Introduction
Presbyopia, derived from the Greek words presbys ("old") and ops ("eye"), is the age-related decline in the eye's capacity to concentrate on proximal objects.[1] This condition represents a widespread refractive anomaly that typically begins in the early to mid-40s and progresses into the sixth decade of life. Although considered physiological and part of aging, presbyopia can considerably hinder an individual's visual capabilities and overall quality of life. The disorder arises from alterations in the crystalline lens and its adjacent components, which collectively reduce the eye's ability to accommodate.[2] These structural alterations are not singular; they are integral to a comprehensive aging process affecting ocular tissues. The human eye relies on the dynamic interplay among the ciliary body, zonular fibers, and crystalline lens for accommodation.[3] In youth, the crystalline lens is supple and malleable, enabling it to alter its shape in reaction to ciliary muscle contraction. This alteration enhances the lens's refractive capability, facilitating clear vision at proximal distances. With advancing age, the lens becomes less flexible and hardens due to protein cross-linking and compaction, whereas the ciliary muscle may experience a reduction in contractile power.[4]
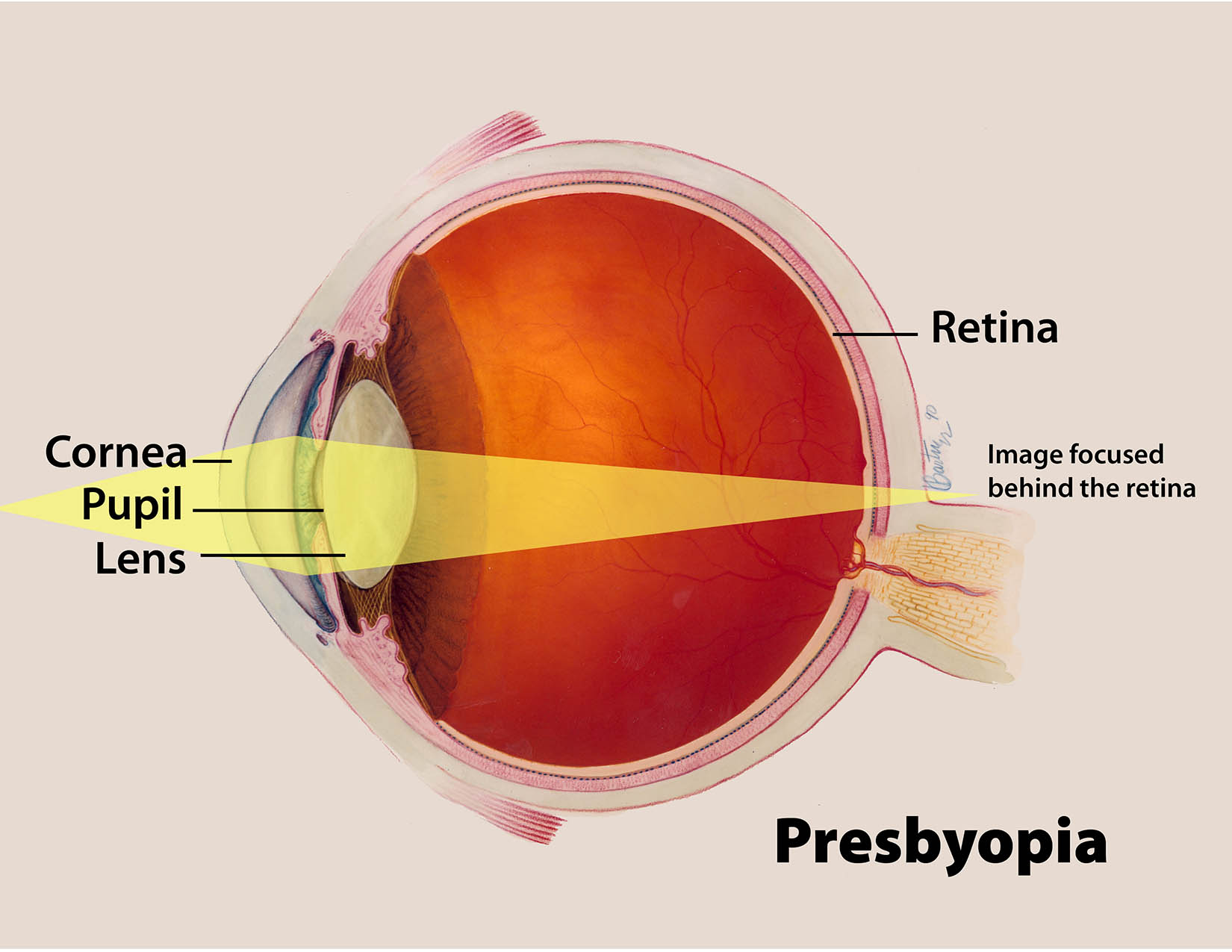
Age-related alterations result in a diminished amplitude of accommodation, a characteristic of presbyopia. The image is focused behind the retina, which results in impaired near vision (see Image. Presbyopia: Age-Related Loss of Near-Vision Focus). The natural history of presbyopia generally commences with minor challenges in reading small text or perceiving nearby objects distinctly, particularly in dim lighting conditions. Initial effects are frequently mitigated by distancing reading material or enhancing ambient illumination. Eventually, these compensations prove insufficient, requiring the utilization of corrective lenses.[5] The transition is incremental, with near visual tasks getting progressively more difficult, ultimately necessitating stronger near enhancements in eyewear.
Progression patterns may vary among individuals based on factors such as initial refractive status, environmental exposure (notably to UV light), and systemic disorders, including diabetes mellitus.[6] Individuals with hyperopia frequently experience presbyopic symptoms earlier than individuals with myopia due to their heightened dependence on accommodation for both distant and near tasks.[7] In addition, variations in ethnicity and geography regarding the development and severity of presbyopia have been observed, with individuals residing closer to the equator frequently exhibiting symptoms at an earlier age, possibly due to cumulative environmental stressors.[8]
Among the various causes of near visual impairment, presbyopia is the most important and common cause in older adults.[9] In a study of a population from the Brazilian Amazon region, presbyopia accounted for 71.8% of all cases of near visual impairment, whereas cataract and pterygium accounted for 16.5% and 2.5%, respectively. This pattern is consistent globally. Presbyopia is a growing global issue affecting over a billion people worldwide.[10] The increase in the aging population has prompted healthcare professionals to find effective ways to manage the situation through various nonsurgical and surgical interventions. This activity discusses these surgical and nonsurgical interventions for presbyopia correction.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The primary cause of presbyopia is the age-related decline in the eye's accommodative capacity, mostly influenced by biomechanical alterations in the crystalline lens.[11] Various theories have been proposed to describe the mechanism involved in presbyopia. Helmholtz's theory, Schachar's theory, and the Catenary theory of Coleman are the most discussed ones. Helmholtz's theory states that the ciliary muscle contraction results in the relaxation of zonules and an increase in the convexity of the anterior lens capsule.[12] Schachar's theory, in contrast to Helmholtz's theory, says that the ciliary muscle contraction results in increased tension of equatorial zonular fibers with simultaneous relaxation of anterior and posterior zonular fibers. This concept results in the steepening of the anterior central part of the lens with flattening of the lens periphery.[13] The Catenary theory of Coleman proposes that with ciliary muscle contraction, a pressure gradient develops from the vitreous compartment to the aqueous compartment, resulting in the steepening of the anterior lens capsule in the center.[14]
With advancing age, lens proteins undergo glycation and oxidation, leading to cross-linking and increased rigidity. This alteration markedly diminishes the lens's capacity to alter its shape, which is crucial for focusing on proximal objects. The decline in lens flexibility is regarded as the primary cause contributing to presbyopia,[15] although other factors, including alterations in lens geometry and increasing lens thickness, also play ancillary roles.[16]
The function of the ciliary muscle in the progression of presbyopia also seems to play a fundamental role in this condition.[3] Although age-related alterations in muscle contractility have been noted, new research indicates that muscle function is largely preserved in older age demographics. The transfer of contractile force to the lens through the zonules may be compromised due to age-related alterations in the extracellular matrix or the zonular fibers themselves. Consequently, although the ciliary muscle has functional capability, the diminished reactivity of the lens restricts efficient accommodation.[17]
Environmental and lifestyle factors also influence the initiation and progression of presbyopia. Prolonged exposure to UV radiation is believed to accelerate oxidative damage to the lens, thereby increasing its stiffness.[18] Likewise, professions necessitating extended periods of near vision may manifest presbyopic symptoms sooner, although this does not seem to affect the inherent schedule of physiological development.[19] Systemic illnesses, including diabetes mellitus and cardiovascular diseases, may contribute, possibly through microvascular alterations that affect the ocular structures responsible for accommodation.[20] Hormonal and sexual distinctions represent an increasingly significant topic of inquiry. Some studies have reported that presbyopia may occur earlier in women than in men, with a slightly higher prevalence in females, possibly due to hormonal fluctuations that influence lens metabolism or ocular blood circulation.[21] Moreover, lifestyle factors such as smoking and alcohol consumption have been loosely associated with the earlier onset of presbyopia.[22] Although the literature mentions these factors as potential influences on presbyopia, their actual impact remains unproven. Collectively, these findings highlight the multifaceted nature of presbyopia, encompassing both internal aging mechanisms and extrinsic modifiable risk factors.
Epidemiology
Presbyopia is a prevalent visual impairment affecting around 1.8 billion individuals worldwide.[19][23] By 2030, this number is expected to increase to more than 2.1 billion.[24] This condition is typical and physiological in individuals older than 50, although the precise age of start and severity differ among populations. Research indicates that presbyopia generally manifests symptomatically between the ages of 40 and 45, with nearly universal prevalence by age 60.[25] Studies have shown that more than 80% of individuals aged 40 develop presbyopia.[24] The worldwide prevalence of presbyopia is escalating as a result of an aging population and growing life expectancy. By 2050, more than 20% of the world's population is expected to be older than 60, which will have a significant impact on this condition in the near future.[26] In numerous high-income nations, the percentage of adults older than 65 is increasing swiftly, resulting in a concomitant rise in the incidence of presbyopia. The ongoing increase in smartphone and digital screen usage highlights the need to manage presbyopia, given the heightened pressure on close vision tasks in both professional and recreational contexts.[27]
The Global Burden of Disease Study indicates that uncorrected presbyopia leads to substantial productivity losses, estimated at over USD 25 billion worldwide, especially in low- and middle-income nations with restricted access to corrective glasses.[28] Gender differences are prominent in specific populations. Systematic research showed that women experience presbyopia earlier than men and are less likely to utilize corrective services in low-income settings. This age-related alteration in accommodation affects both genders, but certain studies suggest an earlier onset in women, possibly due to hormonal and vocational disparities.[29] The gender disparity may be ascribed to socioeconomic influences, cultural perspectives, and inequality in healthcare services.[30]
Environmental factors such as temperature, humidity, and geographic latitude may significantly influence the onset and progression of presbyopia.[31][32] Individuals residing in tropical climates often develop presbyopia at an early age, potentially due to increased exposure to UV radiation and various environmental stressors.[33] Regional disparities in presbyopia correction are evident in the current literature.[34] In wealthy nations such as the United States and certain regions of Europe, more than 60% of individuals with presbyopia use some correction for this condition.[35][36] Conversely, in numerous low-resource areas, less than 20% of individuals with presbyopia have access to adequate visual aids.[37] This gap highlights the necessity for public health initiatives focused on enhancing access to affordable eye care and presbyopic correction, particularly among aging populations in underdeveloped regions.
