Introduction
A skin biopsy is an important diagnostic procedure commonly performed in dermatology practices.[1] Various methods of skin biopsies exist, and multiple factors are considered in choosing the most appropriate biopsy technique for a given situation.[2] Among the most important factors are location, depth, and breadth of sampling. An effort is made to provide the consulting pathologist with an adequate amount of tissue from the site most likely to yield a diagnosis while minimizing disfigurement and preserving the patient’s function as much as possible.
Biopsies are categorized as either incisional, where only a portion of a lesion is sampled, or excisional, where the entire visible lesion is removed. An incisional biopsy can be performed using shave, scissor, curettage, or punch techniques. An excisional biopsy is typically performed with a full-thickness scalpel excision or a deeper oblique (shave or scoop) excision.
Anatomy and Physiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Anatomy and Physiology
When performing a skin biopsy, the clinician must consider the underlying anatomical structures of the skin region, eg, blood vessels, nerves, and muscles, especially when taking a specimen from the face, neck, hands, or feet. Careful planning is necessary to minimize the risk of functional impairment, excessive bleeding, or scarring, while ensuring an adequate diagnostic sample is obtained.
Indications
A skin biopsy is indicated for diagnosing conditions of the skin as well as systemic diseases that have skin or soft tissue manifestations.
Contraindications
A skin biopsy has various relative contraindications for which clinicians should take appropriate precautions, including:
- Allergy to local anesthetics
- Active infection
- Tattoo at the planned biopsy site
Additionally, the prebiopsy evaluation should thoroughly review the patient's clinical history, including any bleeding disorders and the use of anticoagulant medications. However, these factors are not absolute contraindications for skin biopsy.[3]
Equipment
Required equipment includes:
- Skin disinfectant: Usually alcohol, but other skin disinfectants may be used
- Local anesthetic
- Most commonly lidocaine (0.5% to 2%) with or without epinephrine
- Buffering 1:9 with sodium bicarbonate significantly decreases the pain of injection [4]
- Gauze
- Biopsy instrument (usually 1 of the following)
- Biopsy punch
- #15 scalpel blade
- Flexible hand-held surgical blade or razor blade
- Small scissors (for skin tags or other small, protuberant lesions, especially on thin skin)
- Specimen fixative: Most biopsy specimens should be placed in formalin; however, specific tests, eg, direct immunofluorescence and tissue cultures, require alternative media (eg, Michel's solution or sterile saline).[2]
- Hemostatic agent
- Aluminum chloride solution is most commonly used; however, other agents (eg, Monsel's ferric subsulfate solution or Gelfoam) may also be employed.
- Electrocoagulation may be necessary for deeper excisional or wedge biopsies.
- Sterile ointment and bandage material
- Sterile petrolatum is preferred because it has no higher rate of infection than topical antibiotics, but carries a significantly lower risk of allergic reactions [5]
- Nonstick surgical dressing and hypoallergenic tape
Personnel
A skin biopsy can be performed by a single clinician; however, having an assistant can increase efficiency and improve the procedural workflow.
Preparation
Although performing a skin biopsy remains technically straightforward, selecting the appropriate biopsy type and site plays a critical role in obtaining a diagnostically useful sample. Careful planning ensures that the chosen technique captures sufficient tissue while minimizing both cosmetic and functional impact.
All necessary supplies should be prepared and readily accessible before beginning the procedure to promote efficiency and reduce the risk of complications. High-quality clinical photographs should be obtained prior to the biopsy for both documentation and diagnostic purposes, creating a valuable record of the lesion’s appearance.
Once the biopsy site has been selected, the area should be wiped with alcohol to decrease the bacterial count and remove skin oils. For pink lesions, marking the site before injecting the anesthetic is important, as these lesions often blanch (lose color) when injected.
Technique or Treatment
Site Selection for Skin Biopsy
Appropriate site selection remains crucial. When eruptions present with multiple morphologies, more than 1 site may need sampling. Blistering conditions often require both lesional and perilesional biopsies, sometimes using different transport media depending on planned studies, eg, direct immunofluorescence, tissue culture, or fungal culture. Consulting the pathologist in advance can ensure correct equipment and specimen handling. Providing the pathologist with relevant clinical information—including history, lesion duration, distribution, symptoms, and differential diagnosis—significantly improves the likelihood of obtaining a meaningful and clinically useful histopathologic interpretation.
Skin Biopsy Techniques
Following effective preparation of the skin biopsy site, the appropriate skin biopsy method should be selected based on various clinical factors of the lesion (eg, type, depth, and location).
