Introduction
The goal of stapes surgery is to restore normal transmission of acoustic vibrations to the cochlear fluid when stapes footplate fixation disrupts this process. Improved sound conduction significantly enhances quality of life by restoring auditory perception and enabling effective communication.[1][2] The origins of stapedectomy trace back to 1892, when Frederick L Jack performed a bilateral procedure on a patient who reportedly retained hearing 10 years postoperatively.[3] In the early 1950s, John J Shea Jr recognized the potential of stapes surgery and introduced the concept of using a prosthesis to replicate stapes function. On May 1, 1956, Dr Shea performed the first successful stapedectomy using a Teflon prosthesis in a patient with otosclerosis.[4]
The primary goal when operating on the stapes is to reestablish sound transmission through an ossicular chain stiffened by otosclerosis, a disease process characterized by absorption of compact bone and redeposition of spongiotic bone within the otic capsule.[5] Otosclerosis is the most common cause of acquired conductive hearing loss (CHL) that results in stapes fixation.[6] The condition presents as a progressive, insidious form of CHL. Affected individuals often experience difficulties with having conversations, particularly while chewing, and may perceive speech more clearly in noisy environments than in quiet ones—a phenomenon known as paracusis of Willis.
Otoscopic examination may reveal a red blush or discoloration over the promontory of the basal turn of the cochlea in approximately 10% of cases.[7] This finding, when it does not blanch with pneumatic otoscopy, is referred to as the "Schwartze sign." The absence of this sign does not exclude the diagnosis. In some cases, the sign only becomes apparent after elevation of the tympanomeatal flap and direct visualization of the middle ear cleft during surgery.[8]
As detailed in the review by Markou and Goudakos, the etiology of otosclerosis remains unknown, though both genetic and environmental factors are believed to contribute. Otosclerosis is classically inherited as an autosomal dominant trait with incomplete penetrance and is associated with 9 chromosomal loci, including COL1A1 and OTSC1 through OTSC8. The disease primarily affects White individuals, comprising up to 12% of the population, although only 0.3% to 0.4% develop clinical symptoms. A sex-based predisposition has been observed, with a female-to-male ratio of 1.5:1 to 2:1, and pregnancy has been reported to accelerate hearing loss progression, suggesting a hormonal influence.[9][10][11]
Stapedectomy and stapedotomy address the CHL associated with otosclerosis by reestablishing transmission of acoustic energy through the stapes footplate to the oval window and subsequently to the perilymph in the scala vestibuli.[12] Procedural success is typically assessed by the degree of air-bone gap (ABG) closure on audiometric evaluation.[13][14][15] The ABG is calculated as the difference between air and bone conduction thresholds, using a pure-tone average across 0.5, 1, 2, and 4 kHz. Surgical intervention is usually considered when the ABG measures 20 to 30 dB, although patients with smaller gaps may also benefit. The primary goal is to reduce the ABG to 10 dB or less.[16]
Multiple studies have compared stapedectomy, which involves the removal of the stapes superstructure and all or most of the footplate, with stapedotomy. This procedure entails removing the superstructure and creating a small fenestra in the footplate to accommodate a prosthesis that transmits vibrations from the incus to the oval window membrane. Results from these studies have found no significant difference between the 2 techniques in achieving closure of the ABG.[17][18][19] The most reliable predictors of successful surgical outcomes are the surgeon’s experience and willingness to adopt evolving techniques and technologies in stapes surgery.[20]
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
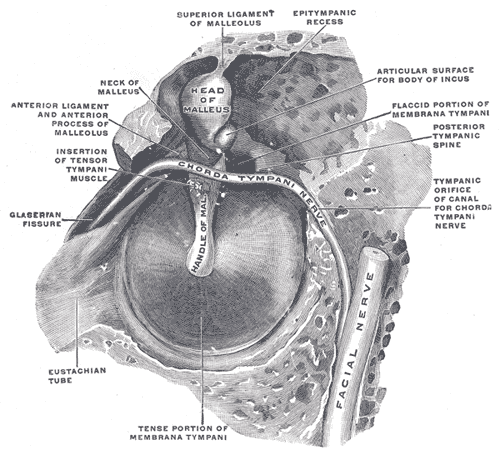
The temporal bone is classically divided into 4 parts: squamous, tympanic, mastoid, and petrous. The styloid process arises from the petrous portion as a bony projection. The tympanic portion primarily forms the bony medial two-thirds of the external auditory canal, while the middle and inner ears are housed within the petrous portion. Working from the outside in, a surgeon would first visualize the external ear, which consists of the pinna, the external auditory canal (the lateral third, of which is supported by cartilage, known as the "membranous" portion, and the medial two-thirds are supported by the tympanic portion of the temporal bone), and the tympanic membrane. The tympanic membrane is covered in keratinized, stratified, squamous epithelium laterally and mucosa medially. The mucosa adheres to the long process, or manubrium, of the malleus, which is visible through the eardrum as the umbo.
Between the epithelial layers lie radially and circumferentially oriented fibrous layers that provide strength to the pars tensa, the portion of the eardrum inferior to the level of the lateral process of the malleus, which protrudes toward the examiner under otoscopy (see Image. Right Tympanic Membrane, Otoscopic View). The pars tensa thickens into a peripheral band, the tympanic annulus, where it meets the bone of the external auditory canal. This structure supports the membrane and anchors it within the shallow tympanic sulcus along its perimeter.
Superior to the pars tensa lies the pars flaccida, or membrane of Shrapnell, which lacks a fibrous layer and the structural support of the tympanic annulus, rendering it more susceptible to retraction during Eustachian tube dysfunction. Rather than anchoring into a tympanic sulcus, the periphery of the pars flaccida aligns with the notch of Rivinus. This bony concavity contributes to the tympanic membrane’s slight eccentricity, approximately 9 to 10 mm in height and 8 to 9 mm in width. A line drawn along the manubrium of the malleus bisects the pars flaccida, designating the 12 o’clock position on otoscopic examination and dividing the membrane into anterior and posterior halves. A perpendicular line drawn through the midpoint further divides the tympanic membrane into superior and inferior quadrants. The stapes is located deep to the posterosuperior quadrant.
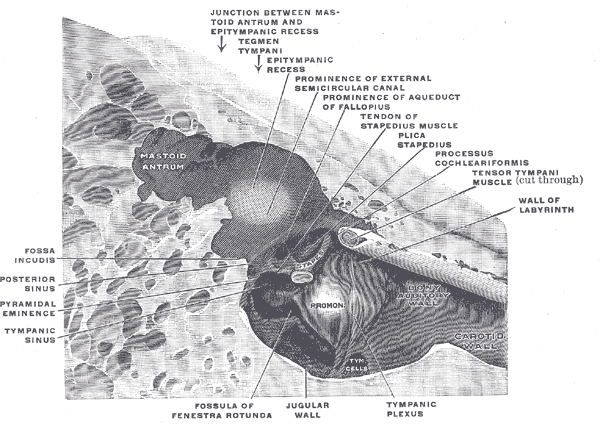
Medial to the tympanic membrane is the middle ear cavity, positioned directly beneath the floor of the middle cranial fossa. This space is the primary operative field during stapedectomy. The oval window membrane, occupied by the stapes footplate, marks the entrance to the inner ear. Enclosed within dense otic capsule bone, the inner ear contains the membranous labyrinth, which houses the cochlea, vestibule, saccule, utricle, and 3 semicircular canals.