Pathophysiology
There are various explanations about the pathophysiology of presbyopia. Among all the concepts, the increased stiffness of the crystalline lens is the most widely accepted. Presbyopia is a physiological condition wherein there is a progressive functional decline in the accommodative capacity of the crystalline lens. Clinically, it manifests as progressive difficulty in reading at the usual reading distance. In an in vitro study by Glasser and Campbell, no significant change in focal length was observed with simulated zonular tension and relaxation.[38]
The primary pathologic alteration is the reduction of lens flexibility due to protein aggregation and cross-linking. These chemical changes diminish the lens's capacity to bend and thicken in response to ciliary muscle contraction, which is essential for near vision. With age, the lens becomes increasingly rigid and sclerotic, directly leading to a reduction in accommodation. Normally, the nucleus is stiffer than the cortex in the older lens, whereas among young individuals, the cortex is stiffer than the nucleus.[39] However, the stiffness of both nucleus and cortex equalizes between the ages of 35 and 40, which is probably the cause of the onset of presbyopic symptoms around the age of 40.[40] Another important factor contributing to presbyopia is a relative change in the shape of the lens with increasing age (increased thickness of the lens), such that the vector forces exerted by zonules at the equator spread over a wider region around the equator. This change has a minimal effect on lens shape during zonular contraction and relaxation.[41]
The biomechanical connection among the ciliary muscle, zonular fibers, and lens can change over time.[42] Age-associated alterations in the extracellular matrix of the zonules and lens capsule diminish the transfer of muscle force.[43] This mechanical inefficiency, coupled with a more rigid lens, significantly undermines the dynamic accommodation mechanism. The central and peripheral lens zones experience varying degrees of compaction as they age. The core nucleus grows progressively denser and less reactive, whereas the peripheral cortex becomes thicker. This alteration in lens morphology further obstructs shape transformation. Moreover, a variation in the refractive index distribution across the lens frequently occurs, which diminishes the optical power produced by any remaining accommodative movement.[44]
The predominant clinical manifestation of presbyopia is a progressive deterioration in close visual acuity, whereas distance vision stays mostly intact, especially in emmetropic individuals.[45] Patients commonly indicate the necessity of positioning reading materials at a greater distance and may encounter ocular strain, cephalalgia, or visual fatigue following extended near duties. These symptoms result from the functional ramifications of the underlying biomechanical and biochemical alterations within the aging lens system.
Histopathology
The histological characteristics of presbyopia are most commonly observed in the aged crystalline lens and the adjacent zonular apparatus. As individuals age, the lens exhibits progressive nuclear sclerosis, marked by the compaction of lens fibers in the nucleus and the buildup of insoluble crystallin proteins.[46] These protein aggregates arise from oxidative stress and post-translational changes, including deamidation, glycation, and truncation, which render the lens rigid and less able to deform.[47] Histologically, the lens reveals a diminished gradient refractive index and a reduction in transparency in more advanced phases.[47][22] A key histological alteration in the aging lens is the formation of a denser, more rigid nucleus encased by an augmented cortex.[48]
The zonular fibers connecting the lens capsule to the ciliary body exhibit histological signs of aging. The microfibrils fragment and exhibit degenerative alterations in their elastic components, such as fibrillin. This degradation hinders the transfer of mechanical forces from the ciliary body to the lens capsule.[43] The lens capsule expands with age, particularly on the anterior surface, diminishing its flexibility and contributing to the decline in accommodation. Although these changes may appear subtle under optical microscopy, they are well-documented with electron microscopy. A notable histological finding is the buildup of advanced glycation end-products within the lens matrix, especially in the nucleus.[49] Advanced glycation end-products facilitate the cross-linking of lens proteins and extracellular matrix constituents, enhancing rigidity and resistance to shear deformation. In addition, oxidative damage to mitochondrial DNA and lipid peroxidation have been detected in lens cells, corroborating the hypothesis that cumulative oxidative stress plays a pivotal role in the etiology of presbyopia. Histopathological findings indicate a gradual degenerative process impacting both the cellular and extracellular structures of the lens and its suspensory apparatus.[46]
History and Physical
A comprehensive history is crucial for diagnosing presbyopia, especially in middle-aged and older individuals with vision issues. Patients generally report a progressive difficulty concentrating on nearby objects, particularly in low-light conditions or during extended near tasks. Common symptoms include ocular strain, exhaustion, cephalalgia, and a tendency to hold reading materials at arm's length. These concerns are often reported in the absence of notable distance vision issues, especially among individuals with emmetropia. Some patients report variable eyesight when transitioning between near and distant activities. The physical examination should commence with a thorough evaluation of visual acuity at both distance and near. During the examination, the light source should always be behind the patient. The light source in front of the patient can result in the pin-hole effect, which can falsely increase the depth of focus. Asthenopic symptoms appear relatively earlier in patients with longer screen time exposure due to latent accommodative dysfunction.[50] Other symptoms include delayed focusing of near and distance, squinting, drowsiness during near work, and a need for bright light for reading.[51]
Presbyopia is characterized by a notable decline in close visual acuity, frequently accompanied by normal or near-normal distance acuity. The severity of near vision impairment can be assessed using Jaeger or Rosenbaum cards at a standardized reading distance.[52] Objective refraction and assessment of accommodative amplitude—typically with the push-up or minus lens technique—validate the diagnosis. Accommodation is deemed functionally inadequate when the near point exceeds the patient's usual reading distance.
Slit-lamp examination is crucial for assessing the anterior segment, especially to exclude associated ocular surface conditions such as dry eye, which may intensify near vision problems. The examiner must evaluate pupillary responses and ocular movement to rule out neurological etiologies of accommodative failure.[53] Intraocular pressure measurement and fundus examination are essential to rule out glaucoma and age-related macular degeneration, particularly in older patients. The patient's occupational and lifestyle requirements must be meticulously evaluated during the history-taking process, especially regarding their reading habits, digital screen usage, and any hobbies or professional pursuits necessitating accurate near vision.[54] The influence of presbyopia on quality of life can differ markedly depending on these characteristics. Identifying patients who rely significantly on intermediate or near tasks, such as computer work or complex manual labor, is essential for directing personalized care.[55] Patient-reported outcome measures, such as the Near Activity Visual Questionnaire (NAVQ), can clarify the functional impact of presbyopia and guide treatment strategies.[56]
Evaluation
In presbyopia, the near point of accommodation recedes beyond the usual reading distance.[57] The Royal Air Force rule is used to calculate the near point of accommodation and the amplitude of accommodation.[58] The amplitude of accommodation decreases with age. Evaluation is subjective. Patients are asked to keep the near reading target at the usual reading distance, and lenses are added. The minimum value of the plus lens, which makes vision clear enough to read the last line of the reading chart at the usual reading distance, is considered to be the dioptric power that has to be prescribed.[59]
The assessment of presbyopia commences with a thorough ophthalmologic examination, encompassing both subjective and objective evaluations of refractive error and accommodative capability. The fundamental aspect of evaluation is the assessment of visual acuity at different distances, especially near vision, which is predominantly impacted. Alongside refractive testing, clinicians must conduct a comprehensive evaluation of both the anterior and posterior segments using slit-lamp biomicroscopy and ophthalmoscopy. These evaluations assist in identifying comorbid disorders, such as cataracts, glaucoma, macular degeneration, or dry eye disease, which can influence the choice of presbyopia treatment methods. The evaluation of the tear film and ocular surface is crucial, as ocular surface disease can significantly impact the outcomes of both optical and surgical interventions for presbyopia.[5] Contemporary clinical guidelines emphasize a personalized approach. The American Academy of Ophthalmology and the American Optometric Association advocate for personalized correction tailored to the patient's visual requirements and ocular health condition.[60][61] Globally, guidelines emphasize the significance of thorough ocular evaluation and patient-centered decision-making. When considering surgical correction, such as corneal inlays or lens-based operations, supplementary diagnostic tools, including corneal topography, optical coherence tomography, and aberrometry, may be necessary to enhance results and minimize postoperative complications.
Treatment / Management
Presbyopia, a common age-related reduction in accommodative capacity, presents a significant clinical challenge that requires a tailored and comprehensive treatment approach. The primary goal of treatment is to restore adequate near vision while preserving functional distance acuity. Management strategies include optical corrections, such as glasses and contact lenses; pharmacological agents; surgical operations; and behavioral modifications. International and national recommendations emphasize the importance of tailoring treatment to the patient's visual needs, ocular health, refractive error, and lifestyle preferences. The British Contact Lens Association (BCLA) CLEAR reports emphasize that effective presbyopia correction is crucial for maintaining quality of life in older individuals, particularly in digitally demanding settings.[62] Optical correction is the predominant initial strategy, especially in the early stages of presbyopia. Available options include single-vision reading glasses, bifocals, and progressive addition lenses. Progressive addition lenses are favored for their aesthetic appeal and seamless transition across viewing fields. Nonetheless, adaptation may prove difficult, especially for individuals with vestibular sensitivity or those engaged in prolonged, intermediate tasks such as computer work. Bifocals offer a distinct delineation between distance and near focal areas; however, they result in intermediate blurriness and image displacement. Degressive lenses, a type of progressive addition lenses tailored for intermediate and near vision, are increasingly advised for patients with significant visual task requirements when working at computer distances.
Nonsurgical Options
Spectacles: Single-vision or monovision lenses are a relatively cheaper option. Patients can comfortably read at near distances; however, separate distance glasses may be required if individuals have a refractive error for distance vision.[63] Bifocal lenses are of great help, especially for individuals who have both refractive errors for distance vision and presbyopia. However, bifocals are more expensive than single-vision lenses.[59] Bifocal corrects for near and distance vision; however, intermediate vision is unaffected and blurry. Progressive lenses were introduced to address the issue of blurred vision at intermediate distances.[62] Progressive lenses are considered to be the most expensive of all. However, the quality of vision is better with progressive lenses, and the duration of use of glasses increases from 40% to 60% during working hours.[64] Neither bifocal nor progressive glasses are tolerated well initially and may cause nausea and dizziness. Due to an alteration in vision quality at the junction of lenses, the patients may have difficulty judging depth while walking. However, with continued use, the symptoms resolve within 2 to 3 weeks.(B2)
- Bifocal lenses [65]
- The Bifocal lenses can be classified based on their make as:
- Fused bifocal: A depression curve in the crown glass is fitted with a flint button
- Solid bifocal: Made from a single material
- Cemented bifocal: A segment is glued onto a single vision lens
- Split bifocal: Two separate lenses are held together with a frame
- Based on the design, bifocal lenses are further categorized into:
- D-seg or straight top bifocal lens
- Round-segmented bifocal lens
- Executive bifocal lens
- Kryptok lens: In the Kryptok lens, the segment for near-vision correction is round. The advantage of the Kryptok lens is that the transition is not visible from outside, making it cosmetically appealing compared to D-seg, where the segmentation is very well demarcated. However, image jump can occur with all these designs.