Shave technique
The shave technique represents the simplest form of an incisional biopsy. Using a scalpel or handheld blade, the clinician scoops a skin sample of the desired thickness. This approach is most effective for treating superficial skin conditions or for diagnosing nonmelanoma skin cancers (NMSC). However, some NMSCs display more aggressive histologic features in deeper layers that may be missed with a superficial biopsy. During the procedure, the nondominant hand stretches the skin while the dominant hand maneuvers the scalpel or flexible blade to obtain the specimen. Alternatively, the skin may be squeezed to access deeper tissue, though this can create a more depressed wound.
Scissor biopsy
Scissor biopsies serve as an alternative incisional option, particularly for small, pedunculated lesions, such as skin tags, or in regions with thin, redundant skin, like the eyelids or axillae. The technique involves gently grasping the lesion’s base with forceps before snipping it at the base.
Punch biopsy
The punch biopsy provides a full-thickness specimen using a cylindrical blade, making it valuable for diagnosing inflammatory dermatoses that involve deeper skin layers or subcutaneous fat. Punch biopsy also serves as a method for excising small lesions or sampling larger pigmented lesions when complete excision is not feasible. Multiple punches may be performed to capture representative areas of a larger lesion. Disposable punches are preferred for their sharpness and reliability. Sizes typically range from 2 mm to 8 mm, and clinicians must balance adequate sampling with cosmetic outcomes, especially on the face. The skin should be stretched perpendicular to relaxed skin tension lines while rotating the punch back and forth until full penetration is achieved. The specimen is lifted carefully with forceps or a skin hook to avoid crushing, and the base is cut with fine scissors. Once released, the wound assumes an elliptical shape. Attention to anatomy remains critical to avoid injury to underlying structures.
Wedge biopsy
A wedge biopsy involves the removal of a narrow, wedge-shaped, or elliptical tissue section from a larger lesion and is often used when full excision is impractical. This technique typically involves a cross-section from the center of the lesion extending into adjacent normal skin. Orienting the ellipse radially provides an optimal architectural view. Wedge biopsies hold particular value in diagnosing keratoacanthoma, where architecture is essential for diagnosis, and in evaluating suspected melanomas when excision is not feasible due to the lesion's size or location. Adequate depth and inclusion of lesional and non-lesional skin improve histopathologic assessment.
Excisional biopsy
An excisional biopsy is the preferred approach for small lesions or suspected malignant melanoma, provided the size and location permit.[6][7][8] Adequate depth is critical because tumor thickness (Breslow depth) determines staging and guides treatment decisions. Transection of the base may compromise staging accuracy. Excisional biopsies are typically performed with a scalpel, removing the full lesion, including the dermis and a small portion of subcutaneous tissue. Alternatively, a deep shave excision performed with a razor or flexible blade can be considered an excision if it extends into the adipose tissue.
Hemostasis Techniques
Hemostasis following biopsy depends on wound size and depth. Small or superficial wounds often respond well to chemical agents such as aluminum chloride or Monsel’s ferric subsulfate. Punch biopsy sites may require interrupted sutures or Gelfoam. Absorbable sutures offer the benefit of eliminating the need for suture removal. Excisional sites often require electrocoagulation, and chemical anticoagulants should be avoided when closure with sutures is planned. Once hemostasis is achieved, sterile petrolatum and a nonstick dressing are applied, with gauze pressure secured by hypoallergenic tape. Placing tape strips perpendicular to the incision line reduces tension and helps prevent wound dehiscence.
Complications
Complications of skin biopsy may include:
- Bleeding at the biopsy site
- Hematoma
- Infection
Pressure dressings and ice can help reduce bleeding and hematoma formation. Sutures may be needed for hemostasis. Uncontaminated skin biopsy procedures have an infection rate of less than 1%.[9][10] As such, prophylactic antibiotics are generally not indicated, but can be considered for high-risk patients.[11] Adverse reactions to skin biopsy are rare but may include hypersensitivity reactions or a vasovagal response. If a vasovagal episode occurs, the patient should be placed in the Trendelenburg position or lie flat with legs elevated.
Clinical Significance
Patients should be advised that the biopsy site will heal with some degree of scarring. Shave biopsies generally heal within several weeks and often form a crust during the process. The resulting scar may appear hypopigmented or hyperpigmented, depending on the individual's healing response.
The primary purpose of skin biopsies is to assist in the diagnosis or confirmation of a suspected condition. The procedure provides tissue samples that enable detailed histopathologic evaluation, facilitating the characterization of a skin lesion or eruption. Adequate sampling remains essential to ensure accurate interpretation and appropriate clinical management. Providing the pathologist with detailed clinical information, including the patient’s history, the exact biopsy location, and the differential diagnosis, holds equal importance. This communication allows the pathologist to interpret the specimen accurately and in the appropriate clinical context, thereby maximizing the diagnostic value of the procedure.