Traversing the middle ear space from lateral to medial, the ossicular chain mechanically conveys sound pressure from the tympanic membrane to the cochlea (see Image. Right Auditory Ossicles). The malleus, the most lateral ossicle, adheres directly to the tympanic membrane. A synovial incudomalleolar joint connects the head of the malleus to the body of the incus, which possesses a long process that extends inferiorly to articulate with the capitulum (head) of the stapes at the incudostapedial joint. The stapes consists of a footplate and a superstructure. The footplate rests against the oval window membrane and is suspended by the annular ligament, transmitting auditory vibrations to the cochlea unless immobilized by otosclerosis. The superstructure includes the capitulum and the anterior and posterior crura. The stapedius tendon attaches to the posterior crus (see Image. Stapes).
The middle ear cleft, lined by respiratory epithelium composed of cuboidal and goblet cells, is ventilated by the eustachian tube, which connects the anterosuperior middle ear to the posterolateral nasopharynx. The middle ear is subdivided into the mesotympanum, epitympanum, and hypotympanum. Within the mesotympanum are the manubrium of the malleus, the stapes, the long process of the incus, the pyramidal eminence (from which the stapedius tendon emerges), the ponticulus (connecting the pyramidal eminence to the cochlear promontory), the chorda tympani nerve (protected by the scutum), a suprapyramidal recess known as the facial recess, and an infrapyramidal recess known as the sinus tympani (see Images. Medial and Adjacent Walls of the Right Tympanic Cavity and Middle Ear Anatomy, Right Side).
Above the mesotympanum is the epitympanum. The 2 structures are divided by a horizontal line drawn from the scutum to the tympanic segment of the facial nerve canal. A vertical crest of bone on the medial wall of the middle ear, known as the cog, further divides the epitympanum into anterior and posterior compartments. The cog extends from the tegmen tympani, the roof of the middle ear, to the cochleariform process, around which the tensor tympani muscle bends, and serves as an intraoperative landmark for the facial nerve. The posterior epitympanum contains the head of the malleus and the body of the incus. The hypotympanum lies inferior to the mesotympanum, with the boundary defined at the level of the inferior wall of the external auditory canal. This space varies considerably in size and may contain vascular anomalies such as a dehiscent jugular bulb or an aberrant carotid artery.
Indications
Stapes surgery for otosclerosis is considered when several criteria are met. The diagnosis must be confirmed, and the patient must be medically fit for the procedure, particularly if general anesthesia is required. A CHL of 25 dB or greater with a negative Rinne test at 512 Hz supports candidacy. A characteristic finding in otosclerosis is a “Carhart notch” at 2 kHz, an apparent ABG narrowing caused by diminished ossicular resonance rather than sensorineural deficit. A stiff or type As tympanogram may also be present, reflecting reduced tympanic membrane compliance without evidence of Eustachian tube dysfunction (see Image. Audiometric and Tympanometric Findings in Otosclerosis).
A negative Rinne test at 1,024 Hz indicates a more significant CHL and may further support surgical consideration. In CHL, tuning fork testing typically reveals louder perception by bone conduction than air conduction, known as a negative Rinne or “flipping the forks.” This finding is most reliable at 512 Hz, corresponding to a CHL of 20 to 30 dB.[21][22] In cases of mixed hearing loss, effective hearing aid use often requires reduction of the CHL through surgery.
Contraindications
Stapes surgery is contraindicated in the presence of the following conditions:
- Poor physical status that precludes tolerance of general anesthesia or the ability to remain still and responsive under local anesthesia with sedation
- Unilateral anacusis with otosclerosis affecting the only hearing ear
- Active infection involving the external auditory canal or middle ear
- Persistent vestibular symptoms, including those attributable to concomitant Ménière disease [23]
- Occupational need for uncompromised vestibular function (eg, commercial aviation)
- Presence of a persistent stapedial artery supplying primary cerebral circulation
Stapes surgery may be aborted intraoperatively under the following conditions:
- Identification of a persistent stapedial artery completely occupying the obturator foramen
- A low-lying facial nerve that obstructs surgical access to the stapes footplate.
- Complete obliteration of the oval window due to otosclerosis
- Drilling the oval window in such cases carries a high risk of sensorineural hearing loss.
Stapes surgery remains a technically demanding but highly effective treatment for CHL caused by otosclerosis. Careful patient selection, sound surgical judgment, and familiarity with anatomic and procedural nuances are critical to optimizing outcomes.
Equipment
Stapes surgery requires a complete set of middle ear instruments, including a sickle knife, House round knife, Bellucci scissors, Rosen pick, right-angle pick, Gimmick elevator, Alligator forceps, incudostapedial joint knife, fascia press, measuring probe, fine suction tips, and various sizes of otologic specula. Many surgeons favor the use of a speculum holder to facilitate the bimanual technique.
The entire procedure is performed under an operative microscope equipped with a 200- to 250-mm objective lens and a sterile drape. Removal of the stapes superstructure and either detachment or perforation of the footplate can be achieved using a microdrill or laser. Fiberoptically delivered lasers, typically argon, potassium titanyl phosphate, diode, or carbon dioxide, are commonly employed to limit vibratory acoustic trauma at the basal turn of the cochlea.[24][25][26][27][28] The selection of a stapes prosthesis depends on the surgeon’s familiarity and experience with a particular model.
Personnel
Working behind an operative microscope is essentially a single-surgeon endeavor. However, a skilled operating room scrub technician is essential to maintaining a seamless workflow. The technician enables the surgeon to remain focused through the microscope without diverting attention from the operative field.
An assistant may perform the harvest when graft material is required from a secondary site, such as a vein on the dorsum of the contralateral hand. Alternatively, the surgeon may use the temporalis fascia obtained before beginning the middle ear approach. In either scenario, the scrub technician is responsible for preparing, drying, and preserving the graft until it is needed later in the procedure.
Preparation
Semicircular canal dehiscence (SCD) or enlarged vestibular aqueduct (EVA) should be excluded while evaluating a patient for otosclerosis and a possible stapes procedure. These conditions may also present with a low-frequency CHL. Autophony or hyperacusis, along with vertigo induced by loud sounds or pressure changes (Tullio and Hennebert phenomena, respectively), may suggest a labyrinthine anomaly rather than otosclerosis.[29]
Acoustic reflex testing by an audiologist may help to differentiate labyrinthine anomalies, such as SCD, from ossicular chain pathology. A normal stapedius reflex is typically preserved in SCD, EVA, and other third-window lesions, but may also be present in some cases of perilymphatic fistula. In otosclerosis, the reflex is usually absent due to the fixation of the stapes footplate, although it may remain detectable in early stages of the disease.[30][31]
High-resolution computed tomography (CT) of the temporal bone aids in evaluating CHL when the otoscopic examination appears normal. This imaging modality is more than 95% sensitive for detecting otosclerosis.[32] CT can also identify structural anomalies, such as EVA and SCD. The classic radiographic sign of otosclerosis is a radiolucency at the fissula ante fenestram, anterior to the stapes footplate, indicative of spongiotic bone. Sensorineural hearing loss caused by otosclerosis may be predicted by the presence of a “halo sign,” a hypodense ring around the cochlea or otic capsule, suggestive of retrofenestral involvement.[33] Notably, the sensorineural component of hearing loss in otosclerosis does not respond to surgery. Medical management with sodium fluoride or bisphosphonates may help stabilize progression, although long-term outcomes remain uncertain due to the absence of data from randomized, controlled trials.[34][35][36]
The ear selected for initial stapes surgery should be the one perceived by the patient as having poorer hearing, regardless of audiometric thresholds. Operating on the contralateral ear may be considered 6 months later, provided that it has since become the poorer-hearing ear. In pediatric cases, operating on the less functional ear may avoid the need for a hearing aid before school begins. Surgery on the better-hearing ear should be deferred until the child is mature enough to participate in the decision-making process.
