Introduction
The median nerve, known as the "eye of the hand," plays a crucial role in hand function. This nerve supplies the flexor-pronator muscles of the forearm and most muscles in the radial portion of the hand, controlling thumb abduction, wrist flexion, and flexion of the finger phalanges. Sensory innervation covers the palmar surface of the thumb, index, middle, and radial half of the ring finger, and the entire palmar region of the radial hand. Additionally, the median nerve supplies sensation to the dorsal skin of the distal phalanges of the index and middle fingers.
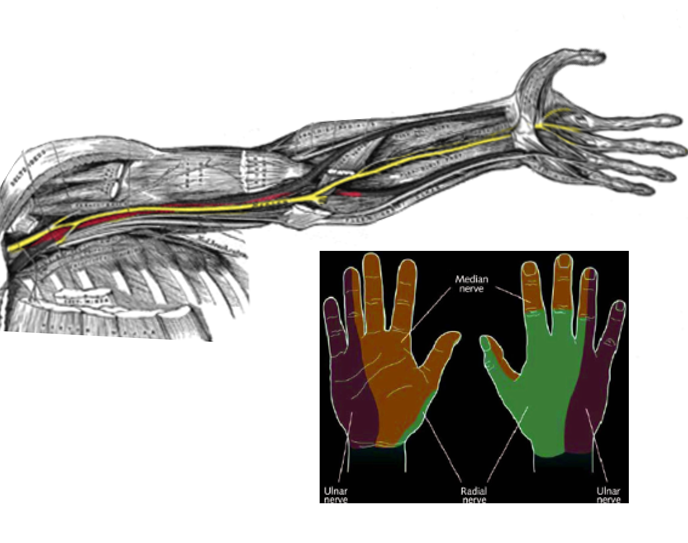
Originating in the cervical spinal cord, the median nerve forms from the medial and lateral cords of the brachial plexus, which derive from the ventral primary rami of cervical roots C5 to C8 and the first thoracic segment. The nerve descends medial to the brachial artery at the humerus level, passing between the 2 heads of the pronator teres muscle in the forearm (see Image. Nerve Distribution in the Arm and Hand). The nerve lies superficially in the cubital fossa, beneath the bicipital aponeurosis, then courses deep to the flexor digitorum superficialis and superficial to the flexor digitorum profundus. Entering the palm beneath the flexor retinaculum, the nerve passes lateral to the flexor digitorum superficialis tendon and posterior to the palmaris longus tendon. Injury or pathology may occur at any point along this course.
Of note, the median nerve does not supply any muscles in the arm. A branch to the pronator teres arises proximal to the elbow joint. Several vascular branches of the median nerve supply the brachial artery, and articular branches provide innervation to the elbow joint. In the forearm, the median nerve innervates the pronator teres, flexor digitorum superficialis, palmaris longus, and flexor carpi radialis. The nerve also supplies the lateral half of the flexor digitorum profundus and the pronator quadratus via its anterior interosseous branch (see Image. Course of the Median Nerve in the Forearm). Additionally, the anterior interosseous nerve supplies the flexor pollicis longus.
Articular branches from the median nerve supply the carpal joints and the distal radioulnar and radiocarpal joints. Multiple communicating branches connect the median nerve with the ulnar nerve in the forearm and hand. In the hand, the median nerve innervates the thenar muscles, including the abductor pollicis brevis, opponens pollicis, and the superficial head of the flexor pollicis brevis. The palmar cutaneous branch of the median nerve provides sensation to the skin over the thenar eminence. The median nerve supplies sensation to the palmar surface of the lateral two and a half digits—the thumb, index finger, middle finger, and the radial half of the ring finger—and the dorsal distal phalanges of these same digits.
The median nerve may be affected by acute traumatic, chronic microtraumatic, and compressive lesions. Damage may also result from multiple-cause degenerative processes and neuropathies. These different lesion types can involve various levels along the nerve’s long course from the brachial plexus and axilla to the hand. Neuropathies primarily affect the distal territory.
Compression frequently occurs beneath the fascial sheath of the flexor retinaculum, leading to burning pain, numbness, and tingling—symptoms characteristic of neuropathic pain. This condition, entrapment or carpal tunnel syndrome, produces a needle-and-pin sensation along the median nerve distribution. Carpal tunnel syndrome often arises idiopathically but has associations with hypothyroidism, pregnancy, and diabetes.
Decreased sensation over the thenar eminence indicates a median nerve injury proximal to the carpal tunnel. The palmar cutaneous branch, which supplies this area, originates proximal to the carpal tunnel. Clinically, symptoms may present intermittently, with periods of flares and remissions.
A strong clinical history often suggests median nerve pathology, but several diagnostic modalities can aid confirmation. Plain radiographs, including dedicated carpal tunnel views, assist in identifying underlying causes. Ultrasound use is increasingly becoming a valuable tool in diagnosing nerve abnormalities.
Median nerve mononeuropathy most commonly occurs at the carpal tunnel. However, entrapment at other sites accounts for approximately 7% to 10% of cases.[1] These sites include the ligament of Struthers, lacertus fibrosus, between the heads of the pronator teres, and near the flexor digitorum superficialis. Electromyography is key in confirming the diagnosis and precisely localizing the lesion.
Treatment varies according to the entrapment site. Initial management typically involves noninvasive measures such as braces to relieve compression, physical therapy, and lifestyle modifications to reduce repetitive stress. Surgical intervention may be considered if conservative therapies prove ineffective.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Median nerve injuries arise from multiple mechanisms and may occur at various sites along its course in the upper limb. Common causes include anterior shoulder dislocation, elbow dislocation, humerus fractures, midshaft radius fractures, stab wounds, prolonged tourniquet application, and repeated use of crutches. These injuries rarely occur in isolation and often coexist with radial or ulnar nerve neuropathies. The most common mechanisms of injury are as follows:
- Direct trauma to the wrist and elbow joints
- Accidental trauma in the axilla, wrist, and palm during surgical procedures
- Self-inflicted wrist lacerations as part of attempted self-harm
- Humerus fractures, especially supracondylar fractures
- Entrapment at the elbow between the 2 heads of the pronator teres (pronator teres syndrome) and under the flexor retinaculum (carpal tunnel syndrome)
- Involvement in generalized degenerative and demyelinating disorders
- Chemotherapy-induced peripheral neuropathy [2]
- Carpal tunnel injection involving the median nerve at the wrist (Source: Attia, 2021)
- Neurotoxic agents causing neuropathy, where compression neuropathy may precede generalized peripheral neuropathy [3]
- Thoracic outlet syndrome [4]
Although most cases of carpal tunnel syndrome are idiopathic, various conditions can induce or precipitate nerve entrapment at the elbow, contributing to its clinical presentation. Pregnancy-induced carpal tunnel syndrome, for example, is partly caused by fluid retention. Secondary causes include space-occupying lesions such as tumors, fractured callus, osteophytes, and hypertrophic synovial tissue.