- The Bifocal lenses can be classified based on their make as:
- Progressive or multifocal lenses have a gradient of power for near add in the central zone. The peripheral part of the lens may cause distortion.[66] (B2)
Contact lenses: Contact lenses can help manage presbyopia in two ways. One option is monofocal contact lenses, which correct one eye for distance vision and the other for near vision. Typically, the dominant eye is corrected for distance, a concept known as monovision. The advantage of monovision is that it provides good clarity of vision over a range of distances; however, contrast sensitivity and stereopsis are reduced.[67]
The correction of presbyopia with contact lenses has markedly progressed. There are multifocal contact lenses with concentric refractive designs available to correct distance, intermediate, and near vision.[68] Multifocal contact lenses utilize concentric or aspheric optics to achieve simultaneous focus at various distances, thereby ensuring adequate visual acuity for close, intermediate, and distant vision. The BCLA CLEAR 2024 report reveals that more than 40% of patients with presbyopia who use contact lenses are currently prescribed soft multifocal lenses, indicating a global shift towards these technologies due to advancements in lens materials, optics, and comfort.[62] Rigid gas-permeable multifocal and hybrid lenses remain viable alternatives for patients with high astigmatism or corneal irregularities.[69]
Pharmacological approach: Novel pharmacological treatments seek to target the fundamental pathology or improve pseudo-accommodation. Pilocarpine 1.25% ophthalmic solution, sanctioned by the Food and Drug Administration (FDA) in 2021 under the brand name Vuity, has demonstrated efficacy in enhancing near vision through miosis induction and depth of focus augmentation.[70][71] Nonetheless, its effects are transient, generally persisting for 6 to 10 hours, with potential adverse effects including headache, brow discomfort, and diminished night vision resulting from pupil constriction.[72] Additional agents under scrutiny are lens-softening drops designed to reinstate lens elasticity, including UNR844 (lipoic acid choline ester).[73] However, further data are required to validate long-term efficacy and safety.(B3)
In addition to monotherapies such as pilocarpine, novel pharmacological compounds are being investigated to enhance the equilibrium between effectiveness and tolerance in the treatment of presbyopia.[74][75] Aceclidine, a parasympathomimetic agent, is now undergoing clinical trials. RX-100 is composed of a muscarinic antagonist and an agonist that contains tropicamide and aceclidine, which produce miosis while limiting ciliary muscle contraction.[76] This targeted approach may diminish the prevalence of typical adverse effects linked to conventional miotics, such as headaches and visual disturbances, while simultaneously improving near vision.[77] Preliminary clinical findings are promising, indicating a more pleasant user experience with no impact on distant vision; nevertheless, further phase III trials are necessary to confirm its long-term safety and efficacy. Several combination treatments are attracting interest for their ability to enhance therapeutic effects through synergistic pathways. A fixed-dose combination of carbachol and brimonidine has shown the ability to maintain miosis and improve near visual acuity for a long period.[78] Carbachol, a cholinergic agonist, induces pupillary constriction, whereas brimonidine, an alpha-2 adrenergic agonist, enhances this action by decreasing aqueous humor production and prolonging the pupillary dilation delay.[79] Initial research suggests that this combination can sustain functional near vision for as long as 8 hours with a benign adverse-effect profile, positioning it as a viable option for future clinical use in presbyopia treatment.(B2)
Surgical Options
Corneal procedures: Corneal surgical techniques for presbyopia typically focus on altering corneal curvature to improve near vision, frequently by creating a multifocal effect. One of the most well-known methods is monovision with laser refractive surgery, commonly performed through laser-assisted sub-epithelial keratectomy (LASIK) or photorefractive keratectomy (PRK), when one eye is corrected for distant vision and the other for near vision.[80] Although successful, monovision may impair binocular vision and depth perception, necessitating comprehensive patient counseling and adaptation.[81] Innovations in corneal ablation profiles have led to the development of procedures including central steep island induction, decentered steep areas, and mid-peripheral near-vision zones.[82] Each technique aims to alter the corneal configuration to enhance depth of focus.[83] The central steep island and global optimization of curvature and asphericity have demonstrated encouraging outcomes in improving close vision while preserving satisfactory quality for distance vision. Nonetheless, personalized ablations may lead to optical distortions, and interventions such as creating a central steep island are particularly challenging to rectify if the results are unsatisfactory.[84] Conductive keratoplasty is a non-laser technique that uses radiofrequency radiation to contract mid-peripheral corneal collagen fibers, resulting in an increased curvature of the central cornea.[85] Although initially helpful, its outcomes often diminish with time, constraining its long-term usefulness. Intracorneal inlays, shown by the Kamra small-aperture inlay, provide a novel corneal intervention.[86] These devices, embedded in the corneal stroma, operate through the pinhole effect, restricting peripheral light beams to enhance depth of focus. The inlay is often placed in the non-dominant eye through a pocket generated by a femtosecond laser. Some patients experience enhanced near vision without compromising distant acuity; nonetheless, potential concerns include corneal haze, implant decentration, and the need for explantation in cases of dissatisfaction.[87] Microlens inlays, intended to modify refractive power by altering the refractive index, have been investigated; however, several devices have been withdrawn due to safety or regulatory issues.[88](B2)
Scleral procedures: Surgical intervention involving the sclera is based on the hypothesis that age-related presbyopia results from biomechanical rigidity of the ocular tissues around the ciliary body. Scleral expansion treatments, including the implantation of polymethyl methacrylate rings, such as the VisAbility Micro-Insert System, in the ciliary muscle area, seek to restore accommodative amplitude by mechanical expansion of the scleral wall. Posterior radial scleral incisions are designed to diminish scleral stiffness and improve ciliary muscle mobility.[89] Although initial findings suggested some advantages, further research has raised concerns about the repeatability, longevity, and safety of these treatments. The majority lack widespread acceptance or FDA approval due to insufficient evidence.
Monovision with intraocular implant: For patients with considerable ametropia or presbyopia who are not candidates for corneal correction, monovision attained by intraocular lens implantation is a viable surgical alternative. Typically performed during refractive lens exchange or cataract surgery, this approach uses monofocal intraocular lenses to correct one eye for near vision and the other for distance vision. Although helpful, some individuals may experience difficulties with depth perception and require time to adjust.
Phakic intraocular lenses: Phakic intraocular lenses are implanted lenses that maintain the native crystalline lens while rectifying refractive errors.[90] Both anterior chamber (angle-supported or iris-claw) and posterior chamber designs are accessible.[91][92] Recent advancements have unveiled multifocal phakic intraocular lenses, which concurrently correct both distant and close vision. Despite their potential, these lenses are often designated for patients who are ineligible for corneal refractive surgery and continue to raise apprehensions over endothelial cell depletion and cataract development with prolonged usage.[93]
Clear lens extraction followed by intraocular lens implantation: Clear lens extraction, also known as refractive lens exchange, is increasingly favored for treating presbyopia, particularly among older individuals with reduced accommodation and concurrent refractive anomalies. Planned myopic astigmatism after cataract surgery gives some pseudo-accommodation.[94] Monovision with monofocal intraocular lenses is a valid option; however, the visual outcome is inferior to that of multifocal intraocular lenses.[95] After the extraction of the clear crystalline lens, multifocal, trifocal, or extended depth of focus intraocular lenses may be implanted. Trifocal intraocular lenses exhibit enhanced intermediate vision relative to conventional bifocal lenses.[96] Recent quadrifocal and extended depth of focus lenses seek to improve depth of field while reducing photic phenomena, including glare and halos.[97][98] Nonetheless, light attenuation and diminished contrast sensitivity persist as significant constraints, particularly in low-light environments. Asymmetric intraocular lens designs have been created to replicate natural accommodation more accurately.[99] These lenses incorporate a sector-shaped near-vision zone, often located inferiorly, enhancing reading capability while maintaining distance acuity and contrast sensitivity. Preliminary results indicate that, while still being assessed, they may offer a more physiological visual experience with reduced compromises; however, extensive misalignment can occur in rare cases.[100](B3)
Differential Diagnosis
Presbyopia, a prevalent and anticipated age-related refractive disorder, must be carefully distinguished from other ocular illnesses and functional vision issues that may resemble its symptoms. The primary clinical characteristic of presbyopia is a gradual deterioration of near vision resulting from the diminished accommodating ability of the crystalline lens. However, many patients exhibit nonspecific symptoms, including eye strain, reading difficulties, blurred near vision, and headaches, all of which may potentially result from binocular vision problems, accommodative dysfunctions, early cataracts, or uncorrected refractive errors. Consequently, formulating a differential diagnosis is crucial for effective care and for preventing misdiagnosis, especially in younger or atypical patients.
Accommodative insufficiency, a condition not typically associated with age, commonly affects younger adults or adolescents and resembles presbyopia; however, it arises from a failure of the accommodative system rather than age-related changes in the lens.[101] Individuals with accommodative insufficiency may encounter variable near vision, eye strain, and difficulty maintaining near tasks.[102] In contrast to presbyopia, accommodative amplitude in these individuals can occasionally be enhanced with vision therapy, and the disease may be reversible. Binocular vision anomalies, including convergence insufficiency or excess, must be ruled out, particularly when patients experience diplopia or frontal headaches when reading.[103] These diseases may simulate presbyopic symptoms and are generally diagnosed through cover testing, near point of convergence evaluation, and fusional reserve assessment.
Latent hyperopia is a significant factor in the differential diagnosis.[104] In such cases, the patient may possess sufficient distant vision yet encounter strain during near tasks due to an undetected hyperopic refractive defect that necessitates excessive accommodative exertion. This condition can especially impact younger patients who retain accommodation reserves yet are starting to exhibit signs of visual fatigue. Cycloplegic refraction is crucial for identifying latent hyperopia, particularly in patients younger than 45 exhibiting early presbyopia symptoms. Inability to recognize this condition may lead to an incorrect diagnosis of presbyopia and inappropriate treatment.
Initial nuclear sclerotic cataracts may exhibit symptoms akin to presbyopia.[105] Patients may experience a transition to myopia or, conversely, enhanced near vision, a condition referred to as second sight. In such instances, conventional refraction may erroneously indicate the resolution of presbyopia when the actual underlying condition is lenticular opacification. Slit-lamp biomicroscopy is crucial for identifying initial nuclear alterations that may not yet substantially affect visual acuity but signify the commencement of cataract development.
Dry eye syndrome and digital eye strain, both increasingly prevalent due to prolonged screen exposure, can cause near vision blurriness and discomfort that resemble presbyopia, particularly in individuals with significant visual requirements at intermediate and near distances.[106]
Specific neurological disorders, such as progressive supranuclear palsy and cranial nerve palsies, can hinder accommodation or induce convergence impairments, leading to challenges with near vision.[107] Although uncommon, these disorders should be considered when the clinical presentation deviates from age-related norms or when neurological symptoms are present. A comprehensive history and neurological evaluation are required in these instances. The BCLA CLEAR review report emphasizes that a definitive diagnostic approach must consistently exclude non-presbyopic factors contributing to near-vision loss, particularly when patients present atypically in terms of age, symptoms, or responsiveness to corrective trials.[108]
Ocular conditions affecting near vision include:
- Macular and retinal diseases: In macular diseases, vision does not improve with refractive corrections, and optical coherence tomography of the retina may reveal the abnormalities.
- Diseases of the optic nerve
- Glaucoma
- Posterior subcapsular cataract: Unlike presbyopia, the near vision further deteriorates in bright light.