Stapedotomy or stapedectomy may be performed under either local or general anesthesia. Local anesthesia allows intraoperative communication, enabling the surgeon to monitor for vertigo during prosthesis placement. General anesthesia eliminates distress from the loud noise generated during drilling on the stapes footplate. When general anesthesia is used, a facial nerve monitor is typically employed, and it requires avoiding long-acting neuromuscular blocking agents. Facial nerve monitoring not only preserves nerve function but also improves operative efficiency, facilitates anatomic identification, and enhances safety in training settings.[37] Anecdotal reports suggest that excessive infiltration of local anesthetic into the external auditory canal may impair facial nerve monitoring, particularly in the presence of dehiscence. However, this complication has not been systematically studied or confirmed.[38]
Proper patient positioning is essential to ensure a stable and ergonomic operative field. The head of the operating table should be rotated 180º away from the anesthesia provider, and the patient should be shifted laterally so that the operative ear is near the surgeon, aligning with the table’s midline. For patients with a short neck or large chest, a slight reverse Trendelenburg position can help displace the ipsilateral shoulder and improve access. If a venous graft from the dorsum of the hand is planned, the contralateral arm should be secured on an arm board. Shaving is generally unnecessary. Stray hair may be managed with adhesive tape, surgical lubricant, or skin glue. The surgical site is prepped with alcohol or povidone-iodine solution and draped for a transcanal approach. The operative microscope is draped before the case begins. The ear canal is suctioned of any residual solution, and cerumen is removed as necessary.
Technique or Treatment
The patient is positioned so that the surgeon, while seated, has a direct line of sight down the ear canal. Local anesthesia is administered using 1% lidocaine with 1:100,000 epinephrine through a 1.5-inch, 27- or 30-gauge needle, beginning at the posterior canal wall. Slow injection prevents tissue ballooning, which would otherwise obscure visualization of the middle ear. Infiltration proceeds circumferentially, with a total volume not exceeding 1 cc.
Among the various speculum sizes, the largest that can be comfortably seated should be used. A speculum holder may facilitate a 2-handed technique but may cause canal injury if the patient moves unexpectedly. Plain metal specula and instruments are preferred, as black-coated tools reduce illumination within the operative field.
The procedure begins as a middle ear exploration. Surgery on the stapes is pursued only after inspection of the ossicular chain confirms that a stapedotomy or stapedectomy is appropriate. The first step is elevation of a tympanomeatal flap. Using a sickle knife, a radial incision is made 1 to 2 mm from the tympanic membrane and extended superolaterally from the inferior annulus. A second incision is made superior and parallel to the pars flaccida. A circumferential incision connects the 2 to complete the flap (see Image. Tympanomeatal Flap Incisions for Stapedotomy).
Several sweeps with the sickle knife may be required to incise the periosteum, which is tightly adherent to the fragile skin of the canal. A House round knife or #7200 beaver blade is used to create the connecting incision, which lies 7 to 8 mm lateral and parallel to the tympanic annulus. Including the vascular strip of the canal wall in the flap improves perfusion and promotes postoperative healing. Once incised, the flap is elevated with a round knife toward the tympanic membrane until the fibrous annulus is visualized. The mucosa is then incised under the annulus using a sickle knife and opened to expose the middle ear. The annulus is elevated from the tympanic sulcus with a Gimmick elevator as the flap is reflected superiorly.
Surface tension typically maintains adherence of the tympanomeatal flap to the anterior aspect of the canal and tympanic membrane, enabling visualization of the posterior middle ear. The scutum, a bony overhang in the posterosuperior quadrant, is curetted away to uncover the chorda tympani nerve and expose the stapes. Surgery proceeds once the following landmarks are visible: the neck and handle of the malleus anteriorly, the round window niche inferiorly, the pyramidal process posteriorly, and the horizontal segment of the facial nerve superiorly (see Image. Left Middle Ear Exposure).
Once adequate exposure is achieved, the ossicular chain must be palpated to identify the site of pathology. In a normal middle ear, palpation of the malleus produces a round-window reflex, indicating an intact ossicular chain and physiologic movement of perilymph within the scala media and scala vestibuli. If present, this finding warrants aborting the procedure and pursuing alternative causes of CHL, such as SCD. The round-window reflex is absent in otosclerosis due to stapes fixation. A similar absence may occur with malleus fixation, necessitating repalpation of the malleus to assess mobility after separation of the incudostapedial joint.
The subsequent steps may be performed in a variable sequence depending on the surgeon's preference. The division of the incudostapedial joint is performed using an incudostapedial joint knife, which is moved gently in a sawing motion from posterior to anterior, allowing the stapedial tendon to stabilize the stapes. The tendon is then severed with Bellucci scissors.
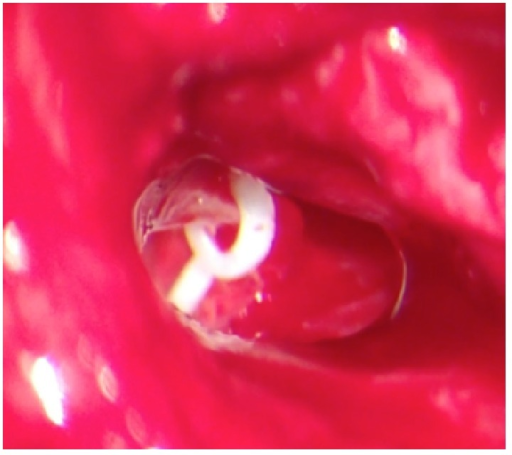
The downfracture of the stapes superstructure may follow, with or without prior laser or drill sectioning of the crura (see Image. Severing the Stapedius Tendon). A right-angle pick is used to sharply sweep the capitulum inferiorly to fracture both crura simultaneously, or just the anterior crus if the posterior has already been sectioned. Removing the superstructure before footplate fenestration improves visualization. However, creating the fenestra first provides a means of securing a mobile footplate should it loosen during the downfracture. Some surgeons delay the downfracture until after the prosthesis is inserted into the fenestra.
Prosthesis length is determined by measuring the distance from the footplate to the top of the incus and adding 0.25 mm to allow for vestibular penetration. Most prostheses measure approximately 4.25 mm, though the range extends from 3.5 to 5.5 mm. Several prosthesis types are available, and incus attachment techniques vary: the prosthesis may slide onto the long process, clip or crimp into place, or attach via laser-induced loop shrinkage (see Image. Fluoroplastic Piston Placement).[39][40]
Footplate fenestration, also known as platinotomy, is often initiated by creating a rosette with the laser and completing the perforation with a microdrill (see Image. Stapes Footplate Perforation by Fiber-Delivered Carbon Dioxide Laser). The resulting fenestra should be slightly larger than the prosthesis, typically between 0.3 and 0.8 mm in diameter. Wider implants may better close the ABG, while narrower devices may reduce the risk of inner ear complications. A blood patch is applied to the footplate to minimize perilymph leakage following prosthesis placement. This step is achieved by scratching the mucosa of the cochlear promontory, allowing a small amount of blood to pool at the oval window.