Metabolic conditions, including hypothyroidism, pregnancy, and rheumatoid arthritis, also contribute. Infection, alcohol use disorder, and familial disorders represent additional risk factors. Connective tissue diseases further increase susceptibility to carpal tunnel syndrome. Established risk factors include repetitive wrist extension and flexion, obesity, and recent menopause.[5] Increased pressure within the carpal tunnel results in nerve compression and damage.[6] Repetitive motion and exposure to vibratory tools elevate the risk of developing carpal tunnel syndrome.[7]
Epidemiology
Median nerve injuries are the primary cause of emergency department visits for peripheral nerve injuries. Approximately 8,000,000 cases are reported annually in the United States.[8] Carpal tunnel syndrome is the most common entrapment neuropathy of the upper extremity, affecting up to 3% of the general population.
The incidence of carpal tunnel syndrome stands at 105 cases per 100,000 person-years. Sex differences are notable. The syndrome occurs in 52 per 100,000 men and 149 per 100,000 women. Prevalence rates show that 1% of men and 7% of women are affected, resulting in an overall general population prevalence of 3%. Peak incidence occurs between ages 45 and 54. Bilateral carpal tunnel syndrome develops in up to 65% of cases.[9] Among older adults aged 65 to 74, women are 4 times more likely to develop carpal tunnel syndrome than men.
Carpal tunnel entrapment of the median nerve represents the most common nerve mononeuropathy. However, 7% to 10% of median nerve entrapments occur more proximally along the nerve. The supracondylar process, a bone spur on the medial distal humerus, accounts for approximately 0.5% of median nerve entrapments. Other entrapment sites include the lacertus fibrosus near the pronator teres muscle and the flexor digitorum superficialis muscle. Symptoms mimicking median nerve entrapment may also arise from conditions such as Martin-Gruber anastomosis. Electromyogram plays a crucial role in distinguishing and localizing nerve damage.
Carpal tunnel syndrome is common during pregnancy, affecting up to 62% of women. Hormonal changes, particularly increased relaxin levels, contribute to symptom development. In most cases, symptoms resolve postpartum as hormone levels normalize and fluid retention decreases.[10] Dexamethasone is widely considered the safest steroid for injection in these cases.
Pathophysiology
Median nerve involvement in a supracondylar fracture results in loss of pronation at both the proximal and distal radioulnar joints. The forearm becomes fixed in supination due to paralysis of the pronator teres and quadratus muscles. Wrist flexion is not primarily affected by the flexor digitorum superficialis or flexor digitorum profundus. Rather, wrist flexion weakness results mainly from paralysis of the flexor carpi radialis.
Weakness of the flexor carpi radialis impairs wrist flexion and may cause radial deviation during wrist flexion because the ulnar-sided wrist flexors act unopposed. Flexion loss at the proximal interphalangeal joints of the index and middle fingers results from paralysis of the flexor digitorum superficialis. In contrast, loss of flexion at the distal interphalangeal joints results from paralysis of the lateral half of the flexor digitorum profundus. Flexion loss at the terminal phalanx of the thumb is caused by paralysis of the flexor pollicis longus. Paralysis of the thenar muscles, particularly the opponens pollicis, leads to wasting the thenar eminence (see Image. Signs of Untreated Carpal Tunnel Syndrome). The thumb typically becomes adducted and rotated, producing the characteristic “ape hand” deformity, which is marked by loss of thumb opposition and abduction, with the thumb aligned along the palm.
In median nerve injuries at the midforearm, relative extension of the index finger may occur due to paralysis of the flexor digitorum superficialis and the lateral half of the flexor digitorum profundus supplying this finger. Sensory loss typically affects the palmar surface of the lateral three and a half digits—the thumb, index finger, middle finger, and radial half of the ring finger—and the dorsal distal phalanges of these same digits. Sensation over the thenar eminence is usually spared in distal lesions due to the early branching of the palmar cutaneous nerve. The affected skin area may feel warm and dry because of sympathetic denervation. Chronic vasomotor changes in longstanding cases can lead to atrophy of the finger pulp.
Toxicokinetics
Although not specific to median neuropathy, toxic neuropathies continue to cause considerable morbidity worldwide. The list of causative agents, particularly medications, continues to grow, and no definitive breakthrough treatments have emerged. Management is focused on prevention and symptom control. Many toxins may be responsible, including alcohol, industrial chemicals, biotoxins, and pharmaceuticals. Toxic neuropathy may initially present as localized entrapment neuropathies, such as carpal tunnel syndrome or lateral femoral cutaneous nerve involvement, before progressing to a generalized pattern.
Several pharmacologic and environmental agents are known to induce toxic neuropathies. Among chemotherapeutic agents, cisplatin, oxaliplatin, and taxanes are frequently implicated. Antiretroviral drugs such as zalcitabine and didanosine can also produce neuropathy. Tumor necrosis factor α inhibitors, including infliximab (Remicade), etanercept (Enbrel), adalimumab (Humira), certolizumab pegol (Cimzia), and golimumab (Simponi), have also been associated with peripheral nerve injury.
Exposure to organic solvents such as n-hexane, often through recreational glue sniffing, and trichloroethylene, a contaminant in some groundwater, can result in neuropathy. Other neurotoxic agents include organophosphates, diphtheria toxin (Corynebacterium diphtheriae), trimethyltin, dimethylaminopropionitrile, and thallium. Substances such as heroin or its contaminants (eg, bleach, pesticides), especially when injected, may produce direct neurotoxic effects or injury related to intravenous drug use.[11] Heavy metals, particularly lead, mercury, cadmium, and arsenic, are significant contributors to toxic neuropathy.
History and Physical
The impact of trauma on the median nerve varies by injury site and may involve the palm, forearm, arm, or axilla. Damage to the nerve results in motor, sensory, and vasomotor deficits. Most injuries affect the nerve at the wrist. While carpal tunnel syndrome remains the most recognized manifestation, several traumatic lesions can impair the nerve along its course, from the wrist to the axilla and up to the brachial plexus.
Wrist Lesions
Median nerve trauma at the wrist occurs most frequently, particularly in association with wrist fractures. Injuries range from compression by fracture fragments to contusions and, less commonly, complete or partial nerve transections. The median nerve remains highly vulnerable at the wrist due to its superficial location, making it susceptible to lacerations and penetrating trauma. Damage to the palmar sensory branch or iatrogenic injury during wrist surgery may result in painful amputation neuromas.
Carpal Tunnel Syndrome
Anatomically, the carpal tunnel consists of the flexor retinaculum superiorly and the carpal bones inferiorly. Within this tunnel lie the median nerve and 9 flexor tendons. Symptoms may localize to the wrist or affect the entire hand, often radiating into the forearm. Typical signs and symptoms of carpal tunnel syndrome include thenar weakness, numbness in the radial three and a half fingers, and paresthesias. Burning pain along the distribution of the median nerve also occurs. These symptoms can resemble those caused by injury to the C6 and C7 nerve roots.
