumulation, and infection.
For cases requiring nail plate removal and repair, counseling should be provided regarding the longer recovery period, the importance of meticulous dressing care, and the risks of temporary or permanent nail deformity. Patients should be educated about anticipated postprocedure discomfort, the expected appearance of the draining hematoma, and signs of complications to ensure appropriate expectations and adequate follow-up.
Technique or Treatment
Trephination techniques aim to relieve pressure by creating a small opening in the nail plate to drain accumulated blood. Several methods may be used, depending on the available tools, including electrocautery, needle puncture, or improvised means such as a heated paper clip. When using handheld electrocautery, the device should be applied perpendicular (at a 90° angle) to the nail surface, directly over the central portion of the hematoma. The heat melts a small hole through the nail plate, allowing blood to escape. A capillary tube, such as a heparinized hematocrit tube, may assist in drawing out the hematoma. However, electrocautery is generally contraindicated when acrylic nails are present due to the risk of ignition.[16]
For the needle method, an 18-gauge needle is positioned at a 90° angle over the hematoma and rotated in a drilling fashion to create a hole. In young patients or when using smaller-gauge needles, multiple perforations may be necessary to achieve adequate drainage. In the absence of standard equipment, a heated paper clip may be used. After heating the paper clip until it becomes red-hot, it is gently applied at a 90° angle to the nail over the hematoma, burning a small hole through which blood can escape.
Once the opening is made, drainage typically relieves most of the patient’s pain. In some cases, more than 1 trephination procedure may be needed to decompress the hematoma completely. Care must be taken to avoid advancing too deeply and damaging the underlying nail bed. The site should be bandaged with sterile gauze, and the patient instructed to keep the area clean and dry. The choice of trephination method often depends on provider preference and the available resources, but the goal remains consistent: to create an opening sufficient for complete drainage while minimizing trauma to the nail unit.
After administering a digital nerve block and performing sterile preparation, the nail plate is carefully elevated from the surrounding nail folds to allow for inspection of the nail bed for lacerations. Any identified lacerations are meticulously repaired using fine absorbable sutures. When available, the removed nail plate may be trimmed and repositioned within the nail folds to serve as a stent, maintaining the nail fold space and guiding new nail growth. Alternatively, a nonadherent dressing may be applied to fulfill a similar role. Finally, the finger is dressed with a protective bandage to complete the procedure.
Complications
Follow-up instructions should be provided, advising the patient to avoid soaking the finger to prevent bacterial contamination. Patients should be informed that blood may continue to ooze from the nail hole for 1 to 2 days. Reevaluation is recommended if signs of infection develop, including warmth, redness, increasing swelling, fever, or if the hematoma reaccumulates with pain.
Nondisplaced distal phalanx fractures require immobilization in an extension splint for 4 weeks, with follow-up arranged with a hand specialist. Patients should be advised that the hematoma typically advances distally over several weeks. Lack of progression warrants evaluation by a dermatologist to rule out abnormal tissue growth, such as melanoma or a nevus. Current evidence does not support routine use of postprocedure antibiotics, as a small observational study of 47 patients found no benefit.[17]
Although complications are generally rare when proper technique is used, long-term issues such as nail deformity (onychodystrophy) or onycholysis (nail separation from the nail bed) may occur, particularly following severe injuries or inadequate drainage. Patient education about potential delayed complications is essential, especially after nailbed repair, given the increased risk of nail growth abnormalities.
Clinical Significance
This injury frequently presents in both pediatric and adult populations and occurs commonly in austere environments. Employing multiple strategies, including nonspecialized methods, facilitates prompt and adequate treatment. Effective management alleviates acute pain while preserving nail health and function, reducing the risk of chronic deformities that affect daily activities and appearance.
Enhancing Healthcare Team Outcomes
Managing subungual hematomas often involves emergency department clinicians, primary care clinicians, or surgeons, with nurses assisting in finger stabilization. Ensuring the hematoma is less than 48 hours old is crucial. Most hematomas may be safely drained using a large needle without complications.
Patient follow-up is crucial to confirm resolution and rule out any potential infection. An interprofessional team, including clinicians, nurses, and, for complex cases, hand therapists, optimizes outcomes through comprehensive evaluation, appropriate interventions such as trephination or nailbed repair, and thorough patient education on wound care and follow-up. Clear communication among team members streamlines care and reduces the risk of complications.
Nursing, Allied Health, and Interprofessional Team Interventions
Nurses play a critical role in educating patients about wound care, pain management, and recognizing signs of infection or hematoma reaccumulation. Nurses assist in preparing the sterile field and ensure patient comfort throughout the procedure. Allied health professionals, such as hand therapists, play a crucial role in postprocedural rehabilitation, particularly in complex cases or those involving fractures or nailbed repairs, to optimize hand function and minimize the risk of long-term stiffness or deformity.