Stapedectomy is an older procedure that is now performed less frequently than stapedotomy, given that stapedotomy offers greater improvement in high-frequency hearing and may carry a lower complication rate.[41] Nonetheless, maintaining the ability to perform a stapedectomy remains essential, as intraoperative complications, such as fragmentation of the footplate during the downfracture of the stapes superstructure, may necessitate conversion from stapedotomy to stapedectomy.
The distinction between these 2 procedures lies in the extent of footplate removal. Stapedotomy entails excision of a central core of the footplate to accommodate the prosthesis piston. In contrast, stapedectomy involves the removal of nearly the entire footplate, leaving only the central portion, approximately 25%, to support the prosthesis. Any bone fragments that fall into the vestibule during footplate removal should be left undisturbed unless clearly visible and easily retrievable.
Before prosthesis placement during stapedectomy, a graft, commonly harvested from tragal perichondrium, temporalis fascia, or vein wall, is typically positioned to seal the oval window. Graft harvest should occur before manipulation of the stapes begins, so that the material is immediately available following footplate removal, thereby minimizing the duration of vestibular exposure. After placement of the prosthesis, the ossicular chain is palpated to confirm restored mobility. Small pieces of gelatin foam may be positioned around the piston to support it during the early healing phase. Gelatin foam must be used judiciously, as its overuse has been implicated in the development of reparative granuloma, a potentially devastating complication. Once prosthesis support has been secured, the tympanomeatal flap is repositioned, and the external auditory canal is lightly packed with cotton impregnated with antibiotic ointment.
In addition to stapedectomy and stapedotomy, a third surgical option exists for otosclerosis confined to the anterior stapes footplate: stapedotomy minus prosthesis, or the “StaMP” procedure.[42] Otosclerosis typically originates at the fissula ante fenestram, initially affecting the anterior footplate. The StaMP procedure involves removal of the anterior crus and laser separation of the fixed anterior third of the footplate from the mobile posterior two-thirds. This approach preserves the native ossicular chain and avoids both prosthesis placement and manipulation of the oval window. Outcomes following the StaMP procedure are comparable to those of traditional stapes surgeries while preserving stapedius tendon function and minimizing the risk of hyperacusis. Conversion to a stapedotomy or stapedectomy is possible if otosclerosis progresses to involve the posterior footplate.
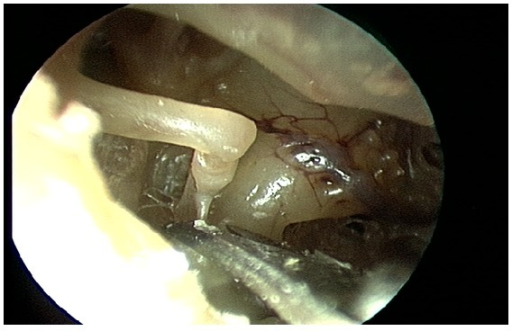
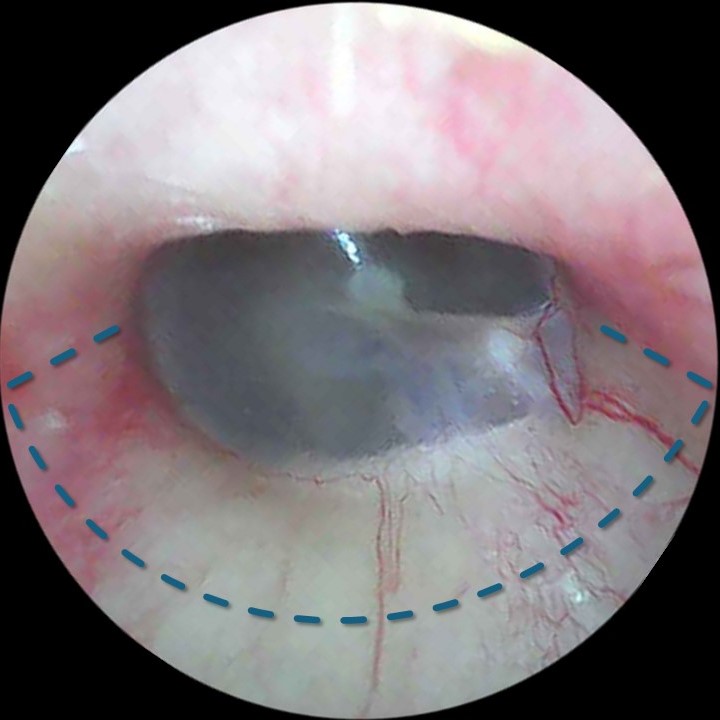
Partial or complete dehiscence of the tympanic segment of the facial nerve commonly presents during middle ear surgery (see Image. Incudostapedial Joint, Intraoperative View). Recognizing this anomaly is essential to prevent iatrogenic injury. In some cases, the facial nerve overhangs the oval window or courses directly across its surface. Gentle retraction using the side of a suction tip often permits sufficient exposure to complete a fenestration and prosthesis placement. When the overhang is more pronounced, certain metal crimp-on prostheses can accommodate the nerve by curving around it. Complete obstruction of the footplate by a significantly displaced facial nerve may require aborting the surgery.
A persistent stapedial artery, a remnant of the second branchial arch vasculature, may also hinder or preclude completion of the procedure. This artery traverses the obturator foramen of the stapes, between the crura, and can obstruct access to the footplate (see Image. Stages of Stapedial Artery Development). In most cases, the vessel’s caliber allows for the placement of the prosthesis adjacent to it. However, complete obstruction of the foramen may necessitate the cessation of the operation, with hearing amplification subsequently achieved through the use of a hearing aid. Although cautery and transection of the persistent stapedial artery are generally well tolerated and may eliminate a source of pulsatile tinnitus, the artery’s course through the facial nerve canal and its contribution to the middle meningeal artery raise the risk of facial paralysis or cerebral ischemia following ligation. Ideally, angiography should precede division of the artery.[43][44]
Complications
Middle ear procedures, such as stapedotomy and stapedectomy, should always prioritize hearing preservation, even when complications necessitate intraoperative cessation. Retaining cochlear reserve remains preferable to risking profound sensorineural hearing loss, and hearing aids offer a viable alternative when surgery cannot proceed safely. Intraoperative complications may include tympanic membrane perforation, chorda tympani nerve injury, ossicular chain disruption, floating stapedial footplate, perilymph leakage, facial nerve injury, and vertigo. Postoperative complications include reparative granuloma, perilymphatic fistula, and hyperacusis. The latter commonly arises from division of the stapedius tendon, although perilymph leakage and granuloma formation can also contribute to profound or complete sensorineural hearing loss.
Tympanic membrane perforation often results from raising the tympanomeatal flap before annular elevation. Small tears may be managed with resorbable gelatin sponge. Larger defects may require reinforcement with harvested tissue, such as temporalis fascia or perichondrium. Preoperative assessment of tympanic membrane integrity remains critical, as atrophic membranes may necessitate concurrent myringoplasty. Despite these risks, tympanic membrane complications rarely affect the overall success of stapes surgery.
When curetting the scutum to improve visualization of the stapes, care must be taken to avoid injury to the chorda tympani nerve, which can be preserved in approximately 90% of cases. Partial transection may be managed by reapproximating the nerve fibers, whereas complete sectioning is occasionally unavoidable. Interestingly, patients who undergo complete transection tend to report fewer symptoms of dysgeusia than those with injured but anatomically intact nerves.[45] Ossicular disruption outside the incudostapedial joint is uncommon and typically involves subluxation of the incudomalleal joint due to lateral displacement of the long process of the incus during separation of the incudostapedial joint. Although this displacement may complicate prosthesis insertion, repositioning the incus generally restores proper alignment and results in favorable hearing outcomes.