Carpal tunnel syndrome is an isolated injury to the distal median nerve. In contrast to radiculopathy, this condition does not cause triceps weakness or impaired wrist extension. Symptoms often worsen at night and may awaken patients from sleep. Carpal tunnel syndrome may be distinguished clinically using Tinel and Phalen tests. Thenar atrophy suggests chronic median nerve injury. Tenderness or swelling in the cubital fossa may indicate proximal nerve involvement, often accompanied by weakness in forearm pronation and active wrist flexion. A positive Tinel sign supports the diagnosis of carpal tunnel syndrome; a positive Phalen maneuver further reinforces the diagnosis.[12] Descriptions of these tests appear below.
The "flick sign" refers to a patient's instinctive need to flick the hands to relieve symptoms after waking from sleep due to carpal tunnel syndrome. This test demonstrates 93% sensitivity and 96% specificity for the condition.[13] The hand elevation test offers diagnostic utility comparable to the Phalen maneuver and the Tinel sign. In this test, the patient raises their hand above their head for a minute. Reproduction of symptoms suggests carpal tunnel syndrome.[14]
Several specialized physical examination tests assist in confirming the diagnosis. The Phalen maneuver involves wrist flexion to 90° with elbows fully extended. Symptom reproduction within 60 seconds constitutes a positive result. The Tinel sign is positive when rapid, repeated tapping over the volar aspect of the wrist elicits symptoms along the median nerve distribution. The median nerve compression test involves applying direct pressure over the transverse carpal ligament. Reproduction of symptoms within 30 seconds is considered a positive result.
The severity index of carpal tunnel syndrome is categorized as mild, moderate, or severe. Mild carpal tunnel syndrome causes numbness and tingling in the median nerve distribution without motor or sensory deficits. Sleep remains undisturbed, and activities of daily living are not affected. Moderate carpal tunnel syndrome includes symptoms of the mild form, accompanied by sensory loss in the median nerve distribution and disrupted sleep. Some decline in hand function may also occur. Severe carpal tunnel syndrome presents with symptoms of both mild and moderate cases, as well as weakness in the median nerve distribution and limitations in activities of daily living.
Pronator Syndrome
Pronator syndrome, also known as pronator teres syndrome, arises from compression of the median nerve by the pronator teres muscle. The clinical presentation can closely resemble carpal tunnel syndrome. Patients often report forearm discomfort during activity. Symptoms are frequently reproduced by maintaining an extended elbow and engaging in repetitive pronation, which provokes numbness and tingling in the thumb and first 2 digits.
Sensation over the forearm and fingers is generally preserved in pronator syndrome. However, loss of sensation over the thenar eminence frequently occurs, offering a clinical distinction from carpal tunnel syndrome. The Phalen maneuver and Tinel sign are typically negative. In pronator teres syndrome, the median nerve becomes entrapped as it passes through the pronator teres. This syndrome is commonly observed in professional cyclists. Sensory loss is most often observed over the lateral palm and, as noted, the thenar eminence.
Anterior Interosseous Neuropathy
Anterior interosseous neuropathy is a distinct form of median nerve injury. The anterior interosseous branch originates from the median nerve at the elbow and courses into the anterior forearm. This nerve supplies the flexor pollicis longus, pronator quadratus, and the deep flexors of digits 2 and 3. As the anterior interosseous nerve has no cutaneous branch, the neuropathy presents solely with motor deficits and no sensory loss.
On physical examination, patients cannot approximate the thumb and index finger. This deficit results in difficulty pinching objects and an inability to form an "OK" sign with the thumb and index finger. Most injuries to the anterior interosseous nerve occur in the context of complex trauma. Isolated injuries are uncommon.
Elbow Lesions
Median nerve involvement at the elbow can occur during fracture-dislocations, either directly from bone fragments in high-impact trauma that tear the nerve or indirectly through acute compression by perineural hematomas or nerve stretching. Additionally, reparative fibrous processes can entrap and constrict the nerve during healing. The median nerve can become interposed between fracture fragments or articular surfaces during attempts at reduction or alignment, resulting in entrapment.
Compressive lesions may also arise at the fibrous arch of the flexor digitorum superficialis or the pronator teres muscle. Compression at the fibrous arch often causes painful neuropathic symptoms accompanied by muscle weakness. Median nerve injury can also occur as a complication of elbow surgical procedures, including arthroscopy, corrective surgeries, prosthetic implantation, and fracture management. Iatrogenic damage remains a recognized cause of elbow-level median neuropathy.
Arm, Axillary, or Upper Lesions
Traumatic injuries of the arm, including humerus fractures, can result in median nerve paralysis. However, deep penetrating trauma more commonly causes acute damage. Stab wounds, gunshot wounds, high-energy forces, such as in road traffic accidents, and complex brachial plexus injuries can lead to nerve lesions at the axilla or upper arm. Damage at these levels results in paralysis of all muscles innervated by the median nerve, accompanied by sensory impairment.
High median nerve injuries encompass lesions occurring proximal to the origin of the anterior interosseous nerve.[15] These injuries lead to substantial disability of the affected limb and compromise the ability to perform even basic activities of daily living. The degree of dysfunction varies due to overlapping innervation and muscular compensation. Tendon and nerve transfers are commonly employed in management.[16] However, functional outcomes often fall short of expectations.
Evaluation
The Tinel and Phalen tests commonly diagnose carpal tunnel syndrome, but their accuracy varies. Study results report sensitivities ranging from 50% to 91% and specificities between 33% and 88%.[17] The Tinel sign involves lightly tapping over a nerve to elicit a tingling or "pins and needles" sensation along its distribution. A positive Tinel sign suggests potential nerve irritation or compression. However, this test has limitations. Any nerve can produce a tingling sensation if tapped with enough force, and the sensitivity for carpal tunnel syndrome is only around 50%.[18] Electromyography and nerve conduction studies (NCS), collectively known as electrodiagnostic evaluation, represent the gold standard for diagnosing median neuropathies like carpal tunnel syndrome.
Manual motor testing of the abductor pollicis brevis may be performed with the patient seated, palms facing upward, and facing the examiner. The patient is asked to press the pad of the thumb (digit 1) against the pinky (digit 5) while the examiner attempts to force the base of the thumb toward the radial side. Observation should also be made for atrophy of the abductor pollicis brevis or thinning and smoothness of the skin over the muscle, which are common clinical findings.
NCS can detect impaired median nerve conduction across the carpal tunnel while showing normal conduction along the remainder of its path. Electromyography helps determine pathology within the muscles innervated by the median nerve and is especially useful for excluding polyneuropathy or radiculopathy. NCS can demonstrate up to 99% specificity for carpal tunnel syndrome, although results may remain normal in patients with mild symptoms.[19][20]
Carpal tunnel syndrome may be classified based on nerve conduction velocity into 4 categories. Mild cases show prolonged sensory latencies with a slight decrease in conduction velocity and no signs of axonal degeneration. Moderate cases exhibit abnormal sensory conduction velocities alongside reduced motor conduction velocities, still without axonal degeneration. Severe cases present with absent sensory responses and prolonged motor latencies, indicating reduced motor conduction velocities. Extreme cases involve the absence of both sensory and motor responses.