With a low overall risk profile, skin biopsies can be safely and routinely performed in both inpatient and outpatient settings. Proper technique, site selection, and aftercare contribute to favorable outcomes, making the procedure a reliable and widely used diagnostic tool in dermatologic practice.
Enhancing Healthcare Team Outcomes
Skin biopsy is a widely used diagnostic procedure in dermatology that provides essential tissue samples for histopathologic evaluation of skin and systemic diseases with cutaneous manifestations. Techniques such as shave, punch, scissor, wedge, and excisional biopsies are selected based on lesion type, depth, location, and patient-specific considerations. The procedure carries a low risk and can be safely performed in both inpatient and outpatient settings. However, proper technique and careful planning are vital to minimize complications such as bleeding, infection, scarring, or functional impairment.
Effective patient-centered care in skin biopsy requires collaboration among physicians, general practitioners, advanced practitioners, nurses, pharmacists, and other health professionals. Clinicians must possess technical skill in biopsy techniques, judgment in site selection, and knowledge of contraindications and specimen handling. Nurses play a central role in patient education, wound care, and monitoring for complications. Pharmacists provide guidance on managing anticoagulation, allergies, and reducing the risk of postoperative pain or infection. Interprofessional communication, particularly between clinicians and pathologists, ensures the quality of specimens and the meaningful interpretation of results. Coordinated teamwork enhances diagnostic accuracy, strengthens patient safety, and promotes efficient, high-quality dermatologic care.
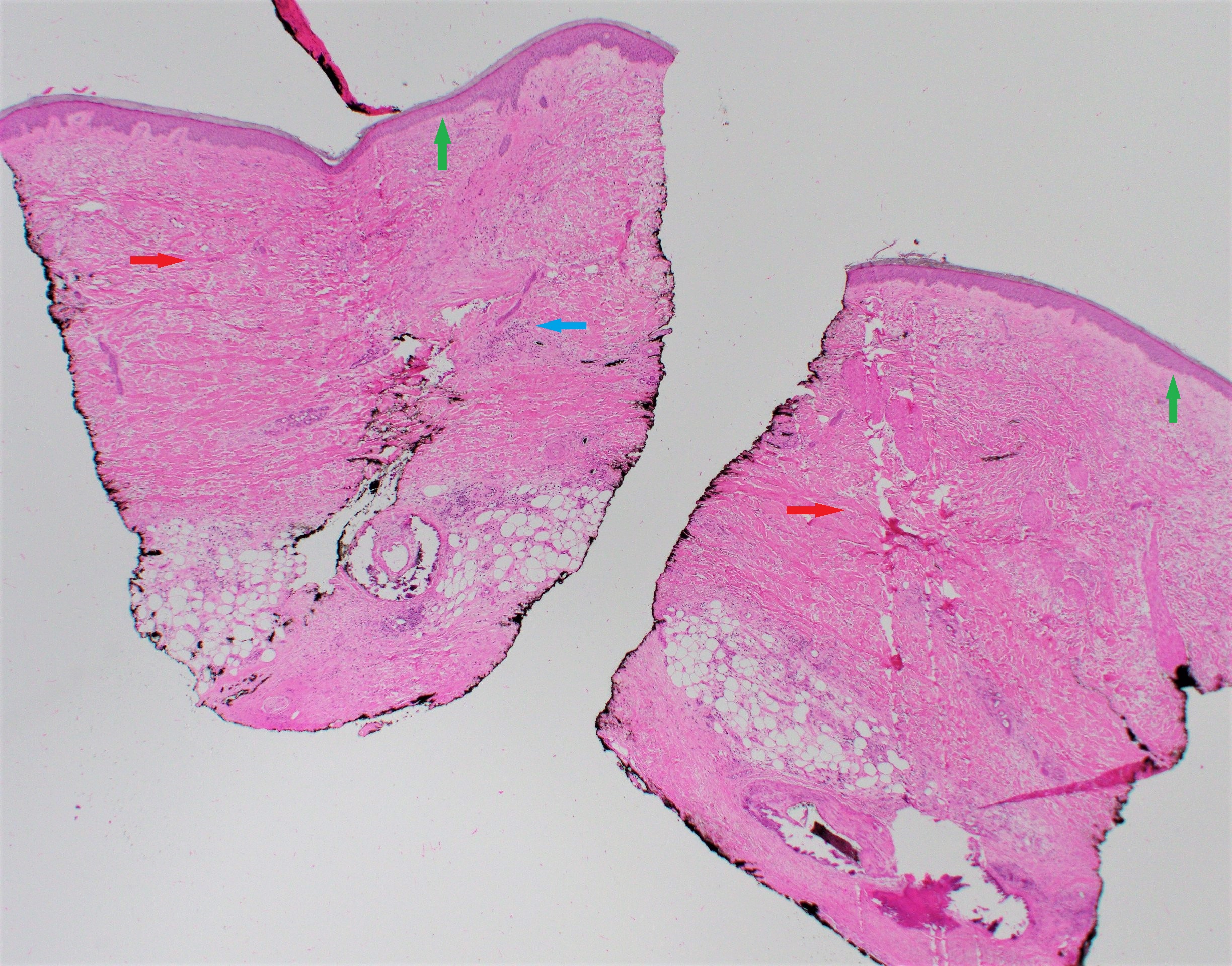
Media
(Click Image to Enlarge)
References
Yang S, Kampp J. Common Dermatologic Procedures. The Medical clinics of North America. 2015 Nov:99(6):1305-21. doi: 10.1016/j.mcna.2015.07.004. Epub 2015 Sep 11 [PubMed PMID: 26476254]
Elston DM, Stratman EJ, Miller SJ. Skin biopsy: Biopsy issues in specific diseases. Journal of the American Academy of Dermatology. 2016 Jan:74(1):1-16; quiz 17-8. doi: 10.1016/j.jaad.2015.06.033. Epub [PubMed PMID: 26702794]