Downfracture of the stapes superstructure carries a small risk (<1%) of complete footplate avulsion from its annular attachment to the oval window. This complication can also arise during fenestration of a thickened footplate, making it essential to avoid excessive pressure. A "floating" footplate must be secured, often requiring careful drilling or curetting on the promontory side until a small right-angled pick can be positioned beneath the plate. Consequently, some surgeons prefer to fenestrate the footplate before downfracturing the superstructure, thereby ensuring a secure point of traction if removal becomes necessary.
When multiple fragments remain mobile within the oval window, a few drops of blood can be applied to the site. Once clotted, the fragments may be withdrawn en bloc within the clot. Fragments that fall into the vestibule should not be retrieved blindly, as instrumentation within the vestibule carries a risk of sensorineural hearing loss and vertigo. Small bony fragments left in the vestibule rarely lead to complications, although larger fragments may provoke symptoms resembling benign paroxysmal positional vertigo.
Postoperative or intraoperative vertigo may arise from excessive manipulation of the stapes or a reduction in vestibular fluid volume, both of which stimulate labyrinthine receptors. Under local anesthesia, vertigo can serve as an early warning sign of impending inner ear trauma—an advantage not available under general anesthesia. Vertigo during prosthesis placement often indicates that the piston is too long and irritating the saccule, prompting consideration of a shorter implant (see Image. Three-Dimensional Reconstruction of Stapes and Vestibular Structures from Micro–Computed Tomography).
Persistent vertigo may prevent completion of the procedure in awake patients, which is a reason many surgeons prefer general anesthesia. Rapid management of vertigo is essential. Droperidol, administered slowly via intravenous push, offers the fastest relief. Close monitoring is necessary following administration due to the risk of hypotension.
On rare occasions, a sudden flow of perilymph, referred to as a "perilymph gusher," may occur immediately after fenestration of the stapes footplate. This phenomenon most commonly affects children with congenital stapes fixation but has occasionally been observed in adults with otosclerotic disease. The appearance of a perilymphatic gusher significantly increases the risk of sensorineural hearing loss following surgery. Gushers typically result from enlargement of the cochlear aqueduct or an abnormal connection between the subarachnoid and perilymphatic spaces, such as a fistula between the medial internal auditory canal and the labyrinth.[46]
Preoperative CT of the temporal bones is recommended when planning stapedectomy in young patients, given the increased likelihood of congenital otic capsule anomalies in children with hearing loss. Upon encountering a gusher, the surgeon should elevate the patient's head, harvest fat from the earlobe for placement into the oval window, and use the prosthesis to secure the fat. Postoperative head elevation must be maintained. Insertion of a lumbar drain may serve as an additional measure to control cerebrospinal fluid pressure.
Iatrogenic perilymphatic fistulas may also develop after stapes surgery if the temporary opening created during platinotomy fails to seal. Imperfect graft placement, prosthesis displacement, or abrupt increases in intracranial pressure, such as those caused by coughing or sneezing, can lead to persistent or recurrent leakage. Affected patients typically report fluctuating hearing loss and dizziness, and audiometry will reveal sensorineural hearing loss. Prompt surgical exploration is essential to preserve hearing. If a fistula is identified, revision of the graft and prosthesis must be performed immediately.
The most feared complication of stapes surgery is the formation of reactive granulation tissue in and around the oval window. The etiology of these reparative granulomas remains uncertain, although their incidence appears to have declined with the use of modern prostheses. To minimize risk, some authors recommend using powder-free gloves, avoiding gelatin foam, and rinsing the prosthesis before insertion into the middle ear.
Reparative granulomas typically present within 1 to 2 weeks postoperatively, with patients reporting otalgia, vertigo, and worsening hearing. Otoscopic examination may reveal a violaceous mass in the posterosuperior quadrant of the tympanic membrane, and audiometry usually demonstrates sensorineural hearing loss with deterioration of speech recognition thresholds. Management requires urgent surgical removal of the granulomatous tissue, replacement of the prosthesis and graft, and adjunctive administration of high-dose corticosteroids. Delayed intervention may result in irreversible sensorineural deficits, including complete anacusis.[47]
Clinical Significance
Over the 40 years that Dr Shea performed stapedectomy, he consistently produced good results, and the outcomes of stapes operations have continued to improve over the ensuing years as the quality of surgical microscopes, prostheses, drills, and laser delivery systems has evolved.[48] Successful closure of the ABG after stapes surgery occurs in 90% and 70% of primary and revision cases, respectively. Nevertheless, the potential for causing iatrogenic sensorineural hearing loss remains. Shea found that 1.8% of primary and 4% of revision stapedectomies resulted in this complication. Stapedectomy at baseline is a technically challenging operation due to the small size of the structures involved, the precise tolerances for prosthesis placement, and the tight confines in which the procedure takes place. All these challenges are exacerbated in cases requiring revision, and the risk of profound sensorineural hearing loss, or even an anacustic, "dead ear," is substantially higher.
Stapedectomy and stapedotomy are both considered state-of-the-art operations in treating CHL due to otosclerosis, with the small fenestra stapedotomy procedure being most commonly performed at present. The reason is that many perceive stapedotomy as affording greater improvements in hearing at higher frequencies and carrying lower complication rates than stapedectomy, although controversy persists on this point. However, as many studies have concluded, the surgeon's experience plays a greater role in the success and safety of the stapes procedure than the particular operative technique selected.[49][50] Despite the risks involved and the expertise required for stapes surgery, no treatment currently surpasses this intervention in improving bone conduction and closing the ABG associated with CHL, especially in the setting of otosclerosis.[51][52]
Enhancing Healthcare Team Outcomes
Only surgeons who are sufficiently trained, familiar with the relevant anatomy, and experienced in middle ear surgery for otosclerosis should perform stapes surgery, and only when supported by a trained surgical technician, a knowledgeable circulating nurse, an experienced anesthesia provider, and appropriate equipment. The specific procedure selected to treat CHL, whether stapedectomy or stapedotomy, using lasers or drills, plays a lesser role in outcomes than the proficiency of the surgeon. A 90% closure of the ABG and an sensorineural hearing loss rate below 1% validate the choice of technique and equipment.