A cross-sectional area of 9 mm² or more on musculoskeletal ultrasound demonstrates 87% sensitivity for carpal tunnel syndrome.[21] Magnetic resonance imaging (MRI) and x-ray are typically not indicated for suspected carpal tunnel syndrome. However, MRI may be considered when median nerve entrapment at the wrist is suspected and the patient does not recover along the expected course. This imaging modality can help identify synovial hypertrophy or space-occupying lesions such as ganglion cysts.
Significant differences exist in the median nerve's shear modulus and cross-sectional area in patients with carpal tunnel syndrome. Specifically, carpal tunnel syndrome is characterized by greater nerve stiffness on the symptomatic side compared to the asymptomatic side at various angular positions of the radiocarpal joint. Median nerve stiffness increases with greater degrees of flexion and extension of the radiocarpal joint in both symptomatic and asymptomatic limbs.[22]
Treatment / Management
Management of median nerve injury depends on the cause. Splinting is considered a first-line treatment for mild to moderate carpal tunnel syndrome. Study results show this method to be more effective than a placebo, but no single splint has proven superior. However, results from a study demonstrated that a neutral wrist splint provided twice the symptomatic relief compared to an extension splint.[23][24] When night splints are started and symptoms persist after a month, splinting should be continued for 1 to 2 months while another conservative treatment is added to the care plan. Splints may be worn at night or continuously, though continuous use offers no advantage over nighttime use.[25][26](A1)
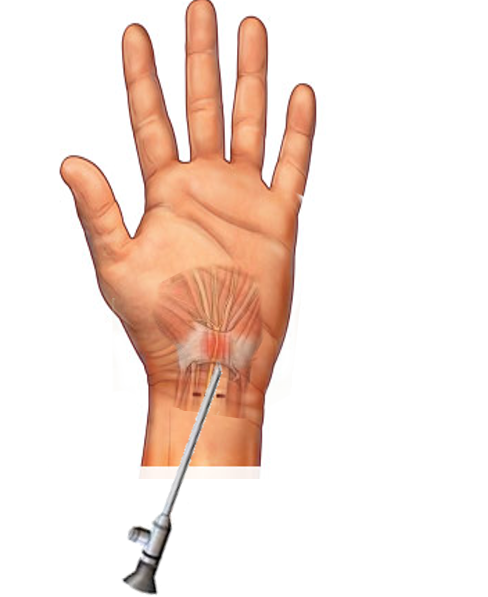
Other conservative treatments include physical therapy, yoga, and therapeutic ultrasound. Corticosteroid injections combined with night splints are the first-line conservative approach for mild to moderate carpal tunnel syndrome.[27][28] Combined therapies are recommended as they are more effective than any single modality alone.[29] Local corticosteroid injections have been shown to delay the need for surgery at 1 year postinjection (see Image. Injection Treatment for Carpal Tunnel Syndrome). Risks include possible injection into the median nerve and tendon rupture. Ultrasound guidance is recommended for carpal tunnel injections to minimize risks and improve accuracy. When comparing 80 mg to 40 mg of methylprednisolone for corticosteroid injections, both doses reduced the likelihood of surgery at 12 months compared to placebo.[30](A1)
Evidence does not support one technique over another. However, ultrasound-guided injections demonstrate greater effectiveness than blind techniques.[31] A repeat corticosteroid injection may be offered 6 months after the initial injection. Surgery is recommended if symptoms recur following the second injection. Oral prednisone at a dose of 20 mg for 10 to 14 days improves pain related to carpal tunnel syndrome and hand function compared to placebo up to 8 weeks after treatment.[32] Physical therapy, therapeutic ultrasound, and carpal bone mobilization show limited effectiveness. However, a randomized trial found yoga to improve patient symptoms compared to wrist splints for up to 8 weeks.[33] Success rates of nonsurgical options vary from 20% to 93%, depending on symptom severity.[34](A1)
Patients with severe carpal tunnel symptoms who fail conservative management after 4 to 6 months should be offered surgical decompression. Electrodiagnostic studies are recommended before surgery to assess underlying severity and prognosis in patients opting for surgical decompression after unsuccessful conservative treatment. Consensus indicates that carpal tunnel release surgery offers more benefit than no treatment and demonstrates improved clinical outcomes compared to wrist splints. Both endoscopic and open carpal tunnel release surgeries improve patient symptoms. When comparing open and endoscopic decompression, patients return to work a week earlier with endoscopic surgery. New evidence supports ultrasound-guided carpal tunnel releases.
Mild compression of the median nerve tends to worsen over 10 to 15 months, whereas moderate or severe involvement often improves. Treatment of carpal tunnel syndrome with splinting or surgical decompression results in complete or marked improvement in 70% to 90% of patients at 1 year following therapy.[35][36] Management of pronator teres syndrome includes limiting activities that provoke symptoms. Nonsteroidal anti-inflammatory drugs, local corticosteroid injections into tender points of the pronator teres, and median nerve decompression surgery have demonstrated effectiveness.(A1)
All peripheral nerve injuries, including those affecting the median nerve, present therapeutic challenges due to heterogeneous etiology and pathoanatomy, necessitating a tailored approach to maximize functional recovery. Autografts remain the gold standard for nerve reconstruction, offering superior biocompatibility and support for axonal regeneration. However, autografts involve donor site morbidity, limited availability, and possible mismatches in nerve diameter and structure. To overcome these limitations, significant advancements have been made in nerve conduits, allografts, and regenerative medicine. Engineered nerve conduits, including synthetic and biological scaffolds, offer alternatives to autografts by guiding axonal growth across nerve gaps while reducing risks associated with donor nerve harvesting.[37](B3)
Differential Diagnosis
The differential diagnosis includes cervical radiculopathy, motor neuron diseases, fibromyalgia, compartment syndrome, pain from simple overuse, myofascial syndrome, which are usually time-limited and resolve with rest, and brachial plexopathy. The various clinical conditions to consider may be grouped as follows:
- Dislocation of the interphalangeal joints or the carpometacarpal joint of the thumb
- Peripheral demyelinating diseases, such as acute disseminated inflammatory polyradiculopathy and chronic inflammatory demyelinating polyneuropathy
- Central demyelinating disorders
- Infection of the underlying palmar spaces
- Local muscular injuries around the thumb
- Rheumatoid arthritis causing arthritic changes in the wrist that compromise the carpal tunnel
- Tenosynovitis involving the tendons of the opponens pollicis and flexor pollicis longus
- Malingering
- Somatization
Careful clinical evaluation is essential to differentiate these conditions from median nerve pathology. Accurate diagnosis ensures appropriate management and avoids unnecessary interventions.
Treatment Planning
Treatment planning focuses on the underlying diagnosis, the location of median nerve compression, and the cause of that compression. Almost all clinicians have managed or encountered cases of carpal tunnel syndrome, even if they have not personally experienced it. Carpal tunnel release surgery is the most common procedure performed. Surgical practices vary regarding the use of bracing, sutures, staples, or dissolvable plastic closures, as well as the timing for removal of staples or sutures. Prophylactic antibiotics are rarely administered. Surgical decompression at the wrist tends to be straightforward, whereas decompression at the elbow or other sites may be more complex. Immobilization in a cast, half-cast, or sling may or may not be necessary after elbow surgery. Preferences for wound care and postoperative management differ widely among surgeons.