- Hypermetropia
- Astigmatism
Staging
Although presbyopia is conventionally viewed as a progressive age-related deterioration in accommodation, new initiatives have aimed to establish a clinically relevant staging system.[109] Staging helps categorize the severity of functional impairment and informs treatment choices, particularly in customizing optical treatments or evaluating surgical options. The 2024 BCLA CLEAR consensus review [110] recognizes the development of a viable clinical staging paradigm, principally founded on near addition requirements, near visual acuity, and related behavioral adaptations. No universally accepted staging method exists; however, expert organizations have suggested categorizing presbyopia into mild, moderate, and advanced phases based on defined clinical criteria.
Mild presbyopia typically begins between the ages of 40 and 45, characterized by initial subjective reports of near vision blurriness, particularly in low-light conditions or during prolonged reading activities. Clinically, patients frequently necessitate an increase of +0.75 to +1.25 diopters. These patients may indicate a necessity to position reading materials at a greater distance or enhance ambient illumination. Objective assessment reveals a reduced accommodative amplitude, although some residual accommodation may persist. These patients frequently benefit from single-vision reading glasses or moderate bifocal adjustments and may start using over-the-counter readers. Proper reading correction is imperative. Overcorrection results in a loss of accommodative reserve and may result in an unsynchronized convergence movement while focusing on a near object. The purpose of slight undercorrection is to let the patient use his accommodative reserves, which increases the depth of focus.
Moderate presbyopia, typically manifesting between the ages of 46 and 55, is characterized by a near addition requirement of +1.50 to +2.25 diopters. Individuals at this level encounter persistent near-vision challenges that disrupt their professional duties and everyday activities, such as using smartphones, reading, and performing computer tasks. Behavioral adaptations, such as evading extended near tasks or augmenting font sizes, become increasingly pronounced. At this juncture, visual requirements typically surpass the capabilities of single-vision reading glasses alone. Progressive addition lenses, bifocals, and multifocal contact lenses are frequently prescribed. Objective testing reveals a further decrease in accommodation amplitude and a corresponding increase in near point distance.
Advanced presbyopia, generally noted after 55, necessitates a near increase of +2.50 diopters or greater. Currently, patients exhibit negligible or absent residual accommodation and are unable to engage in near tasks without corrective devices effectively. Concurrent age-related disorders, such as early cataracts, dry eye syndrome, or retinal alterations, may also compromise visual quality. In advanced presbyopes, visual correction techniques typically involve higher-powered multifocal spectacles, specific vocational lenses for intermediate activities, or surgical interventions, such as multifocal intraocular lenses. These patients may exhibit diminished tolerance to inadequate corrections and necessitate more precise customization of visual aids.
Staging is evolving through the integration of dynamic measurements, including clear focus, defocus curves, and acuity reserve metrics, which provide quantitative data on a patient's functional vision at different distances. These measurements enable clinicians to examine actual visual performance and may be especially beneficial in research or in evaluating outcomes following therapies. Defocus curves can illustrate acuity across a range of distances and are particularly helpful in evaluating candidates for multifocal intraocular lenses or corneal inlays.[111] Although not yet common in ordinary clinical practice due to time and equipment requirements, these approaches are expected to assume a progressively significant position in future staging systems. In addition, psychometric tools such as the NAVQ [56][112] and the Presbyopia Impact and Coping Questionnaire (PICQ) [113] provide further understanding of the impact of presbyopia on daily activities. These techniques enhance the staging process by integrating the patient's perceived functional limitations and coping mechanisms. The BCLA CLEAR 2024 study highlights that these technologies are crucial for correlating clinical findings with patient-reported outcomes and enhancing the accuracy of treatment planning.[23]
Prognosis
Presbyopia typically progresses physiologically, ultimately leading to a near-total loss of accommodative ability. From a clinical perspective, the prognosis of presbyopia is clear: it is an unavoidable and permanent physiological phenomenon that impacts nearly all individuals by their mid-50s. The rate of progression may vary among individuals due to factors such as initial refractive error, age of onset, overall health, and environmental influences. The prognosis for presbyopia is generally positive, as it is non-fatal and easily controlled, with numerous treatment methods accessible. However, without suitable management, it can significantly impair quality of life, especially in communities and occupations that depend heavily on close and intermediate vision.
The earliest stage of presbyopia, which often begins in the early to mid-40s, may progress gradually. Over time, the lens progressively loses elasticity, resulting in a reduction in the amplitude of accommodation. Specific individuals may remain asymptomatic, especially myopes who can adjust by reducing their distance correction for near tasks. Emmetropes and hyperopes frequently encounter symptoms sooner and more severely. The amplitude of accommodation diminishes to below 1 diopter, generally by the late 50s or early 60s. Currently, the majority of individuals necessitate complete near correction and are unable to perform tasks at close distances without visual assistance. An essential element of prognosis relates to the enduring satisfaction and adjustment to presbyopic adjustments.[114]
Individuals who wear spectacles typically acclimate effectively to reading glasses or progressive addition lenses, although some may encounter ongoing difficulties with distortion or depth perception. Contact lens users may experience difficulties adjusting to multifocal or monovision designs, particularly in low-contrast or dynamic settings. Surgical interventions, including multifocal intraocular lenses, offer enhanced independence from spectacles but may lead to diminished contrast sensitivity and dysphotopsia.[115] Notwithstanding these potential disadvantages, patient satisfaction with multifocal intraocular lenses is generally high, particularly when patients receive thorough counseling and preoperative evaluation.[8]
The natural history of presbyopia is additionally affected by concurrent ocular disorders. The advancement of nuclear sclerosis can temporarily enhance near vision by causing a myopic shift, referred to as second sight, which may postpone the necessity for presbyopic correction. Nonetheless, this is typically succeeded by a gradual deterioration of vision resulting from cataract progression. Systemic disorders such as diabetes mellitus can affect accommodative function through autonomic neuropathy or initial lenticular alterations, resulting in unusual manifestations of presbyopia. The prognosis in these instances may be intricate and necessitate simultaneous therapy of systemic variables.
Significantly, although the mechanical loss of accommodation is irreversible, functional outcomes can be enhanced with advancements in lens technology, surgical procedures, and patient education.[116] The visual prognosis for individuals with presbyopia is highly favorable when the problem is identified and effectively treated. Recent advancements, such as pharmaceutical treatments and extended depth-of-focus optics, are expected to enhance long-term visual function and quality of life. Consequently, the clinician's responsibility extends beyond delivering suitable corrections to encompass anticipating the patient's changing demands and integrating solutions that address both functional constraints and lifestyle choices.[117]
Complications
Although presbyopia is a benign and non-progressive condition concerning ocular health risks, issues may arise due to improper management of the condition or the remedial measures used. These problems can affect visual acuity, comfort, and overall patient satisfaction. Moreover, an erroneous diagnosis or unsuitable correction may exacerbate symptoms, including visual fatigue, diminished productivity, and inadequate adaptation to visual aids, particularly in high-demand professional environments. Consequently, comprehending the range of possible complications—both iatrogenic and intrinsic—is crucial for the appropriate long-term management of presbyopia.
A common consequence is inadequate correction, leading to persistent visual difficulties. This Inadequate correction may stem from erroneous refraction, inadequately fitted spectacle lenses, or inferior contact lens designs. Multifocal contact lenses may produce overlapping or ghost images due to simultaneous vision optics, leading to diminished contrast sensitivity and visual discontent. Progressive addition lenses may induce peripheral distortion or swim effects during head motions, especially in novice users or individuals with considerable astigmatism. Neglecting to inform patients about these anticipated visual distortions frequently leads to the early cessation of prescribed adjustments.
Dry eye disease is a prevalent condition that can hinder visual function in individuals with presbyopia, particularly those who use contact lenses. Age-related meibomian gland dysfunction, diminished tear production, and heightened ocular surface inflammation are all aggravated by extended close work and digital screen usage—behaviors characteristic of this cohort. The use of contact lenses can exacerbate tear film instability, leading to symptoms such as foreign body sensation, intermittent blurriness, and burning. This issue is especially important with multifocal lenses, as even minor surface imperfections or dryness can significantly impair their function. Preventive measures include assessing the pre-fitting ocular surface, using lubricating drops, and switching to daily disposable or silicone hydrogel lenses with enhanced wettability.
Surgical correction methods for presbyopia, such as presbyLASIK, corneal inlays, and intraocular lens implantation, are also associated with potential complications. PresbyLASIK, which alters the cornea to create a multifocal optical profile, may lead to halos, glare, impaired night vision, and decreased contrast sensitivity. These consequences may be especially problematic in individuals with dilated pupils or abnormal corneal topography. Corneal inlays have been associated with epithelial thinning, stromal haze, and complications related to flaps; indeed, multiple inlays have been withdrawn from the market due to safety concerns and unsatisfactory long-term outcomes. Multifocal intraocular lenses enhance spectacle independence but may induce dysphotopsias, including starbursts and halos, especially in low-light circumstances. These occurrences may result in patient unhappiness, even when visual acuity measures are sufficient.
Emotional and functional challenges may arise when presbyopia is mismanaged or misunderstood. Patients often view the necessity for immediate repair as an indicator of age, thus leading to rejection or postponement of obtaining care. The psychological strain of adjusting to visual aids, such as bifocals or contact lenses, can diminish the quality of life. These difficulties may be exacerbated by occupational limitations, such as challenges in reading fine print, using computers, or performing manual tasks that require depth perception. Furthermore, the escalating intricacy of visual settings, especially due to the prevalence of digital devices, has heightened the necessity for tailored repairs. Neglecting to satisfy these evolving demands may result in unhappiness and nonadherence to prescribed treatments.
Deterrence and Patient Education
Considering the inevitability of presbyopia with aging, the focus of deterrence shifts from preventing onset to delaying functional impairment, improving adaptability, and mitigating the effects on quality of life. Patient education is fundamental to this technique, ensuring that patients comprehend the nature of the condition, recognize early signs, and are empowered to make informed decisions regarding treatment options. Early education can help normalize presbyopia as a physiological and manageable condition.
Healthcare practitioners must clarify that presbyopia is not a disease but an inevitable consequence of lens aging, and that prompt correction can restore functionality without compromising ocular health. Clinicians should consider mentioning presbyopia in patients starting from the early 40s, especially in those currently using visual correction, so that forthcoming changes can be anticipated rather than dreaded. In addition, healthcare practitioners must be vigilant in assessing patients during routine examinations for nuanced alterations in near-vision capabilities, especially in low-light conditions or during prolonged reading activities. Early recognition fosters preparedness rather than surprise, enabling smoother transitions to appropriate corrective strategies.
Patient education should cover all potential corrective options, explaining the benefits and limitations of each. Individuals unfamiliar with progressive addition lenses may benefit from a demonstration of the visual transitions across different zones. Individuals considering contact lenses should be informed about the probable trial-and-error process involved in fitting multifocal designs, and reasonable expectations for vision quality and adaptation duration should be conveyed. For surgical candidates, particularly those contemplating multifocal intraocular lenses or corneal refractive operations, comprehensive informed consent is essential. This process should include an examination of probable visual abnormalities, such as halos and glare; the durability of surgical outcomes; and the potential necessity for supplementary repairs postoperatively.
Patients can be reminded of minor lifestyle changes, such as using optimal illumination while reading, taking frequent breaks from close work, and adjusting the text size on digital devices to minimize strain. The widespread use of smartphones and computers has altered the visual requirements of contemporary living, rendering correction for intermediate and near vision increasingly essential. Recommendations on digital screen ergonomics, including maintaining an optimal viewing distance (40–70 cm) and a suitable screen height, help mitigate digital eye strain that may exacerbate presbyopic symptoms. For individuals with early or borderline presbyopia, these adjustments—coupled with low-add reading glasses—can provide short-term alleviation while reducing reliance on constant correction.