Media
(Click Image to Enlarge)
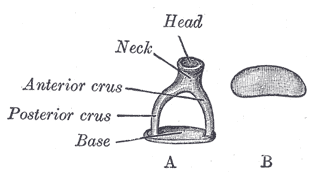
Stapes. Frontal view of the A) left stapes, B) medial surface of the base.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
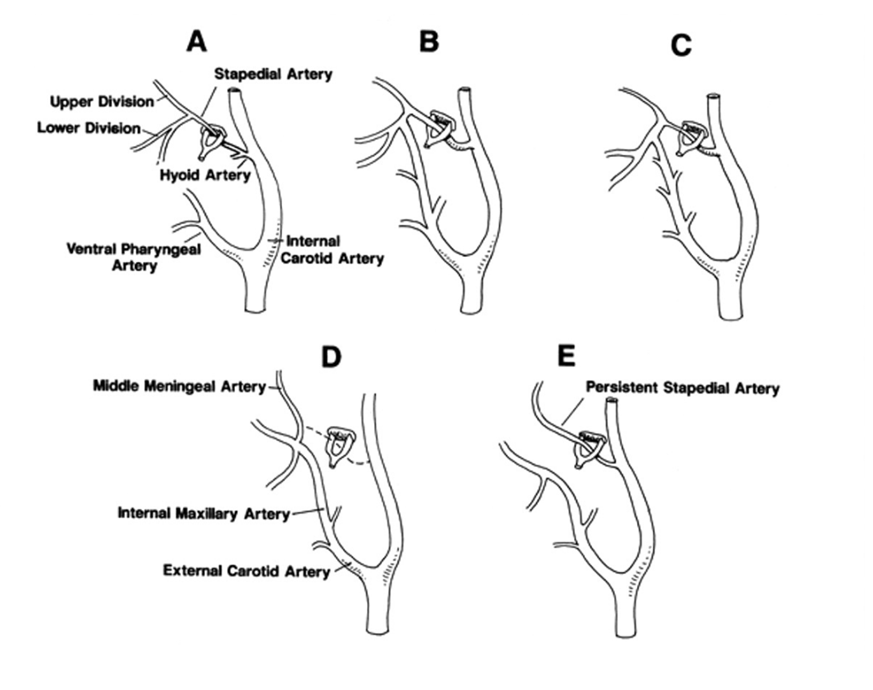
Stages of Stapedial Artery Development. This schematic illustrating embryologic progression was adapted from Silbergleit et al. A) The stapedial artery arises from the hyoid branch of the internal carotid artery and passes through the stapes, branching into upper and lower divisions. B) The lower division anastomoses with the ventral pharyngeal artery, a precursor of the external carotid artery. C) The stapedial artery begins to regress. D) Normal adult anatomy, following complete involution of the stapedial artery. E) Anatomic configuration seen in a persistent stapedial artery, reflecting failure of regression.
With use of the freely accessible article by: Richard Silbergleit, Douglas J. Quint, Bharat A. Mehta, Suresh C. Patel, Joseph J. Metes, and Samir E. Noujaim: The Persistent Stapedial Artery. AJNR 200: 21:572–577
(Click Image to Enlarge)
(Click Image to Enlarge)
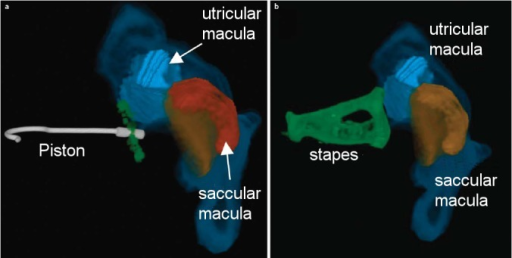
Three-Dimensional Reconstruction of Stapes and Vestibular Structures from Micro–Computed Tomography. Three-dimensional reconstruction of human temporal bone micro–computed tomography images (courtesy of Ian Curthoys and Payal Mukherjee, University of Sydney) demonstrating the spatial relationship between the stapes footplate, prosthesis, and vestibular organs. A) View of a 0.25-mm deep stapes piston (gray) relative to the stapes footplate (green), utricular macula (light blue), and saccular macula (orange); utriculus and sacculus are shown in dark blue and red, respectively. B) Three-dimensional reconstruction of the stapes (green) with utricular and saccular maculae. Both panels illustrate that the posterosuperior utricular macula lies closest to the footplate.
With permission, from: Schick B, Dlugaiczyk J. Surgery of the ear and the lateral skull base: pitfalls and complications. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2013 Dec 13;12:Doc05.
(Click Image to Enlarge)
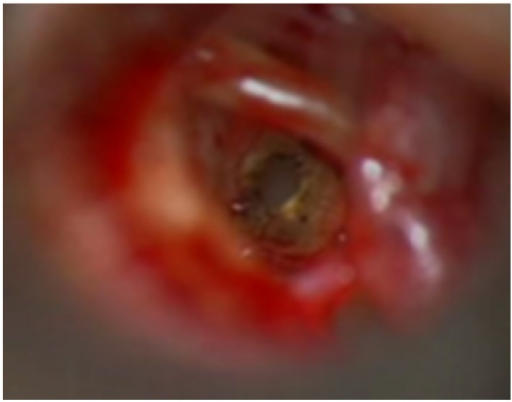
Stapes Footplate Perforation by Fiber-Delivered Carbon Dioxide Laser. Intraoperative image showing a complication resulting from direct perforation of the stapes footplate by a fiber-delivered carbon dioxide laser.
With permission, from: Yetiser S. Flexible Fiber Optic Carbon-Dioxide Laser Assisted Stapedotomy in Otosclerosis. Int J Otolaryngol. 2016;2016:4958074.
(Click Image to Enlarge)
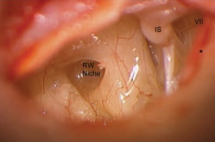
Left Middle Ear Exposure. Intraoperative view demonstrating the incudostapedial joint, chorda tympani nerve (marked by ∗), and tympanic segment of the facial nerve (cranial nerve VII) within the left middle ear.
With permission, from: Silverstein H, Ojo R, Daugherty J, Nazarian R, Wazen J. Minimally invasive surgery for the treatment of hyperacusis. Otol Neurotol. 2016 Dec;37(10):1482-1488.
(Click Image to Enlarge)
Severing the Stapedius Tendon. A straight, sharp instrument such as Bellucci microscissors is preferred for dividing the stapedius tendon during stapes surgery.
With permission, from: Pollak N, Azadarmaki R, Ahmad S. Feasibility of endoscopic treatment of middle ear myoclonus: a cadaveric study. ISRN Otolaryngol. 2014 Mar 10;2014:175268.
(Click Image to Enlarge)
Fluoroplastic Piston Placement. Intraoperative image showing placement of a fluoroplastic piston prosthesis onto the long process of the incus and into the stapedotomy fenestration.
With permission, from: Henriques V, Teles R, Sousa A, Estevão R, Rodrigues J, Gomes A, Silva F, Fernandes Â, Fernandes F. Abnormal congenital location of stapes' superstructure: clinical and embryological implications. Case Rep Otolaryngol. 2016;2016:2598962.
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
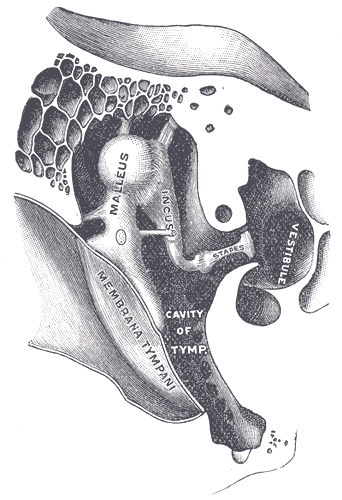
Right Auditory Ossicles. This image shows the anterior aspect of the right chain of ossicles (malleus, incus, and stapes) and their ligaments. Other structures in this illustration include the tympanic membrane, tympanic cavity, and vestibule.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
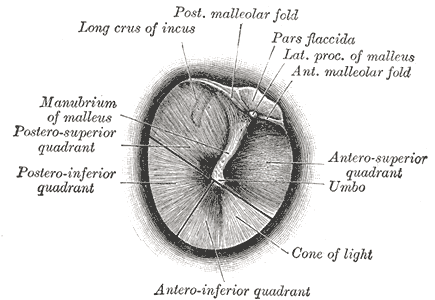
Right Tympanic Membrane, Otoscopic View. Illustration depicting the normal right tympanic membrane as seen through a speculum. Key landmarks include the long crus of the incus, posterior and anterior malleolar folds, pars flaccida, lateral process and manubrium of the malleus, umbo, cone of light, and the four quadrants of the membrane.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
Tympanomeatal Flap Incisions for Stapedotomy. Intraoperative photo showing standard incisions for elevating a tympanomeatal flap. Two radial incisions extend parallel to each other from approximately 1 to 2 mm lateral to the tympanic membrane to a point 7 to 8 mm away, where they are connected by a transverse incision.