Principles of rehabilitation medicine should be applied to maintain joint range of motion, preserve muscle tone, and exercise innervated muscles as much as possible without exceeding postoperative restrictions. Many patients have overlapping myofascial syndrome and may or may not meet the diagnostic criteria for fibromyalgia. These conditions should be managed concurrently. Postoperative care involving immobilization with a sling may trigger flares of myofascial pain. Heat, massage, ice, therapeutic ultrasound, and osteopathic manipulation may be beneficial, particularly targeting the cervicothoracic junction, lower cervical spine segments, or other dysfunctional areas.
Certain professions predispose individuals to carpal tunnel syndrome. In patients undergoing second or third decompressions, vocational rehabilitation and adaptive tools, such as voice recognition software or artificial intelligence, can help reduce repetitive upper extremity motions, especially when performing tasks like editing multiple articles. When secondary arthritis is present, injections may be directed to the carpal tunnel, wrist joint, basal joint, or thumb extensor mechanism, depending on the clinical situation.
The mechanics of the hand are complex and interconnected. Many patients also develop metacarpophalangeal arthritis, basal joint pain, first compartment syndrome (de Quervain syndrome), tennis elbow (epicondylitis), or other overuse syndromes involving the medial or lateral epicondyles. Sensory symptoms may persist even years after surgical decompression, often requiring ongoing use of wrist braces or night splints. Secondary muscular or skeletal symptoms, such as medial elbow pain, should be managed according to severity, location, and individual patient factors.
Pregnancy presents a unique consideration, as fluid retention and other factors often contribute to clinically significant carpal tunnel syndrome. The operating surgeon typically obtains clearance from the obstetrician, and many procedures are performed under local anesthesia alone. Some clinicians prefer to inject the carpal tunnel and reassess the need for surgical decompression after delivery. Management strategies differ widely, and the approach to carpal tunnel syndrome in pregnancy remains a topic of ongoing debate. Postoperative pain following a simple carpal tunnel release is generally managed with over-the-counter medications such as acetaminophen and nonsteroidal anti-inflammatories.
Patients with chronic pain may also require special consideration. Individuals on long-term pain management regimens, including opioids, serotonin reuptake inhibitors, membrane stabilizers, or tricyclic antidepressants, may experience flares that necessitate additional analgesia. In these cases, the surgeon may collaborate with the patient’s pain management clinician to coordinate postoperative care, typically involving a short-term increase in their existing medications. The primary challenge in this population often lies in tapering them back to their baseline dosing following recovery.
Toxicity and Adverse Effect Management
Toxicologic considerations in managing median nerve pathology largely reflect those associated with generalized peripheral neuropathy, as no toxic agent selectively targets the median nerve. These concerns arise primarily from pharmacologic interventions rather than the underlying nerve condition. Corticosteroid injections into the carpal tunnel, typically using a depot preparation, carry known systemic risks, including hyperglycemia and fluid retention, similar to other steroid formulations administered orally or parenterally. Local anesthetic toxicity also presents a potential hazard, particularly with agents such as bupivacaine (Marcaine), although the doses used for carpal tunnel injections rarely reach toxic thresholds. Inadvertent intravascular injection, however, remains a known risk.[38]
While not an isolated median nerve injury, reflex sympathetic dystrophy, also known as complex regional pain syndrome type I, can follow trauma to the median nerve. In such cases, interventional treatments, including stellate ganglion blocks, thoracic sympathetic blocks, or Bier blocks, pose significant procedural risks. These potential complications include pneumothorax, hematoma formation, and phrenic nerve blockade leading to respiratory compromise. The most frequently encountered complication is systemic local anesthetic toxicity, which primarily affects cardiac conduction and can be managed with intravenous lipid emulsion therapy or "lipid rescue."[39] (Source: Caroll et al, 2023)
Safe administration of these interventions requires appropriate facility readiness. At minimum, the procedure setting should include 2 clinicians trained in basic and advanced cardiac life support, 2 additional staff members with basic life support certification, and access to a fully stocked emergency resuscitation cart. Ideally, personnel should also hold advanced trauma life support certification, particularly in settings where thoracic decompression or surgical airway management may become necessary.
Pregnant individuals require individualized care due to physiologic changes that often contribute to the development of carpal tunnel syndrome. Decompression of the median nerve under local anesthesia poses minimal risk during pregnancy. Lidocaine, commonly used in these procedures, is generally regarded as safe for topical and systemic use in pregnant individuals. Although lidocaine crosses the placental barrier, current data show no association with increased miscarriage, congenital anomalies, or adverse neonatal outcomes when used within recommended dosing limits. (Source: Mother to Baby Ask the Experts, 2023)
The timing of decompression during pregnancy remains controversial. Some clinicians advocate for conservative management until after delivery, anticipating spontaneous resolution postpartum. Others recommend early surgical intervention for symptom relief and functional preservation. Strong opinions persist on both sides of this debate.
Removal of the offending substance is essential in cases of exposure to neurotoxic agents during pregnancy. Blood levels may be obtained for agents such as lead, and medication regimens should be reviewed and modified where feasible. However, certain exposures, whether environmental, occupational, or therapeutic, cannot always be avoided. For example, chemotherapeutic neurotoxins may be the only viable treatment, and their continued use must be weighed against the neurological risk to both patient and fetus.
Prognosis
The prognosis of median nerve injuries depends on the site of entrapment or damage and the interval between injury and repair. Minor lacerations treated with immediate surgical intervention and appropriate supportive care tend to yield the most favorable outcomes and minimize long-term deformities. The Sunderland classification system defines peripheral nerve injuries across 5 grades, based on the extent of structural disruption and the corresponding potential for regeneration. These injuries range from neurapraxia, characterized by a transient conduction block without structural damage and typically resolving within weeks (commonly referred to as “Saturday night palsy”), to neurotmesis, a complete transection of the nerve including the epineurium, which necessitates surgical repair.
Neurotmesis often results from penetrating trauma and carries additional surgical implications. For example, a knife wound to the median nerve proximal to the elbow may also involve the brachial artery or surrounding tendons, requiring complex vascular and orthopedic repair. Diagnosis may be delayed until after intensive care unit stabilization, and recovery efforts such as occupational therapy or nerve regeneration treatments may be complicated by broader trauma and postoperative constraints.
Median Neuropathy at the Wrist
An acute carpal tunnel syndrome can follow a single event, such as extensive yard work in 1 day or a rear-impact motor vehicle collision while gripping the steering wheel. This carpal tunnel syndrome often resolves if the precipitating activity is avoided. Similarly, prognosis in pregnancy tends to be favorable once the pregnancy concludes.