Pearls and Other Issues
Presbyopia is not simply a refractive alteration, but a lifestyle issue. The influence is intricately linked to visual work requirements, professional necessities, illumination settings, and patient expectations. Consequently, effective management frequently relies more on patient communication and behavioral counseling than on mere aesthetics. Presbyopia must be regarded as a chronic, progressive condition that needs continuous management rather than a singular prescription occurrence.
A frequently overlooked aspect of presbyopia management is the notion of pseudo-accommodation—functional near vision attained without genuine accommodative exertion.[118] This effect may arise from reduced pupil size, spherical aberration, or multifocal optics, often elucidating why specific individuals can execute close tasks despite very constrained objective accommodation. Identifying pseudo-accommodation is particularly crucial when advising patients who possess adequate near vision without correction, such as individuals with mild myopia or post-cataract patients with monofocal intraocular lenses. Promoting environmental techniques such as enhanced lighting, heightened contrast, and enlarged text can prolong functional near eyesight even without formal correction.
A significant drawback in presbyopia therapy is the inadequate or excessive correction of near addition, resulting in subpar vision and discontent. Excessive prescription of plus lenses may impair intermediate vision, whilst insufficient prescription may result in difficulties with small text. Accuracy in refraction, especially for near and intermediate working distances, is crucial. Clinicians must evaluate visual requirements and determine acceptable working distances to customize the near addition, rather than depend exclusively on age-related charts. Furthermore, as surgical alternatives become interesting alternatives, practitioners must be equipped to collaborate with ophthalmic surgeons and co-manage patients during refractive lens exchange or cataract surgeries, thereby ensuring continuity of care and facilitating informed patient decisions.
Enhancing Healthcare Team Outcomes
Effective management of presbyopia, particularly in contemporary visually intensive environments, necessitates collaborative, interdisciplinary care. Collaboration among optometrists, ophthalmologists, dispensing opticians, primary care physicians, nurses, and pharmacists is crucial for providing personalized, safe, and effective patient-centered care. Although presbyopia is not classified as a sickness in the conventional sense, its effects on functional vision, quality of life, and psychological well-being necessitate that healthcare teams address it with the same diligence and coordination as chronic disorders. Clinicians and optometrists play a pivotal role in diagnosing and managing presbyopia. Their duties encompass not only refraction but also counseling, managing concurrent ocular surface diseases, identifying symptoms that may indicate differential diagnosis, and arranging referrals for surgical evaluations.
By fostering open communication with ophthalmologists, particularly regarding multifocal intraocular lenses or laser vision correction, optometrists facilitate proper patient screening, education, and follow-up care. Furthermore, the timely identification of progression and the evaluation of changing visual requirements rely on consistent eye examinations and a longitudinal care strategy. Advanced practitioners, nurses, and ophthalmic technicians facilitate care by executing critical diagnostic and triage tasks, including assessing visual acuity at various distances; administering validated questionnaires, such as NAVQ and PICQ; and preparing patients for physician consultations. These healthcare professionals serve a crucial role in patient education, encompassing guidance on the use of spectacles and contact lenses, ocular hygiene, and postoperative care. Nurses and allied healthcare professionals frequently serve as the initial point of contact for patient issues, facilitating expectation management, alleviating discomfort, and ensuring compliance with prescribed treatments. Communication must be sympathetic and aligned with the messaging from the prescribing professionals. Dispensing opticians and contact lens specialists play a crucial role in fitting patients with appropriate devices, educating them on lens maintenance, and assisting them during the adaptation phase. Their active involvement in resolving prevalent issues, such as challenges with multifocal lenses or complaints about progressive addition lens distortion, can significantly impact patient satisfaction.
A culture that values each healthcare provider's competence cultivates collaboration, thereby improving patient safety, visual outcomes, and satisfaction. The inclusion of the patient as an active participant in the healthcare team is equally significant. Informed decision-making, customized education, and accessible communication enhance results and adherence. Enabling patients to express their visual priorities—such as reading, driving, or computer usage—allows the team to tailor interventions that correspond with their values and lifestyle. The healthcare team not only restores near eyesight but also preserves autonomy, productivity, and dignity throughout life.
Media
(Click Image to Enlarge)
References
Gualdi L, Gualdi F, Rusciano D, Ambrósio R Jr, Salomão MQ, Lopes B, Cappello V, Fintina T, Gualdi M. Ciliary Muscle Electrostimulation to Restore Accommodation in Patients With Early Presbyopia: Preliminary Results. Journal of refractive surgery (Thorofare, N.J. : 1995). 2017 Sep 1:33(9):578-583. doi: 10.3928/1081597X-20170621-05. Epub [PubMed PMID: 28880331]
Kassumeh S, Priglinger SG. [Age-related loss of accommodation - presbyopia]. MMW Fortschritte der Medizin. 2023 Sep:165(15):43-45. doi: 10.1007/s15006-023-2837-8. Epub [PubMed PMID: 37653317]
Zuo H, Cheng H, Lin M, Gao X, Xiang Y, Zhang T, Gao N, Du M, Chen Y, Zheng S, Huang R, Wan W, Hu K. The effect of aging on the ciliary muscle and its potential relationship with presbyopia: a literature review. PeerJ. 2024:12():e18437. doi: 10.7717/peerj.18437. Epub 2024 Dec 24 [PubMed PMID: 39735562]
Rich W, Reilly MA. A Review of Lens Biomechanical Contributions to Presbyopia. Current eye research. 2023 Feb:48(2):182-194. doi: 10.1080/02713683.2022.2088797. Epub 2022 Jun 17 [PubMed PMID: 35713207]
Lafosse E, Wolffsohn JS, Talens-Estarelles C, García-Lázaro S. Presbyopia and the aging eye: Existing refractive approaches and their potential impact on dry eye signs and symptoms. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2020 Apr:43(2):103-114. doi: 10.1016/j.clae.2019.08.005. Epub 2019 Aug 21 [PubMed PMID: 31445772]
Ayaki M, Hanyuda A, Negishi K. Presbyopia and associated factors specific to age groups. Clinical & experimental optometry. 2025 Feb 12:():1-6. doi: 10.1080/08164622.2025.2461737. Epub 2025 Feb 12 [PubMed PMID: 39938940]
Schiefer U, Kraus C, Baumbach P, Ungewiß J, Michels R. Refractive errors. Deutsches Arzteblatt international. 2016 Oct 14:113(41):693-702. doi: 10.3238/arztebl.2016.0693. Epub [PubMed PMID: 27839543]
Wolffsohn JS, Davies LN, Sheppard AL. New insights in presbyopia: impact of correction strategies. BMJ open ophthalmology. 2023 Jan:8(1):. doi: 10.1136/bmjophth-2022-001122. Epub [PubMed PMID: 37278419]
Cunha CC, Berezovsky A, Furtado JM, Ferraz NN, Fernandes AG, Muñoz S, Watanabe SS, Sacai PY, Cypel M, Mitsuhiro MH, Morales PH, Vasconcelos GC, Cohen MJ, Campos M, Cohen JM, Belfort R Jr, Salomão SR. Presbyopia and Ocular Conditions Causing Near Vision Impairment in Older Adults From the Brazilian Amazon Region. American journal of ophthalmology. 2018 Dec:196():72-81. doi: 10.1016/j.ajo.2018.08.012. Epub 2018 Aug 15 [PubMed PMID: 30118685]
Holden BA, Fricke TR, Ho SM, Wong R, Schlenther G, Cronjé S, Burnett A, Papas E, Naidoo KS, Frick KD. Global vision impairment due to uncorrected presbyopia. Archives of ophthalmology (Chicago, Ill. : 1960). 2008 Dec:126(12):1731-9. doi: 10.1001/archopht.126.12.1731. Epub [PubMed PMID: 19064856]
Ayoub SC, Ahmad M. Presbyopia: Clinical Update. Insight (American Society of Ophthalmic Registered Nurses). 2017 Spring:42(2):29-36 [PubMed PMID: 30074720]
Martin H, Stachs O, Guthoff R, Grabow N, Jünemann A. [Biomechanical investigations on accommodation of the eye]. Der Ophthalmologe : Zeitschrift der Deutschen Ophthalmologischen Gesellschaft. 2018 Aug:115(8):649-654. doi: 10.1007/s00347-018-0661-9. Epub [PubMed PMID: 29404678]
Schachar RA, Tello C, Cudmore DP, Liebmann JM, Black TD, Ritch R. In vivo increase of the human lens equatorial diameter during accommodation. The American journal of physiology. 1996 Sep:271(3 Pt 2):R670-6 [PubMed PMID: 8853390]
Coleman DJ. Unified model for accommodative mechanism. American journal of ophthalmology. 1970 Jun:69(6):1063-79 [PubMed PMID: 5423772]
Efron N, Morgan PB. Rethinking contact lens aftercare. Clinical & experimental optometry. 2017 Sep:100(5):411-431. doi: 10.1111/cxo.12588. Epub 2017 Sep 4 [PubMed PMID: 28871604]
Schachar RA, Schachar IH, Li X, Pu Y, Kumar S, Kamangar F, Hunter B, Pierscionek BK, Cosman PC, Wang K. Finite element analysis of the lens profile during accommodation. PloS one. 2025:20(3):e0317740. doi: 10.1371/journal.pone.0317740. Epub 2025 Mar 17 [PubMed PMID: 40096132]
Davies LN, Biswas S, Bullimore M, Cruickshank F, Estevez JJ, Khanal S, Kollbaum P, Marcotte-Collard R, Montani G, Plainis S, Richdale K, Simard P, Wolffsohn JS. BCLA CLEAR presbyopia: Mechanism and optics. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102185. doi: 10.1016/j.clae.2024.102185. Epub 2024 May 24 [PubMed PMID: 38796331]