Contributed by Marc H Hohman, MD, FACS
(Click Image to Enlarge)

Audiometric and Tympanometric Findings in Otosclerosis. 1) Pure-tone audiogram demonstrates bilateral mild conductive hearing loss with a characteristic Carhart notch at 2 kHz. 2) Tympanogram reveals reduced compliance in both ears. These findings are consistent with increased stiffness of the middle ear system, suggestive of otosclerosis.
Contributed by Yasmin Naqvi
References
Bajaj Y, Uppal S, Bhatti I, Coatesworth AP. Otosclerosis 3: the surgical management of otosclerosis. International journal of clinical practice. 2010 Mar:64(4):505-10. doi: 10.1111/j.1742-1241.2009.02047.x. Epub [PubMed PMID: 20456195]
Souza JC, Bento RF, Pereira LV, Ikari L, Souza SR, Della Torre AA, Fonseca AC. Evaluation of Functional Outcomes after Stapes Surgery in Patients with Clinical Otosclerosis in a Teaching Institution. International archives of otorhinolaryngology. 2016 Jan:20(1):39-42. doi: 10.1055/s-0035-1563540. Epub 2015 Nov 4 [PubMed PMID: 26722344]
Nazarian R, McElveen JT Jr, Eshraghi AA. History of Otosclerosis and Stapes Surgery. Otolaryngologic clinics of North America. 2018 Apr:51(2):275-290. doi: 10.1016/j.otc.2017.11.003. Epub [PubMed PMID: 29502722]
Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy Versus Stapedotomy. Otolaryngologic clinics of North America. 2018 Apr:51(2):375-392. doi: 10.1016/j.otc.2017.11.008. Epub 2018 Feb 3 [PubMed PMID: 29397948]
Markou K, Goudakos J. An overview of the etiology of otosclerosis. European archives of oto-rhino-laryngology : official journal of the European Federation of Oto-Rhino-Laryngological Societies (EUFOS) : affiliated with the German Society for Oto-Rhino-Laryngology - Head and Neck Surgery. 2009 Jan:266(1):25-35. doi: 10.1007/s00405-008-0790-x. Epub 2008 Aug 13 [PubMed PMID: 18704474]
Level 3 (low-level) evidenceBatson L, Rizzolo D. Otosclerosis: An update on diagnosis and treatment. JAAPA : official journal of the American Academy of Physician Assistants. 2017 Feb:30(2):17-22. doi: 10.1097/01.JAA.0000511784.21936.1b. Epub [PubMed PMID: 28060022]
Peng KA, House JW. Schwartze sign. Ear, nose, & throat journal. 2018 Mar:97(3):54 [PubMed PMID: 29554394]
Saha KL, Tarafder F. Peroperative Notification of Schwartze Sign in Otosclerosis. OTO open. 2024 Oct-Dec:8(4):e70021. doi: 10.1002/oto2.70021. Epub 2024 Oct 6 [PubMed PMID: 39371246]
Ealy M, Smith RJH. Otosclerosis. Advances in oto-rhino-laryngology. 2011:70():122-129. doi: 10.1159/000322488. Epub 2011 Feb 24 [PubMed PMID: 21358194]
Level 3 (low-level) evidenceTato JM, Tato JM Jr. Otosclerosis and races. The Annals of otology, rhinology, and laryngology. 1967 Dec:76(5):1018-25 [PubMed PMID: 6074235]
Fabbris C, Molteni G, Tommasi N, Marchioni D. Does pregnancy have an influence on otosclerosis? The Journal of laryngology and otology. 2022 Mar:136(3):191-196. doi: 10.1017/S0022215121003601. Epub 2021 Nov 25 [PubMed PMID: 34819176]
Shea JJ Jr. Forty years of stapes surgery. The American journal of otology. 1998 Jan:19(1):52-5 [PubMed PMID: 9455948]
Level 2 (mid-level) evidencePersson P, Harder H, Magnuson B. Hearing results in otosclerosis surgery after partial stapedectomy, total stapedectomy and stapedotomy. Acta oto-laryngologica. 1997 Jan:117(1):94-9 [PubMed PMID: 9039488]
Level 2 (mid-level) evidenceHouse HP, Hansen MR, Al Dakhail AA, House JW. Stapedectomy versus stapedotomy: comparison of results with long-term follow-up. The Laryngoscope. 2002 Nov:112(11):2046-50 [PubMed PMID: 12439178]
Level 2 (mid-level) evidenceVincent R, Sperling NM, Oates J, Jindal M. Surgical findings and long-term hearing results in 3,050 stapedotomies for primary otosclerosis: a prospective study with the otology-neurotology database. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2006 Dec:27(8 Suppl 2):S25-47 [PubMed PMID: 16985478]
Battista RA, Wiet RJ, Joy J. Revision stapedectomy. Otolaryngologic clinics of North America. 2006 Aug:39(4):677-97, v-vi [PubMed PMID: 16895778]
McGee TM. Comparison of small fenestra and total stapedectomy. The Annals of otology, rhinology, and laryngology. 1981 Nov-Dec:90(6 Pt 1):633-6 [PubMed PMID: 7316389]
Fisch U. Stapedotomy versus stapedectomy. The American journal of otology. 1982 Oct:4(2):112-7 [PubMed PMID: 7148999]
Cremers CW, Beusen JM, Huygen PL. Hearing gain after stapedotomy, partial platinectomy, or total stapedectomy for otosclerosis. The Annals of otology, rhinology, and laryngology. 1991 Dec:100(12):959-61 [PubMed PMID: 1746841]
Rizer FM, Lippy WH. Evolution of techniques of stapedectomy from the total stapedectomy to the small fenestra stapedectomy. Otolaryngologic clinics of North America. 1993 Jun:26(3):443-51 [PubMed PMID: 8341573]
Level 2 (mid-level) evidenceSheehy JL, Gardner G Jr, Hambley WM. Tuning fork tests in modern otology. Archives of otolaryngology (Chicago, Ill. : 1960). 1971 Aug:94(2):132-8 [PubMed PMID: 5556271]
Doyle PJ, Anderson DW, Pijl S. The tuning fork--an essential instrument in otologic practice. The Journal of otolaryngology. 1984 Apr:13(2):83-6 [PubMed PMID: 6726852]
Issa TK, Bahgat MA, Linthicum FH Jr, House HP. The effect of stapedectomy on hearing of patients with otosclerosis and Meniere's disease. The American journal of otology. 1983 Apr:4(4):323-6 [PubMed PMID: 6859241]
Hodgson RS, Wilson DF. Argon laser stapedotomy. The Laryngoscope. 1991 Mar:101(3):230-3 [PubMed PMID: 2000008]
Bartels LJ. KTP laser stapedotomy: is it safe? Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 1990 Nov:103(5 ( Pt 1)):685-92 [PubMed PMID: 2126087]
Level 3 (low-level) evidenceLesinski SG, Palmer A. Lasers for otosclerosis: CO2 vs. Argon and KTP-532. The Laryngoscope. 1989 Jun:99(6 Pt 2 Suppl 46):1-8 [PubMed PMID: 2498587]
Maalouf RR, Marc M, Mukherjee P, Van Rompaey V, Eliezer M, Hautefort C, Verillaud B, Herman P, Kania R. Otosclerosis: audiometric results and quality of life after stapedectomy with interposition or CO(2) laser-calibrated stapedotomy without interposition. Acta oto-laryngologica. 2023 Mar:143(3):231-236. doi: 10.1080/00016489.2023.2186482. Epub 2023 Mar 20 [PubMed PMID: 36939022]