Nursing, Allied Health, and Interprofessional Team Monitoring
Monitoring requires assessment of the trephination or nailbed repair site for signs of infection, including redness, swelling, and purulent discharge. Reaccumulation of the hematoma, causing persistent pain, should be evaluated, along with the proper healing of the nail bed. Patients must be advised to observe the hematoma’s progression as the nail grows and report any changes in nail appearance or discomfort. In cases involving underlying fractures or significant nailbed repairs, monitoring fracture healing, adherence to splinting protocols, and evaluation for persistent nail deformities are essential.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Garcia-Rodriguez JA. Draining a subungual hematoma: procedures and assessments video series. Canadian family physician Medecin de famille canadien. 2013 Aug:59(8):853 [PubMed PMID: 23946029]
Khan MA, West E, Tyler M. Two millimetre biopsy punch: a painless and practical instrument for evacuation of subungual haematomas in adults and children. The Journal of hand surgery, European volume. 2011 Sep:36(7):615-7. doi: 10.1177/1753193411414629. Epub 2011 Jul 1 [PubMed PMID: 21724686]
Level 3 (low-level) evidenceKain N, Koshy O. Evacuation of subungual haematomas using punch biopsy. Journal of plastic, reconstructive & aesthetic surgery : JPRAS. 2010 Nov:63(11):1932-3. doi: 10.1016/j.bjps.2010.03.023. Epub 2010 Mar 31 [PubMed PMID: 20359972]
Level 3 (low-level) evidenceCohen PR, Schulze KE, Nelson BR. Subungual hematoma. Dermatology nursing. 2007 Feb:19(1):83-4 [PubMed PMID: 17330560]
Level 3 (low-level) evidenceAkella A, Daniel AR, Gould MB, Mangal R, Ganti L. Subungual Hematoma. Cureus. 2023 Nov:15(11):e48952. doi: 10.7759/cureus.48952. Epub 2023 Nov 17 [PubMed PMID: 38111403]
Braga Silva J. Fingernail injury in children. Hand surgery & rehabilitation. 2024 Apr:43S():101512. doi: 10.1016/j.hansur.2023.01.001. Epub 2023 Jan 20 [PubMed PMID: 36682538]
Gungor F, Akyol KC, Eken C, Kesapli M, Beydilli I, Akcimen M. The value of point-of-care ultrasound for detecting nail bed injury in ED. The American journal of emergency medicine. 2016 Sep:34(9):1850-4. doi: 10.1016/j.ajem.2016.06.067. Epub 2016 Jun 18 [PubMed PMID: 27358042]
Salter SA, Ciocon DH, Gowrishankar TR, Kimball AB. Controlled nail trephination for subungual hematoma. The American journal of emergency medicine. 2006 Nov:24(7):875-7 [PubMed PMID: 17098113]
Level 3 (low-level) evidenceSkinner PB Jr. Management of traumatic subungual hematoma. American family physician. 2005 Mar 1:71(5):856 [PubMed PMID: 15768614]
Level 3 (low-level) evidenceRichardson M. Selecting a treatment option in subungual haematoma management. Nursing times. 2004 Nov 16-22:100(46):59, 61, 63 [PubMed PMID: 15595491]
Scott PM. Subungual hematoma evacuation. JAAPA : official journal of the American Academy of Physician Assistants. 2002 Mar:15(3):63-5 [PubMed PMID: 11949545]
Roser SE, Gellman H. Comparison of nail bed repair versus nail trephination for subungual hematomas in children. The Journal of hand surgery. 1999 Nov:24(6):1166-70 [PubMed PMID: 10584937]
Santoshi JA, Kori VK, Khurana U. Glomus tumor of the fingertips: A frequently missed diagnosis. Journal of family medicine and primary care. 2019 Mar:8(3):904-908. doi: 10.4103/jfmpc.jfmpc_88_19. Epub [PubMed PMID: 31041222]
Altarifi ME, Kalas A, Alnajjar A, Yasin Dali M, Alkhowailed MS. Glomus tumor: A rare differential diagnosis for subungual lesions. Radiology case reports. 2024 Dec:19(12):6034-6038. doi: 10.1016/j.radcr.2024.08.116. Epub 2024 Sep 19 [PubMed PMID: 39345850]
Level 3 (low-level) evidenceLafreniere AS, Misati G, Knox A. Approach to nail trauma for primary care physicians. Canadian family physician Medecin de famille canadien. 2023 Sep:69(9):609-613. doi: 10.46747/cfp.6909609. Epub [PubMed PMID: 37704235]
Blereau C, Radloff S, Grisham J. Up in Flames: The Safety of Electrocautery Trephination of Subungual Hematomas with Acrylic Nails. The western journal of emergency medicine. 2022 Feb 23:23(2):183-185. doi: 10.5811/westjem.2021.10.53567. Epub 2022 Feb 23 [PubMed PMID: 35302451]
Seaberg DC, Angelos WJ, Paris PM. Treatment of subungual hematomas with nail trephination: a prospective study. The American journal of emergency medicine. 1991 May:9(3):209-10 [PubMed PMID: 2018587]