Wolffsohn JS, Dhallu S, Aujla M, Laughton D, Tempany K, Powell D, Gifford K, Gifford P, Wan K, Cho P, Stahl U, Woods J. International multi-centre study of potential benefits of ultraviolet radiation protection using contact lenses. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2022 Dec:45(6):101593. doi: 10.1016/j.clae.2022.101593. Epub 2022 Apr 15 [PubMed PMID: 35431131]
Berdahl J, Bala C, Dhariwal M, Lemp-Hull J, Thakker D, Jawla S. Patient and Economic Burden of Presbyopia: A Systematic Literature Review. Clinical ophthalmology (Auckland, N.Z.). 2020:14():3439-3450. doi: 10.2147/OPTH.S269597. Epub 2020 Oct 22 [PubMed PMID: 33116396]
Level 1 (high-level) evidenceSrinivasan R, Paramasivan G, Sharma A, Surya J, Sharma T, Raman R. Prevalence, risk factors and association with glycemic levels of presbyopia in South Indian population. Indian journal of ophthalmology. 2021 Nov:69(11):3173-3177. doi: 10.4103/ijo.IJO_1407_21. Epub [PubMed PMID: 34708766]
GBD 2019 Blindness and Vision Impairment Collaborators, Vision Loss Expert Group of the Global Burden of Disease Study. Trends in prevalence of blindness and distance and near vision impairment over 30 years: an analysis for the Global Burden of Disease Study. The Lancet. Global health. 2021 Feb:9(2):e130-e143. doi: 10.1016/S2214-109X(20)30425-3. Epub 2020 Dec 1 [PubMed PMID: 33275950]
Doki Y, Nakazawa Y, Sukegawa M, Petrova RS, Ishida Y, Endo S, Nagai N, Yamamoto N, Funakoshi-Tago M, Donaldson PJ. Piezo1 channel causes lens sclerosis via transglutaminase 2 activation. Experimental eye research. 2023 Dec:237():109719. doi: 10.1016/j.exer.2023.109719. Epub 2023 Nov 10 [PubMed PMID: 37951336]
Markoulli M, Fricke TR, Arvind A, Frick KD, Hart KM, Joshi MR, Kandel H, Filipe Macedo A, Makrynioti D, Retallic N, Garcia-Porta N, Shrestha G, Wolffsohn JS. BCLA CLEAR Presbyopia: Epidemiology and impact. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102157. doi: 10.1016/j.clae.2024.102157. Epub 2024 Apr 9 [PubMed PMID: 38594155]
Vision Loss Expert Group of the Global Burden of Disease Study, GBD 2019 Blindness and Vision Impairment Collaborators. Global estimates on the number of people blind or visually impaired by Uncorrected Refractive Error: a meta-analysis from 2000 to 2020. Eye (London, England). 2024 Aug:38(11):2083-2101. doi: 10.1038/s41433-024-03106-0. Epub 2024 Jul 4 [PubMed PMID: 38965322]
Level 1 (high-level) evidenceFricke TR, Tahhan N, Resnikoff S, Papas E, Burnett A, Ho SM, Naduvilath T, Naidoo KS. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology. 2018 Oct:125(10):1492-1499. doi: 10.1016/j.ophtha.2018.04.013. Epub 2018 May 9 [PubMed PMID: 29753495]
Level 1 (high-level) evidenceCardona G, López S. Pupil diameter, working distance and illumination during habitual tasks. Implications for simultaneous vision contact lenses for presbyopia. Journal of optometry. 2016 Apr-Jun:9(2):78-84. doi: 10.1016/j.optom.2015.06.005. Epub 2015 Oct 9 [PubMed PMID: 26481439]
Wang C, Wang X, Jin L, Tang B, Zhu W, Zhang G, Chen T, McAneney H, Kassalow J, Congdon N. Influence of presbyopia on smartphone usage among Chinese adults: A population study. Clinical & experimental ophthalmology. 2019 Sep:47(7):909-917. doi: 10.1111/ceo.13559. Epub 2019 Jun 13 [PubMed PMID: 31090978]
Frick KD, Joy SM, Wilson DA, Naidoo KS, Holden BA. The Global Burden of Potential Productivity Loss from Uncorrected Presbyopia. Ophthalmology. 2015 Aug:122(8):1706-10 [PubMed PMID: 26190438]
Katz JA, Karpecki PM, Dorca A, Chiva-Razavi S, Floyd H, Barnes E, Wuttke M, Donnenfeld E. Presbyopia - A Review of Current Treatment Options and Emerging Therapies. Clinical ophthalmology (Auckland, N.Z.). 2021:15():2167-2178. doi: 10.2147/OPTH.S259011. Epub 2021 May 24 [PubMed PMID: 34079215]
Hickenbotham A, Roorda A, Steinmaus C, Glasser A. Meta-analysis of sex differences in presbyopia. Investigative ophthalmology & visual science. 2012 May 31:53(6):3215-20. doi: 10.1167/iovs.12-9791. Epub 2012 May 31 [PubMed PMID: 22531698]
Level 1 (high-level) evidenceNakazawa Y, Kuno Y, Shimada H, Nagai N, Hiramatsu N, Takeda S, Yamamoto N, Funakoshi-Tago M, Sasaki H. High ambient temperature may induce presbyopia via TRPV1 activation. Medical molecular morphology. 2024 Dec:57(4):268-276. doi: 10.1007/s00795-024-00391-2. Epub 2024 Jul 9 [PubMed PMID: 38980406]
Wu X, Chen X, Tian F, Yang M, Lu F, Deng R, Lin N. Nonlinear effects of humidex on risk for asthenopia among adults: a national cross-sectional survey in China. Frontiers in public health. 2025:13():1515672. doi: 10.3389/fpubh.2025.1515672. Epub 2025 Mar 13 [PubMed PMID: 40182528]
Level 2 (mid-level) evidenceKoduah C, Bunce C, Gilbert C. Presbyopia and Other Eye Conditions in Teachers in Ghana. International journal of environmental research and public health. 2019 Sep 3:16(17):. doi: 10.3390/ijerph16173209. Epub 2019 Sep 3 [PubMed PMID: 31484296]
Bastawrous A, Kassalow J, Watts E. Global uncorrected refractive error and presbyopia: the size of the problem. Community eye health. 2024:37(122):3-4 [PubMed PMID: 38827964]
Muhit M, Minto H, Parvin A, Jadoon MZ, Islam J, Yasmin S, Khandaker G. Prevalence of refractive error, presbyopia, and unmet need of spectacle coverage in a northern district of Bangladesh: Rapid Assessment of Refractive Error study. Ophthalmic epidemiology. 2018 Apr:25(2):126-132. doi: 10.1080/09286586.2017.1370119. Epub 2017 Oct 4 [PubMed PMID: 28976783]
Bastawrous A, Suni AV. Thirty Year Projected Magnitude (to 2050) of Near and Distance Vision Impairment and the Economic Impact if Existing Solutions are Implemented Globally. Ophthalmic epidemiology. 2020 Apr:27(2):115-120. doi: 10.1080/09286586.2019.1700532. Epub 2019 Dec 6 [PubMed PMID: 31810404]
Bright T, Kuper H, Macleod D, Musendo D, Irunga P, Yip JLY. Population need for primary eye care in Rwanda: A national survey. PloS one. 2018:13(5):e0193817. doi: 10.1371/journal.pone.0193817. Epub 2018 May 1 [PubMed PMID: 29715288]
Level 3 (low-level) evidenceGlasser A, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision research. 1998 Jan:38(2):209-29 [PubMed PMID: 9536350]
Heys KR, Cram SL, Truscott RJ. Massive increase in the stiffness of the human lens nucleus with age: the basis for presbyopia? Molecular vision. 2004 Dec 16:10():956-63 [PubMed PMID: 15616482]
Weeber HA, Eckert G, Pechhold W, van der Heijde RG. Stiffness gradient in the crystalline lens. Graefe's archive for clinical and experimental ophthalmology = Albrecht von Graefes Archiv fur klinische und experimentelle Ophthalmologie. 2007 Sep:245(9):1357-66 [PubMed PMID: 17285335]
Koretz JF, Cook CA, Kaufman PL. Aging of the human lens: changes in lens shape upon accommodation and with accommodative loss. Journal of the Optical Society of America. A, Optics, image science, and vision. 2002 Jan:19(1):144-51 [PubMed PMID: 11778717]
de la Hoz A, Martinez-Enriquez E, Marcos S. Estimation of Crystalline Lens Material Properties From Patient Accommodation Data and Finite Element Models. Investigative ophthalmology & visual science. 2023 Aug 1:64(11):31. doi: 10.1167/iovs.64.11.31. Epub [PubMed PMID: 37639248]
Alejandre-Alba N, Gutierrez-Contreras R, Dorronsoro C, Marcos S. Intraocular Photobonding to Enable Accommodating Intraocular Lens Function. Translational vision science & technology. 2018 Sep:7(5):27. doi: 10.1167/tvst.7.5.27. Epub 2018 Oct 11 [PubMed PMID: 30324000]
Naroo SA, Woods CA, Gil-Cazorla R, Ang RE, Collazos M, Eperjesi F, Guillon M, Hipsley A, Jackson MA, Price ER, Wolffsohn JS. BCLA CLEAR presbyopia: Management with scleral techniques, lens softening, pharmaceutical and nutritional therapies. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102191. doi: 10.1016/j.clae.2024.102191. Epub 2024 Jun 29 [PubMed PMID: 39098809]
Wolffsohn JS, Davies LN. Presbyopia: Effectiveness of correction strategies. Progress in retinal and eye research. 2019 Jan:68():124-143. doi: 10.1016/j.preteyeres.2018.09.004. Epub 2018 Sep 19 [PubMed PMID: 30244049]
Khadka NK, Timsina R, Mainali L. An AFM Approach Applied in a Study of α-Crystallin Membrane Association: New Insights into Lens Hardening and Presbyopia Development. Membranes. 2022 May 14:12(5):. doi: 10.3390/membranes12050522. Epub 2022 May 14 [PubMed PMID: 35629848]
Nandi SK, Nahomi RB, Rankenberg J, Glomb MA, Nagaraj RH. Glycation-mediated inter-protein cross-linking is promoted by chaperone-client complexes of α-crystallin: Implications for lens aging and presbyopia. The Journal of biological chemistry. 2020 Apr 24:295(17):5701-5716. doi: 10.1074/jbc.RA120.012604. Epub 2020 Mar 17 [PubMed PMID: 32184356]
Pescosolido N, Barbato A, Giannotti R, Komaiha C, Lenarduzzi F. Age-related changes in the kinetics of human lenses: prevention of the cataract. International journal of ophthalmology. 2016:9(10):1506-1517 [PubMed PMID: 27803872]
Nandi SK, Rankenberg J, Glomb MA, Nagaraj RH. Transient elevation of temperature promotes cross-linking of α-crystallin-client proteins through formation of advanced glycation endproducts: A potential role in presbyopia and cataracts. Biochemical and biophysical research communications. 2020 Dec 17:533(4):1352-1358. doi: 10.1016/j.bbrc.2020.10.018. Epub 2020 Oct 17 [PubMed PMID: 33081971]
Reindel W, Zhang L, Chinn J, Rah M. Evaluation of binocular function among pre- and early-presbyopes with asthenopia. Clinical optometry. 2018:10():1-8. doi: 10.2147/OPTO.S151294. Epub 2018 Jan 4 [PubMed PMID: 30214336]