Level 2 (mid-level) evidencePerkins RC. Laser stepedotomy for otosclerosis. The Laryngoscope. 1980 Feb:90(2):228-40 [PubMed PMID: 7354691]
Merchant SN, Rosowski JJ, McKenna MJ. Superior semicircular canal dehiscence mimicking otosclerotic hearing loss. Advances in oto-rhino-laryngology. 2007:65():137-145. doi: 10.1159/000098790. Epub [PubMed PMID: 17245035]
Level 3 (low-level) evidenceJerger J, Anthony L, Jerger S, Mauldin L. Studies in impedance audiometry. 3. Middle ear disorders. Archives of otolaryngology (Chicago, Ill. : 1960). 1974 Mar:99(3):165-71 [PubMed PMID: 4854446]
Hannley MT. Audiologic characteristics of the patient with otosclerosis. Otolaryngologic clinics of North America. 1993 Jun:26(3):373-87 [PubMed PMID: 8341569]
Kanona H, Rana I, Offiah C, Patel N. Importance of a dedicated neuroradiologist in reporting high-resolution computed tomography for otosclerosis: a retrospective comparison study of 40 patients. The Journal of laryngology and otology. 2017 Jun:131(6):492-496. doi: 10.1017/S0022215117000561. Epub 2017 Mar 20 [PubMed PMID: 28318477]
Level 2 (mid-level) evidenceVirk JS, Singh A, Lingam RK. The role of imaging in the diagnosis and management of otosclerosis. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2013 Sep:34(7):e55-60. doi: 10.1097/MAO.0b013e318298ac96. Epub [PubMed PMID: 23921926]
Level 1 (high-level) evidencede Oliveira Penido N, de Oliveira Vicente A. Medical Management of Otosclerosis. Otolaryngologic clinics of North America. 2018 Apr:51(2):441-452. doi: 10.1016/j.otc.2017.11.006. Epub [PubMed PMID: 29502728]
Patel S, Walters B, Eastwood M, Abou-Foul AK, Bhimrao S. A Systematic Review of the Effectiveness of Bisphosphonates for Otosclerosis. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2022 Jun 1:43(5):530-537. doi: 10.1097/MAO.0000000000003510. Epub 2022 Feb 24 [PubMed PMID: 35213475]
Level 1 (high-level) evidenceGogoulos PP, Sideris G, Nikolopoulos T, Sevastatou EK, Korres G, Delides A. Conservative Otosclerosis Treatment With Sodium Fluoride and Other Modern Formulations: A Systematic Review. Cureus. 2023 Feb:15(2):e34850. doi: 10.7759/cureus.34850. Epub 2023 Feb 10 [PubMed PMID: 36923175]
Level 1 (high-level) evidenceCasano K, Giangrosso G, Mankekar G, Sevy A, Mehta R, Arriaga M. Additional Benefits of Facial Nerve Monitoring during Otologic Surgery. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2020 Sep:163(3):572-576. doi: 10.1177/0194599820915458. Epub 2020 Apr 14 [PubMed PMID: 32283984]
Caner G, Olgun L, Gültekin G, Aydar L. Local anesthesia for middle ear surgery. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2005 Aug:133(2):295-7 [PubMed PMID: 16087030]
Level 2 (mid-level) evidenceFritsch MH, Naumann IC. Phylogeny of the stapes prosthesis. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2008 Apr:29(3):407-15. doi: 10.1097/MAO.0b013e3181690775. Epub [PubMed PMID: 18317391]
Košec A, Živko J, Marković S, Kelava I, Ajduk J, Ries M. COMPARISON OF HEARING OUTCOMES AFTER STAPES SURGERY DEPENDING ON PROSTHESIS TYPE: A RETROSPECTIVE ANALYSIS. Acta clinica Croatica. 2022 Oct:61(Suppl 4):41-46. doi: 10.20471/acc.2022.61.s4.5. Epub [PubMed PMID: 37250664]
Level 2 (mid-level) evidenceMolinier CE, Gallois Y, Deguine O, Iversenc G, Vales O, Taoui S, Lepage B, Fraysse B, Marx M. Stapedotomy Versus Hearing Aids in the Management of Conductive Hearing Loss Caused by Otosclerosis: A Prospective Comparative Study. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2022 Aug 1:43(7):773-780. doi: 10.1097/MAO.0000000000003585. Epub [PubMed PMID: 35878633]
Level 2 (mid-level) evidenceSilverstein H. Laser stapedotomy minus prosthesis (laser STAMP): a minimally invasive procedure. The American journal of otology. 1998 May:19(3):277-82 [PubMed PMID: 9596174]
Glasscock ME 3rd, Dickins JR, Jackson CG, Wiet RJ. Vascular anomalies of the middle ear. The Laryngoscope. 1980 Jan:90(1):77-88 [PubMed PMID: 7356771]
Silbergleit R, Quint DJ, Mehta BA, Patel SC, Metes JJ, Noujaim SE. The persistent stapedial artery. AJNR. American journal of neuroradiology. 2000 Mar:21(3):572-7 [PubMed PMID: 10730654]
Michael P, Raut V. Chorda tympani injury: operative findings and postoperative symptoms. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2007 Jun:136(6):978-81 [PubMed PMID: 17547991]
Cassano P, Decandia N, Cassano M, Fiorella ML, Ettorre G. Perilymphatic gusher in stapedectomy: demonstration of a fistula of internal auditory canal. Acta otorhinolaryngologica Italica : organo ufficiale della Societa italiana di otorinolaringologia e chirurgia cervico-facciale. 2003 Apr:23(2):116-9 [PubMed PMID: 14526560]
Seicshnaydre MA, Sismanis A, Hughes GB. Update of reparative granuloma: survey of the American Otological Society and the American Neurotology Society. The American journal of otology. 1994 Mar:15(2):155-60 [PubMed PMID: 8172294]
Level 3 (low-level) evidenceSevy A, Arriaga M. The Stapes Prosthesis: Past, Present, and Future. Otolaryngologic clinics of North America. 2018 Apr:51(2):393-404. doi: 10.1016/j.otc.2017.11.010. Epub [PubMed PMID: 29502725]
Colletti V, Sittoni V, Fiorino FG. Stapedotomy with and without stapedius tendon preservation versus stapedectomy: long-term results. The American journal of otology. 1988 Mar:9(2):136-41 [PubMed PMID: 3407746]
Sedwick JD, Louden CL, Shelton C. Stapedectomy vs stapedotomy. Do you really need a laser? Archives of otolaryngology--head & neck surgery. 1997 Feb:123(2):177-80 [PubMed PMID: 9046285]
Level 2 (mid-level) evidenceVijayendra H, Parikh B. Bone conduction improvement after surgery for conductive hearing loss. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India. 2011 Jul:63(3):201-4. doi: 10.1007/s12070-011-0130-0. Epub 2011 Feb 23 [PubMed PMID: 22754794]
Bonnafous S, Margier J, Bartier S, Tournegros R, Tringali S, Fieux M. Estimated Costs Associated With Management of Otosclerosis With Hearing Aids vs Surgery in Europe. JAMA network open. 2022 Feb 1:5(2):e2148932. doi: 10.1001/jamanetworkopen.2021.48932. Epub 2022 Feb 1 [PubMed PMID: 35175343]