Iyengar S, Yeager DG, Cohen JL, Ozog DM. Update and Review of Bleeding Considerations in Dermatologic Surgery: Anticoagulants and Antiplatelets. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2020 Feb:46(2):192-201. doi: 10.1097/DSS.0000000000002266. Epub [PubMed PMID: 31743247]
McKay W, Morris R, Mushlin P. Sodium bicarbonate attenuates pain on skin infiltration with lidocaine, with or without epinephrine. Anesthesia and analgesia. 1987 Jun:66(6):572-4 [PubMed PMID: 3034106]
Lin WL, Wu LM, Nguyen TH, Lin YH, Chen CJ, Huang WT, Guo HR, Chen YH, Chuang CH, Chang PC, Hung HK, Chen SH. Topical Antibiotic Prophylaxis for Preventing Surgical Site Infections of Clean Wounds: A Systematic Review and Meta-Analysis. Surgical infections. 2024 Feb:25(1):32-38. doi: 10.1089/sur.2023.182. Epub 2023 Dec 19 [PubMed PMID: 38112687]
Level 1 (high-level) evidenceMiedema J, Zedek DC, Rayala BZ, Bain EE 3rd. 9 tips to help prevent derm biopsy mistakes. The Journal of family practice. 2014 Oct:63(10):559-64 [PubMed PMID: 25343153]
Cheng R, Bialas RW, Chiu ST, Lawrence TJ, Lesesky EB. Punch biopsy vs. shave biopsy: a comparison of margin status of clinically atypical pigmented lesions. The British journal of dermatology. 2015 Sep:173(3):849-51. doi: 10.1111/bjd.13830. Epub 2015 Aug 19 [PubMed PMID: 25864555]
Sharma KS, Lim P, Brotherston MT. Excision versus incision biopsy in the management of malignant melanoma. The Journal of dermatological treatment. 2016:27(1):88-90. doi: 10.3109/09546634.2015.1034083. Epub 2015 Apr 17 [PubMed PMID: 25886086]
Matos S, Sturm B, Buhnerkempe M, Larson R, Wilson M. Risk Factors for Infection After Minor Dermatologic Procedures: A Case-Control Study. Dermatologic surgery : official publication for American Society for Dermatologic Surgery [et al.]. 2021 Dec 1:47(12):1562-1565. doi: 10.1097/DSS.0000000000003163. Epub [PubMed PMID: 34417389]
Level 2 (mid-level) evidenceYasui Y, Kato H, Oda T, Nakamura M, Morita A. Complications and risk factors of punch biopsy: A retrospective large-scale study. The Journal of dermatology. 2023 Jan:50(1):98-101. doi: 10.1111/1346-8138.16585. Epub 2022 Sep 24 [PubMed PMID: 36151785]
Level 2 (mid-level) evidenceAkiyama Y, Norimatsu Y, Ohno Y. Prophylactic antimicrobials may not be needed to prevent surgical site infection after skin biopsy: a retrospective study. Antimicrobial resistance and infection control. 2022 Feb 16:11(1):35. doi: 10.1186/s13756-022-01077-z. Epub 2022 Feb 16 [PubMed PMID: 35172906]
Level 2 (mid-level) evidence