Pierscionek BK. Age-related response of human lenses to stretching forces. Experimental eye research. 1995 Mar:60(3):325-32 [PubMed PMID: 7789412]
Ntonti P, Mitsi C, Chatzimichael E, Panagiotopoulou EK, Bakirtzis M, Konstantinidis A, Labiris G. A systematic review of reading tests. International journal of ophthalmology. 2023:16(1):121-127. doi: 10.18240/ijo.2023.01.18. Epub 2023 Jan 18 [PubMed PMID: 36659955]
Level 1 (high-level) evidenceCacho-Martínez P, Cantó-Cerdán M, Lara-Lacárcel F, García-Muñoz Á. Validation of the Symptom Questionnaire for Visual Dysfunctions (SQVD): A Questionnaire to Evaluate Symptoms of any Type of Visual Dysfunctions. Translational vision science & technology. 2022 Feb 1:11(2):7. doi: 10.1167/tvst.11.2.7. Epub [PubMed PMID: 35113128]
Level 1 (high-level) evidenceSharma G, Chiva-Razavi S, Viriato D, Naujoks C, Patalano F, Bentley S, Findley A, Johnson C, Arbuckle R, Wolffsohn J. Patient-reported outcome measures in presbyopia: a literature review. BMJ open ophthalmology. 2020:5(1):e000453. doi: 10.1136/bmjophth-2020-000453. Epub 2020 Jul 12 [PubMed PMID: 32685693]
Bentley S, Findley A, Chiva-Razavi S, Naujoks C, Patalano F, Johnson C, Arbuckle R, Wolffsohn JS. Evaluation of the content validity of patient-reported outcome (PRO) instruments developed for use with individuals with phakic presbyopia, including the Near Activity Visual Questionnaire-presbyopia (NAVQ-P) and the near vision correction independence (NVCI) instrument. Journal of patient-reported outcomes. 2021 Oct 23:5(1):109. doi: 10.1186/s41687-021-00379-x. Epub 2021 Oct 23 [PubMed PMID: 34689253]
Sims J, Sloesen B, Bentley S, Naujoks C, Arbuckle R, Chiva-Razavi S, Pascoe B, Stochl J, Findley A, O'Brien P, Wolffsohn JS. Psychometric evaluation of the near activity visual questionnaire presbyopia (NAVQ-P) and additional patient-reported outcome items. Journal of patient-reported outcomes. 2024 Apr 9:8(1):41. doi: 10.1186/s41687-024-00717-9. Epub 2024 Apr 9 [PubMed PMID: 38592339]
Ostadimoghaddam H, Hashemi H, Nabovati P, Yekta A, Khabazkhoob M. The distribution of near point of convergence and its association with age, gender and refractive error: a population-based study. Clinical & experimental optometry. 2017 May:100(3):255-259. doi: 10.1111/cxo.12471. Epub 2016 Sep 22 [PubMed PMID: 27652584]
Deepu S, Kujur ES, Horo S, Priyanka N, Selvin SST, Kuriakose T. Prescription of near addition and its relation to accommodative reserve in presbyopia - The dichotomy between theory and practice. Indian journal of ophthalmology. 2021 Jul:69(7):1702-1706. doi: 10.4103/ijo.IJO_3160_20. Epub [PubMed PMID: 34146010]
du Toit R. How to prescribe spectacles for presbyopia. Community eye health. 2006 Mar:19(57):12-3 [PubMed PMID: 17491738]
Schallhorn JM, Pantanelli SM, Lin CC, Al-Mohtaseb ZN, Steigleman WA 3rd, Santhiago MR, Olsen TW, Kim SJ, Waite AM, Rose-Nussbaumer JR. Multifocal and Accommodating Intraocular Lenses for the Treatment of Presbyopia: A Report by the American Academy of Ophthalmology. Ophthalmology. 2021 Oct:128(10):1469-1482. doi: 10.1016/j.ophtha.2021.03.013. Epub 2021 Mar 17 [PubMed PMID: 33741376]
Walline JJ, Robboy MW, Hilmantel G, Tarver ME, Afshari NA, Dhaliwal DK, Morse CL, Quinn CJ, Repka MX, Eydelman MB. Food and Drug Administration, American Academy of Ophthalmology, American Academy of Optometry, American Association for Pediatric Ophthalmology and Strabismus, American Optometric Association, American Society of Cataract and Refractive Surgery, and Contact Lens Association of Ophthalmologists Co-Sponsored Workshop: Controlling the Progression of Myopia: Contact Lenses and Future Medical Devices. Eye & contact lens. 2018 Jul:44(4):205-211. doi: 10.1097/ICL.0000000000000511. Epub [PubMed PMID: 29923881]
Morgan PB, Efron N, Papas E, Barnett M, Carnt N, Dutta D, Hepworth A, Little JA, Nagra M, Pult H, Schweizer H, Shen Lee B, Subbaraman LN, Sulley A, Thompson A, Webster A, Markoulli M. BCLA CLEAR Presbyopia: Management with contact lenses and spectacles. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102158. doi: 10.1016/j.clae.2024.102158. Epub 2024 Apr 16 [PubMed PMID: 38631935]
Asare FA, Ahiakwao GA, Oduro BA, Nti AN. Assessment of optical quality of ready-made reading spectacles for presbyopic correction. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2023 Nov:43(6):1337-1343. doi: 10.1111/opo.13197. Epub 2023 Jun 28 [PubMed PMID: 37376831]
Level 2 (mid-level) evidenceKrause K. [Acceptance of progressive lenses]. Klinische Monatsblatter fur Augenheilkunde. 1996 Aug-Sep:209(2-3):94-9 [PubMed PMID: 8992091]
Garcia-Porta N, Gómez-Varela AI, Arines-Piferrer J. Visual performance of new affordable and auto-adherent lenses for presbyopia correction. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2024 Jan:44(1):78-82. doi: 10.1111/opo.13241. Epub 2023 Oct 27 [PubMed PMID: 37888774]
Song S, Wen D, Yin Y, Qian F, Xu H, Xia X. Correction of presbyopia. Zhong nan da xue xue bao. Yi xue ban = Journal of Central South University. Medical sciences. 2022 Oct 28:47(10):1454-1460. doi: 10.11817/j.issn.1672-7347.2022.220201. Epub [PubMed PMID: 36411697]
Level 2 (mid-level) evidenceGupta N, Wolffsohn JS, Naroo SA. Comparison of near visual acuity and reading metrics in presbyopia correction. Journal of cataract and refractive surgery. 2009 Aug:35(8):1401-9. doi: 10.1016/j.jcrs.2009.03.026. Epub [PubMed PMID: 19631128]
Fogt JS, Weisenberger K, Fogt N. Visual performance with multifocal contact lenses and progressive addition spectacles. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2022 Aug:45(4):101472. doi: 10.1016/j.clae.2021.101472. Epub 2021 May 26 [PubMed PMID: 34049808]
Steele KR, Wagner H, Lai N, Zimmerman AB. Gas-Permeable Contact Lenses and Water Exposure: Practices and Perceptions. Optometry and vision science : official publication of the American Academy of Optometry. 2021 Mar 1:98(3):258-265. doi: 10.1097/OPX.0000000000001660. Epub [PubMed PMID: 33771955]
Tucker T, Early J. Pilocarpine 1.25% Ophthalmic Solution (Vuity) for the Treatment of Presbyopia. American family physician. 2023 Jun:107(6):659-660 [PubMed PMID: 37327177]
Mousavi SA, Rajavi Z, Sabbaghi H, Abdi S, Montazerin N, Kheiri B, Haseli-Mofrad A, Sheibani K, Jaldian HB. Pharmacological Treatment of Presbyopia Using Pilocarpine 1.25% Eye Drops. Journal of ophthalmic & vision research. 2024 Dec:19(4):468-475. doi: 10.18502/jovr.v19i4.14578. Epub 2024 Dec 31 [PubMed PMID: 39917455]
. Vuity - pilocarpine ophthalmic solution for presbyopia. The Medical letter on drugs and therapeutics. 2022 Feb 7:64(1643):17-18 [PubMed PMID: 35134046]
Level 3 (low-level) evidenceKorenfeld MS, Robertson SM, Stein JM, Evans DG, Rauchman SH, Sall KN, Venkataraman S, Chen BL, Wuttke M, Burns W. Topical lipoic acid choline ester eye drop for improvement of near visual acuity in subjects with presbyopia: a safety and preliminary efficacy trial. Eye (London, England). 2021 Dec:35(12):3292-3301. doi: 10.1038/s41433-020-01391-z. Epub 2021 Jan 29 [PubMed PMID: 33514891]
Grzybowski A, Ruamviboonsuk V. Pharmacological Treatment in Presbyopia. Journal of clinical medicine. 2022 Mar 3:11(5):. doi: 10.3390/jcm11051385. Epub 2022 Mar 3 [PubMed PMID: 35268476]
Orman B, Benozzi G. Pharmacological Treatments for Presbyopia. Drugs & aging. 2023 Feb:40(2):105-116. doi: 10.1007/s40266-022-01002-4. Epub 2023 Jan 20 [PubMed PMID: 36670320]
Grzybowski A, Markeviciute A, Zemaitiene R. A Review of Pharmacological Presbyopia Treatment. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.). 2020 May-Jun:9(3):226-233. doi: 10.1097/APO.0000000000000297. Epub [PubMed PMID: 32511122]
German EJ, Wood D, Hurst MA. Ocular effects of antimuscarinic compounds: is clinical effect determined by binding affinity for muscarinic receptors or melanin pigment? Journal of ocular pharmacology and therapeutics : the official journal of the Association for Ocular Pharmacology and Therapeutics. 1999 Jun:15(3):257-69 [PubMed PMID: 10385135]
Abdelkader A. Improved Presbyopic Vision With Miotics. Eye & contact lens. 2015 Sep:41(5):323-7. doi: 10.1097/ICL.0000000000000137. Epub [PubMed PMID: 25806674]
Abdelkader A, Kaufman HE. Clinical outcomes of combined versus separate carbachol and brimonidine drops in correcting presbyopia. Eye and vision (London, England). 2016:3():31 [PubMed PMID: 27981057]
Level 2 (mid-level) evidenceYe Y, Xian Y, Liu F, Zhang Z, Niu L, Shi W, Wang X, Zhou X, Zhao J. Comparison of monovision surgery using ICL V4c or femtosecond laser LASIK for myopia correction in the presbyopia age patients. Scientific reports. 2025 Mar 4:15(1):7629. doi: 10.1038/s41598-025-88588-y. Epub 2025 Mar 4 [PubMed PMID: 40038326]
Zhang R, Yuan Y, Zhang Y, Chen Y. Visual Quality Following Femtosecond Laser-Assisted In Situ Keratomileusis With Q-Value-Guided Optimized Monovision in Patients With Myopia and Presbyopia. American journal of ophthalmology. 2025 Mar:271():156-165. doi: 10.1016/j.ajo.2024.10.028. Epub 2024 Nov 6 [PubMed PMID: 39510369]
Level 2 (mid-level) evidenceCraig JP, Barsam A, Chen C, Chukwuemeka O Jr, Ghorbani-Mojarrad N, Kretz F, Michaud L, Moore J, Pelosini L, Turnbull AMJ, Vincent SJ, Wang MTM, Ziaei M, Wolffsohn JS. BCLA CLEAR Presbyopia: Management with corneal techniques. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102190. doi: 10.1016/j.clae.2024.102190. Epub 2024 Jun 8 [PubMed PMID: 38851946]
Bauerberg JM. Centered vs. inferior off-center ablation to correct hyperopia and presbyopia. Journal of refractive surgery (Thorofare, N.J. : 1995). 1999 Jan-Feb:15(1):66-9 [PubMed PMID: 9987728]
Koller T, Seiler T. Four corneal presbyopia corrections: simulations of optical consequences on retinal image quality. Journal of cataract and refractive surgery. 2006 Dec:32(12):2118-23 [PubMed PMID: 17137994]