Prognosis improves in younger patients. Meanwhile, a bilateral positive Phalen test on physical examination correlates with worse outcomes. Conservative therapies typically lead to symptom improvement within 2 to 6 weeks, with maximal benefit observed by 3 months. Another conservative modality should be pursued if symptoms persist after 6 weeks of initial treatment with one approach.[40]
Several predictors are linked to the failure of nonsurgical treatment.[41] These factors include symptom duration exceeding 6 months, continuous paresthesias, patient aged 50 and older, impaired 2-point discrimination, a Phalen test becoming positive in under 30 seconds, and prolonged motor and sensory latency on electromyogram. Surgical decompression yields a successful outcome in approximately 70% to 90% of cases. Most patients report marked improvement by the end of the first postoperative week and can return to normal activities within 2 weeks. However, complete recovery may require up to 1 year in some cases.[42]
Complications
Due to reduced myelination, sensory fibers sustain damage from nerve compression more readily than motor fibers. Therefore, paresthesias, numbness, and tingling typically appear as the earliest signs of carpal tunnel syndrome. Motor fibers become involved as the condition worsens. A known variant of carpal tunnel syndrome affects only motor fibers, with normal sensory studies but prolonged motor latency. Patients with this presentation often exhibit weakness in thumb abduction and opposition. Fine motor skills deteriorate, resulting in difficulty with tasks such as dressing or opening jars. As sensory fibers degenerate, pain tends to diminish. As motor fibers deteriorate, muscular atrophy ensues. Two-point discrimination may also be lost at distances of 6 mm or more.[43][44]
Postoperative pain commonly occurs after surgical decompression, often manifesting lateral to the site of release. Failure of surgical decompression is frequently attributed to fibrosis or incomplete division of the flexor retinaculum.[45] Surgical revision becomes necessary in such cases. Some surgeons also address scar tissue surrounding the median nerve as well as intraneural fibrosis.
Complications associated with carpal tunnel release surgery include the following:
- Incomplete division of the transverse carpal ligament
- Injury to the recurrent motor branch or palmar cutaneous branch of the median nerve
- Vascular injury involving the superficial palmar arch [46]
- Laceration of the median or ulnar nerve trunk
- Postoperative wound infection
- Painful scar formation
- Complex regional pain syndrome [47]
Surgical complications can limit functional recovery and require additional intervention. Risk awareness and technical precision are critical for optimal results.
Postoperative and Rehabilitation Care
Postoperative care varies based on the procedure performed and the surgeon’s preferences. Most patients are placed in a brace and soft dressing for 10 to 14 days. Closure may involve sutures or staples requiring removal, or a running intradermal suture placed by a plastic surgeon, which can be extracted in one motion. Dissolvable intradermal sutures are another option, often preferred when travel for suture removal is burdensome or transportation is limited.
Occupational therapy plays a key role in rehabilitation after carpal tunnel release or any median nerve injury. Therapy focuses on restoring hand and wrist function, reducing pain, and facilitating return to daily activities. Early surgical decompression in mild cases may not require additional intervention. However, delayed cases with advanced motor loss or hand arthritis often benefit from targeted therapy. Joint contractures frequently develop when decompression is postponed or nerve transection results in poor motor recovery, further highlighting the need for occupational therapy.
Two common modalities used in therapy are fluidotherapy and paraffin baths. Fluidotherapy is a physical therapy technique that uses a dry, heated whirlpool of solid particles suspended in air. This method delivers heat to soft tissues while providing tactile stimulation, which helps improve joint mobility, reduce stiffness, and manage pain, especially in the upper extremities. Paraffin bath therapy involves applying heated paraffin wax to the skin, primarily targeting the hands and fingers but also adaptable for the shoulders and elbows. This form of heat therapy alleviates pain, enhances mobility, and increases circulation, making it beneficial for conditions such as arthritis, burn scars, and joint stiffness.
Consultations
Carpal tunnel decompression is most commonly performed by orthopedic surgeons, who may or may not have fellowship training in upper extremity surgery, and also by plastic surgeons. Occupational therapy is frequently consulted for both postoperative care and coexisting conditions such as basal joint osteoarthritis or epicondylitis. Prosthetics and orthotics may also be involved. While physical or occupational therapists often fit patients with basic wrist cockup splints, more complex devices, such as dynamic splints or wrist flexor spring-assist orthoses, may require formal consultation with a certified prosthetist.
Although the initial complaint is typically hand pain, further evaluation may reveal abnormal laboratory findings, particularly in cases involving both hand and wrist pain rather than isolated tingling in the first 3 digits. Elevated acute phase reactants such as erythrocyte sedimentation rate and C-reactive protein, or disease-specific markers like anti-cyclic citrullinated peptide, antinuclear antibodies, and rheumatoid factor, may indicate an underlying systemic condition and warrant rheumatology consultation.
Median nerve injuries in pediatric populations are rare, and this activity will not discuss pediatric rehabilitation in detail. However, therapy in this population is typically structured through play-based approaches, which may include music therapy, physical therapy, occupational therapy, animal-assisted therapy, or any creative modality that facilitates participation. Depending on the institution, each of these interventions may require separate consults.
Deterrence and Patient Education
Patients should be informed that median nerve injury most often results from poor posture, workplace ergonomics, direct trauma, or physiological factors such as pregnancy. Diagnosis is primarily clinical, based on history and physical examination, with electrodiagnostic studies, electromyography, and NCS serving as the gold standard to confirm and localize the lesion. Symptoms typically worsen at night or in the early morning and may be temporarily relieved by the flick sign, a classic indicator of median nerve entrapment.[48] Physical examination findings, such as a positive Phalen or Tinel sign, further support the diagnosis. Imaging modalities like x-ray and ultrasound may aid in evaluation.
Initial treatment is conservative and includes ergonomic modification, wrist bracing, and physiotherapy. Steroid injections are often effective as a first-line intervention.[49] While pregnancy-related carpal tunnel syndrome usually resolves postpartum, persistent or refractory cases may require surgical decompression via transverse carpal ligament release.[50]
Pearls and Other Issues
Important information that clinicians should remember when evaluating and managing median nerve injury includes the following:
- Median neuropathy at the wrist (carpal tunnel syndrome) is both the most common entrapment of the median nerve and the most prevalent peripheral nerve entrapment overall. Risk factors include female sex, repetitive motion, a square-shaped carpal tunnel, and diabetes, which increases the risk for all common peripheral nerve entrapments.
- Electrodiagnostic testing by electromyography and NCS is the gold standard for diagnosing peripheral nerve pathology.
- Motor testing of the abductor pollicis brevis may be performed with the patient seated, palms up, facing the examiner. The patient is instructed to press the pad of the thumb (digit 1) to the pinky (digit 5), and the examiner applies resistance by attempting to push the base of the thumb radially. This maneuver isolates the abductor pollicis brevis, a median-nerve-innervated muscle, and allows for assessment of motor function distal to the carpal tunnel. Atrophy or thinning of the thenar eminence, particularly over this muscle, should be noted.
- A common pitfall is using the strength of the thumb-pinky pad grip as a proxy for median nerve motor function. While any observed weakness should be documented, this maneuver primarily tests the flexor pollicis longus and flexor digitorum profundus, which are innervated proximally by the median nerve above the carpal tunnel and the ulnar nerve above the Guyon canal. Therefore, this approach does not assess the motor function of median-innervated muscles below the carpal tunnel. Proper carpal tunnel syndrome motor testing should isolate the abductor pollicis brevis, not the long flexors of digits 1 and 5.
Median nerve evaluation requires precise clinical techniques to distinguish between proximal and distal involvement. Awareness of testing limitations improves both diagnostic precision and treatment outcomes.
Enhancing Healthcare Team Outcomes
Median nerve injury, along with the resulting pain, paresthesias, and upper extremity weakness, requires timely intervention, which may range from the use of night splints to surgical decompression. The underlying cause can vary widely, including idiopathic origins, direct trauma, repetitive strain, early manifestations of diabetes mellitus (whether insulin-dependent or maturity-onset), toxic exposures, central demyelinating disorders, and one of the many neurological “great masqueraders.” A thorough history and physical examination can usually identify nerve impairment without imaging studies.
Consultation with an interprofessional team of specialists is essential. While any advanced clinician may diagnose median nerve entrapment, primary care clinicians most commonly identify the condition. Several subspecialists, including physiatrists, neurologists, sports medicine physicians, orthopedists, hand surgeons, and radiologists, also encounter and manage this condition.
Conservative management typically serves as the first-line approach, especially in acute presentations. Physical and occupational therapists play a critical role during the healing process, contributing to both conservative care and postoperative rehabilitation following median nerve decompression. When clinical evidence is limited or inconclusive, expert input from specialists may guide decisions regarding imaging or treatment. If steroid injections are attempted as an alternative to surgery, pharmacists can support dosing and drug preparation. Their expertise also proves essential in managing persistent neuropathic pain, reinforcing their role within the care team.
The prognosis of median nerve injury depends on the underlying cause, the severity of the lesion, and the timeliness of the intervention. Early identification of complications leads to improved outcomes. Coordination among interprofessional team members is essential for optimal care. Shared decision-making, clear communication, and collaboration significantly influence the prognosis.
At a minimum, effective management should involve the following team members:
- A clinician with expertise in neurological examination, often a neurologist, physiatrist (physical medicine and rehabilitation), or neurosurgeon. However, any clinician capable of performing a comprehensive neurological exam may fulfill this role.
- An electrophysiologist, typically a neurologist or physiatrist, who conducts electrodiagnostic studies such as electromyography and NCS. Serial electrodiagnostic evaluations may be necessary to monitor progress.
- A surgeon for carpal tunnel syndrome, as this specialist may be a plastic or orthopedic surgeon. Some general surgeons, particularly in rural or underserved areas, may also perform carpal tunnel releases proficiently. While neurosurgeons can manage such procedures, their practice often focuses on the brain and spine.
Orthopedic surgeons with fellowship training in hand surgery generally perform more complex interventions, such as decompression of the posterior interosseous nerve. Notably, “hand surgery fellowship” typically refers to advanced training in procedures involving the shoulder, elbow, and wrist, not solely the hand. High median nerve injuries, including those proximal to the posterior interosseous nerve, may require complex nerve transfers. These treatments are often performed only at quaternary care centers by a limited number of highly specialized surgeons. Consequently, patients may need to travel long distances for evaluation and treatment. Humanitarian organizations like Angel Flight may assist in arranging travel for such medically necessary care.
Nurses are vital in coordinating postoperative care, including communication with the therapy team and monitoring patient progress. Physical and occupational therapists focus on restoring function, minimizing impairment, and reducing long-term disability. These professionals may also introduce adaptive equipment, such as button hooks, sock aids, or long-handled tools, to help patients maintain independence during recovery. Certified prosthetists and orthotists may also be consulted, particularly when more advanced orthotic solutions are needed beyond standard wrist cock-up splints. For example, a dynamic finger extension splint, such as one worn by the author in medical school, may support patients with persistent motor deficits.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Meyer P, Lintingre PF, Pesquer L, Poussange N, Silvestre A, Dallaudière B. The Median Nerve at the Carpal Tunnel … and Elsewhere. Journal of the Belgian Society of Radiology. 2018 Jan 31:102(1):17. doi: 10.5334/jbsr.1354. Epub 2018 Jan 31 [PubMed PMID: 30039031]
Cascella M. Chemotherapy-induced peripheral neuropathy: limitations in current prophylactic strategies and directions for future research. Current medical research and opinion. 2017 Jun:33(6):981-984. doi: 10.1080/03007995.2017.1284051. Epub 2017 Feb 15 [PubMed PMID: 28097895]
Level 3 (low-level) evidencePeters J, Staff NP. Update on Toxic Neuropathies. Current treatment options in neurology. 2022 May:24(5):203-216. doi: 10.1007/s11940-022-00716-5. Epub 2022 Apr 6 [PubMed PMID: 36186669]
Capodosal G, Holden D, Maloy W, Schroeder JD. Thoracic Outlet Syndrome. Current sports medicine reports. 2024 Sep 1:23(9):303-309. doi: 10.1249/JSR.0000000000001192. Epub 2024 Sep 1 [PubMed PMID: 39248399]
Ashworth NL. Carpal tunnel syndrome. BMJ clinical evidence. 2011 Oct 21:2011():. pii: 1114. Epub 2011 Oct 21 [PubMed PMID: 22018420]
Level 1 (high-level) evidenceTsai P, Steinberg DR. Median and radial nerve compression about the elbow. The Journal of bone and joint surgery. American volume. 2008 Feb:90(2):420-8 [PubMed PMID: 18254203]
Kozak A, Schedlbauer G, Wirth T, Euler U, Westermann C, Nienhaus A. Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: an overview of systematic reviews and a meta-analysis of current research. BMC musculoskeletal disorders. 2015 Sep 1:16():231. doi: 10.1186/s12891-015-0685-0. Epub 2015 Sep 1 [PubMed PMID: 26323649]
Level 3 (low-level) evidenceLad SP, Nathan JK, Schubert RD, Boakye M. Trends in median, ulnar, radial, and brachioplexus nerve injuries in the United States. Neurosurgery. 2010 May:66(5):953-60 [PubMed PMID: 20414978]