Level 2 (mid-level) evidenceCharman WN. Developments in the correction of presbyopia II: surgical approaches. Ophthalmic & physiological optics : the journal of the British College of Ophthalmic Opticians (Optometrists). 2014 Jul:34(4):397-426. doi: 10.1111/opo.12129. Epub 2014 Apr 10 [PubMed PMID: 24716827]
Harb WG, Chamoun NG, Harb GW. KAMRA Inlay Implantation for Presbyopia Compensation: A Retrospective Evaluation of Patient Satisfaction and Subjective Vision 12-Month Postoperative. Middle East African journal of ophthalmology. 2019 Apr-Jun:26(2):65-70. doi: 10.4103/meajo.MEAJO_159_16. Epub 2019 Aug 26 [PubMed PMID: 31543662]
Level 2 (mid-level) evidenceSánchez-González MC, Gutiérrez-Sánchez E, Sánchez-González JM, De-Hita-Cantalejo C, Pinero-Rodríguez AM, González-Cruces T, Capote-Puente R. Complications of Small Aperture Intracorneal Inlays: A Literature Review. Life (Basel, Switzerland). 2023 Jan 22:13(2):. doi: 10.3390/life13020312. Epub 2023 Jan 22 [PubMed PMID: 36836669]
Moshirfar M, Lau CK, Chartrand NA, Parsons MT, Stapley S, Bundogji N, Ronquillo YC, Linn SH, Hoopes PC. Explantation of KAMRA Corneal Inlay: 10-Year Occurrence and Visual Outcome Analysis. Clinical ophthalmology (Auckland, N.Z.). 2022:16():3327-3337. doi: 10.2147/OPTH.S382544. Epub 2022 Oct 10 [PubMed PMID: 36237487]
Kasthurirangan S, Markwell EL, Atchison DA, Pope JM. MRI study of the changes in crystalline lens shape with accommodation and aging in humans. Journal of vision. 2011 Mar 25:11(3):. pii: 19. doi: 10.1167/11.3.19. Epub 2011 Mar 25 [PubMed PMID: 21441300]
Baïkoff G, Matach G, Fontaine A, Ferraz C, Spera C. Correction of presbyopia with refractive multifocal phakic intraocular lenses. Journal of cataract and refractive surgery. 2004 Jul:30(7):1454-60 [PubMed PMID: 15210222]
Ranno S, Rabbiolo GM, Lucentini S, Ruggiero E, Luccarelli SV, Lombardi L, Nucci P. Angle-supported intraocular lens versus scleral-sutured posterior chamber intraocular lens in post-cataract surgery aphakic patients: two-year follow-up cost-effectiveness analysis. International ophthalmology. 2022 Mar:42(3):871-879. doi: 10.1007/s10792-021-02068-6. Epub 2021 Nov 15 [PubMed PMID: 34779973]
Al-Dwairi R, Saleh O, Aleshawi A, Alladkanie Z, Al Deyabat O, Alasheh A, Adi S, Al-Howthi M. Anterior Versus Retropupillary Iris-Claw Intraocular Lens: Indications, Visual Outcome and Postoperative Complications. Ophthalmology and therapy. 2022 Apr:11(2):771-784. doi: 10.1007/s40123-022-00474-2. Epub 2022 Feb 11 [PubMed PMID: 35149965]
Drolsum L, Kristianslund O. Implantation of retropupillary iris-claw lenses: A review on surgical management and outcomes. Acta ophthalmologica. 2021 Dec:99(8):826-836. doi: 10.1111/aos.14824. Epub 2021 Mar 8 [PubMed PMID: 33683012]
Huber C. Planned myopic astigmatism as a substitute for accommodation in pseudophakia. Journal - American Intra-Ocular Implant Society. 1981 Summer:7(3):244-9 [PubMed PMID: 7287567]
Kelava L, Barić H, Bušić M, Čima I, Trkulja V. Monovision Versus Multifocality for Presbyopia: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Advances in therapy. 2017 Aug:34(8):1815-1839. doi: 10.1007/s12325-017-0579-7. Epub 2017 Jul 3 [PubMed PMID: 28674958]
Level 3 (low-level) evidencede Medeiros AL, de Araújo Rolim AG, Motta AFP, Ventura BV, Vilar C, Chaves MAPD, Carricondo PC, Hida WT. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clinical ophthalmology (Auckland, N.Z.). 2017:11():1911-1916. doi: 10.2147/OPTH.S145945. Epub 2017 Oct 26 [PubMed PMID: 29138533]
Kohnen T, Herzog M, Hemkeppler E, Schönbrunn S, De Lorenzo N, Petermann K, Böhm M. Visual Performance of a Quadrifocal (Trifocal) Intraocular Lens Following Removal of the Crystalline Lens. American journal of ophthalmology. 2017 Dec:184():52-62. doi: 10.1016/j.ajo.2017.09.016. Epub 2017 Sep 18 [PubMed PMID: 28923587]
Bellucci R, Curatolo MC. A New Extended Depth of Focus Intraocular Lens Based on Spherical Aberration. Journal of refractive surgery (Thorofare, N.J. : 1995). 2017 Jun 1:33(6):389-394. doi: 10.3928/1081597X-20170329-01. Epub [PubMed PMID: 28586499]
Moore JE, McNeely RN, Pazo EE, Moore TC. Rotationally asymmetric multifocal intraocular lenses: preoperative considerations and postoperative outcomes. Current opinion in ophthalmology. 2017 Jan:28(1):9-15 [PubMed PMID: 27828894]
Level 3 (low-level) evidenceOshika T, Nakano S, Inamura M, Ikai N, Kato Y, Izumi I, Shimokawabe K. Extensive misalignment of plate-haptic rotationally asymmetric multifocal toric intraocular lens. Japanese journal of ophthalmology. 2023 Sep:67(5):560-564. doi: 10.1007/s10384-023-01001-x. Epub 2023 Jun 8 [PubMed PMID: 37289297]
Enaholo ES, Musa MJ, Zeppieri M. Accommodative Insufficiency. StatPearls. 2025 Jan:(): [PubMed PMID: 36508537]
Hussaindeen JR, Murali A. Accommodative Insufficiency: Prevalence, Impact and Treatment Options. Clinical optometry. 2020:12():135-149. doi: 10.2147/OPTO.S224216. Epub 2020 Sep 11 [PubMed PMID: 32982529]
Gantz L, Stiebel-Kalish H. Convergence insufficiency: Review of clinical diagnostic signs. Journal of optometry. 2022 Oct-Dec:15(4):256-270. doi: 10.1016/j.optom.2021.11.002. Epub 2021 Dec 25 [PubMed PMID: 34963569]
Ozulken K, Ilhan C, Yuksel E, Mumcuoglu T. Preliminary effects of treating the half of high latent hyperopia on refractive and visual results of femtosecond laser-assisted in situ keratomileusis in subjects with hyperopia. International ophthalmology. 2020 Sep:40(9):2361-2369. doi: 10.1007/s10792-020-01421-5. Epub 2020 May 19 [PubMed PMID: 32430870]
Liu YC, Wilkins M, Kim T, Malyugin B, Mehta JS. Cataracts. Lancet (London, England). 2017 Aug 5:390(10094):600-612. doi: 10.1016/S0140-6736(17)30544-5. Epub 2017 Feb 25 [PubMed PMID: 28242111]
Ayaki M, Hanyuda A, Negishi K. Presbyopia, Dry Eye, and Retinal Thickness in the Middle-Aged Population: Focusing on Sex Differences. Clinical optometry. 2024:16():223-231. doi: 10.2147/OPTO.S481279. Epub 2024 Sep 2 [PubMed PMID: 39246672]
Seraji-Bzorgzad N, Paulson H, Heidebrink J. Neurologic examination in the elderly. Handbook of clinical neurology. 2019:167():73-88. doi: 10.1016/B978-0-12-804766-8.00005-4. Epub [PubMed PMID: 31753158]
Wolffsohn JS, Berkow D, Chan KY, Chaurasiya SK, Fadel D, Haddad M, Imane T, Jones L, Sheppard AL, Vianya-Estopa M, Walsh K, Woods J, Zeri F, Morgan PB. BCLA CLEAR Presbyopia: Evaluation and diagnosis. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102156. doi: 10.1016/j.clae.2024.102156. Epub 2024 Apr 18 [PubMed PMID: 38641525]
McDonald MB, Barnett M, Gaddie IB, Karpecki P, Mah F, Nichols KK, Trattler WB. Classification of Presbyopia by Severity. Ophthalmology and therapy. 2022 Feb:11(1):1-11. doi: 10.1007/s40123-021-00410-w. Epub 2021 Oct 28 [PubMed PMID: 34709607]
Wolffsohn JS, Naroo SA, Bullimore MA, Craig JP, Davies LN, Markoulli M, Schnider C, Morgan PB. BCLA CLEAR Presbyopia: Definitions. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2024 Aug:47(4):102155. doi: 10.1016/j.clae.2024.102155. Epub 2024 Apr 11 [PubMed PMID: 38609792]
Shafer BM, Puls-Boever K, Berdahl JP, Thompson V, Ibach MJ, Zimprich LL, Schweitzer JA. Defocus Curve of Emerging Presbyopic Patients. Clinical ophthalmology (Auckland, N.Z.). 2023:17():843-847. doi: 10.2147/OPTH.S400194. Epub 2023 Mar 13 [PubMed PMID: 36937167]
Ren Y, Li J, Jiang X, Khadka J, Wang Y, Gu C, Wu Y, Wang Q, Huang J, Gao R. Psychometric assessment of the Chinese version of the Near Activity Visual Questionnaire in presbyopia using Rasch analysis. Journal of cataract and refractive surgery. 2025 Apr 17:():. doi: 10.1097/j.jcrs.0000000000001675. Epub 2025 Apr 17 [PubMed PMID: 40241405]
Johnson N, Shirneshan E, Coon CD, Stokes J, Wells T, Lundy JJ, Andrae DA, Evans CJ, Campbell J. Development of the Presbyopia Impact and Coping Questionnaire. Ophthalmology and therapy. 2021 Dec:10(4):1057-1075. doi: 10.1007/s40123-021-00391-w. Epub 2021 Oct 13 [PubMed PMID: 34643894]
Zeri F, Naroo S. Finding routes towards understanding and the successful correction of presbyopia. Contact lens & anterior eye : the journal of the British Contact Lens Association. 2016 Dec:39(6):401. doi: 10.1016/j.clae.2016.11.001. Epub [PubMed PMID: 27863717]
Level 3 (low-level) evidenceBilbao-Calabuig R, Gónzalez-López F, Llovet-Rausell A, Ortega-Usobiaga J, Tejerina Fernández V, Llovet-Osuna F. Lens-based surgical correction of presbyopia. Where are we in 2020? Archivos de la Sociedad Espanola de Oftalmologia. 2021 Feb:96(2):74-88. doi: 10.1016/j.oftal.2020.07.012. Epub 2020 Aug 28 [PubMed PMID: 32868085]
Bamdad S, Ahmad Razavizadegan S, Farvardin M, Mohaghegh S. Vision-related Quality of Life after Bilateral Implantation of Monofocal and Multifocal Intraocular Lenses. Journal of ophthalmic & vision research. 2022 Jan-Mar:17(1):19-26. doi: 10.18502/jovr.v17i1.10166. Epub 2022 Jan 21 [PubMed PMID: 35194492]
Level 2 (mid-level) evidenceMencucci R, Favuzza E, Ribeiro F. Editorial: Addressing the unmet needs of cataract patients: when quality of vision can make the difference in quality of life. Frontiers in medicine. 2023:10():1232243. doi: 10.3389/fmed.2023.1232243. Epub 2023 Jun 29 [PubMed PMID: 37457565]
Level 2 (mid-level) evidenceDhallu SK, Sheppard AL, Drew T, Mihashi T, Zapata-Díaz JF, Radhakrishnan H, Iskander DR, Wolffsohn JS. Factors Influencing Pseudo-Accommodation-The Difference between Subjectively Reported Range of Clear Focus and Objectively Measured Accommodation Range. Vision (Basel, Switzerland). 2019 Jun 28:3(3):. doi: 10.3390/vision3030034. Epub 2019 Jun 28 [PubMed PMID: 31735835]