Bland JD, Rudolfer SM. Clinical surveillance of carpal tunnel syndrome in two areas of the United Kingdom, 1991-2001. Journal of neurology, neurosurgery, and psychiatry. 2003 Dec:74(12):1674-9 [PubMed PMID: 14638888]
Khosrawi S, Maghrouri R. The prevalence and severity of carpal tunnel syndrome during pregnancy. Advanced biomedical research. 2012:1():43. doi: 10.4103/2277-9175.100143. Epub 2012 Aug 28 [PubMed PMID: 23326774]
Bergström MA, Andersson ME, Larsson SB. Detection of drugs and hepatitis C virus in used syringes from a needle exchange in Gothenburg, Sweden. Drug testing and analysis. 2024 Sep:16(9):948-956. doi: 10.1002/dta.3614. Epub 2023 Dec 3 [PubMed PMID: 38044807]
Sevy JO, Sina RE, Varacallo MA. Carpal Tunnel Syndrome. StatPearls. 2025 Jan:(): [PubMed PMID: 28846321]
Harris-Adamson C, Eisen EA, Kapellusch J, Garg A, Hegmann KT, Thiese MS, Dale AM, Evanoff B, Burt S, Bao S, Silverstein B, Merlino L, Gerr F, Rempel D. Biomechanical risk factors for carpal tunnel syndrome: a pooled study of 2474 workers. Occupational and environmental medicine. 2015 Jan:72(1):33-41. doi: 10.1136/oemed-2014-102378. Epub 2014 Oct 16 [PubMed PMID: 25324489]
Ahn DS. Hand elevation: a new test for carpal tunnel syndrome. Annals of plastic surgery. 2001 Feb:46(2):120-4 [PubMed PMID: 11216604]
Isaacs J, Ugwu-Oju O. High Median Nerve Injuries. Hand clinics. 2016 Aug:32(3):339-48. doi: 10.1016/j.hcl.2016.03.004. Epub 2016 May 2 [PubMed PMID: 27387077]
Medina A. Use of Nerve Transfer Procedures for Motor and Sensory Restoration of a High Median Nerve Injury. Cureus. 2022 Jun:14(6):e26205. doi: 10.7759/cureus.26205. Epub 2022 Jun 22 [PubMed PMID: 35891829]
Zhang D, Chruscielski CM, Blazar P, Earp BE. Accuracy of Provocative Tests for Carpal Tunnel Syndrome. Journal of hand surgery global online. 2020 May:2(3):121-125. doi: 10.1016/j.jhsg.2020.03.002. Epub 2020 Apr 21 [PubMed PMID: 35415497]
Sharrak S,M Das J, Hand Nerve Compression Syndromes StatPearls. 2021 Jan [PubMed PMID: 31613463]
American Association of Electrodiagnostic Medicine, American Academy of Neurology, and American Academy of Physical Medicine and Rehabilitation. Practice parameter for electrodiagnostic studies in carpal tunnel syndrome: summary statement. Muscle & nerve. 2002 Jun:25(6):918-22 [PubMed PMID: 12115985]
Level 1 (high-level) evidenceWitt JC, Hentz JG, Stevens JC. Carpal tunnel syndrome with normal nerve conduction studies. Muscle & nerve. 2004 Apr:29(4):515-22 [PubMed PMID: 15052616]
Torres-Costoso A, Martínez-Vizcaíno V, Álvarez-Bueno C, Ferri-Morales A, Cavero-Redondo I. Accuracy of Ultrasonography for the Diagnosis of Carpal Tunnel Syndrome: A Systematic Review and Meta-Analysis. Archives of physical medicine and rehabilitation. 2018 Apr:99(4):758-765.e10. doi: 10.1016/j.apmr.2017.08.489. Epub 2017 Sep 22 [PubMed PMID: 28947163]
Level 1 (high-level) evidenceWolny T, Glibov K, Wieczorek M, Gnat R, Linek P. Changes in Ultrasound Parameters of the Median Nerve at Different Positions of the Radiocarpal Joint in Patients with Carpal Tunnel Syndrome. Sensors (Basel, Switzerland). 2024 Jul 11:24(14):. doi: 10.3390/s24144487. Epub 2024 Jul 11 [PubMed PMID: 39065886]
Page MJ, Massy-Westropp N, O'Connor D, Pitt V. Splinting for carpal tunnel syndrome. The Cochrane database of systematic reviews. 2012 Jul 11:2012(7):CD010003. doi: 10.1002/14651858.CD010003. Epub 2012 Jul 11 [PubMed PMID: 22786532]
Level 1 (high-level) evidenceBurke DT, Burke MM, Stewart GW, Cambré A. Splinting for carpal tunnel syndrome: in search of the optimal angle. Archives of physical medicine and rehabilitation. 1994 Nov:75(11):1241-4 [PubMed PMID: 7979936]
Level 1 (high-level) evidenceMuller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermid JC. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2004 Apr-Jun:17(2):210-28 [PubMed PMID: 15162107]
Level 1 (high-level) evidenceWalker WC, Metzler M, Cifu DX, Swartz Z. Neutral wrist splinting in carpal tunnel syndrome: a comparison of night-only versus full-time wear instructions. Archives of physical medicine and rehabilitation. 2000 Apr:81(4):424-9 [PubMed PMID: 10768530]
Level 1 (high-level) evidenceMcClure P. Evidence-based practice: an example related to the use of splinting in a patient with carpal tunnel syndrome. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2003 Jul-Sep:16(3):256-63 [PubMed PMID: 12943130]
Akalin E, El O, Peker O, Senocak O, Tamci S, Gülbahar S, Cakmur R, Oncel S. Treatment of carpal tunnel syndrome with nerve and tendon gliding exercises. American journal of physical medicine & rehabilitation. 2002 Feb:81(2):108-13 [PubMed PMID: 11807347]
Level 1 (high-level) evidenceRozmaryn LM, Dovelle S, Rothman ER, Gorman K, Olvey KM, Bartko JJ. Nerve and tendon gliding exercises and the conservative management of carpal tunnel syndrome. Journal of hand therapy : official journal of the American Society of Hand Therapists. 1998 Jul-Sep:11(3):171-9 [PubMed PMID: 9730093]
Level 1 (high-level) evidenceAtroshi I, Flondell M, Hofer M, Ranstam J. Methylprednisolone injections for the carpal tunnel syndrome: a randomized, placebo-controlled trial. Annals of internal medicine. 2013 Sep 3:159(5):309-17. doi: 10.7326/0003-4819-159-5-201309030-00004. Epub [PubMed PMID: 24026316]
Level 1 (high-level) evidenceLee JY, Park Y, Park KD, Lee JK, Lim OK. Effectiveness of ultrasound-guided carpal tunnel injection using in-plane ulnar approach: a prospective, randomized, single-blinded study. Medicine. 2014 Dec:93(29):e350. doi: 10.1097/MD.0000000000000350. Epub [PubMed PMID: 25546691]
Level 1 (high-level) evidenceHuisstede BM, Hoogvliet P, Randsdorp MS, Glerum S, van Middelkoop M, Koes BW. Carpal tunnel syndrome. Part I: effectiveness of nonsurgical treatments--a systematic review. Archives of physical medicine and rehabilitation. 2010 Jul:91(7):981-1004. doi: 10.1016/j.apmr.2010.03.022. Epub [PubMed PMID: 20599038]
Level 1 (high-level) evidenceGarfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher HR Jr. Yoga-based intervention for carpal tunnel syndrome: a randomized trial. JAMA. 1998 Nov 11:280(18):1601-3 [PubMed PMID: 9820263]
Level 1 (high-level) evidenceKaplan SJ, Glickel SZ, Eaton RG. Predictive factors in the non-surgical treatment of carpal tunnel syndrome. Journal of hand surgery (Edinburgh, Scotland). 1990 Feb:15(1):106-8 [PubMed PMID: 2307866]
Padua L, Padua R, Aprile I, Pasqualetti P, Tonali P, Italian CTS Study Group. Carpal tunnel syndrome. Multiperspective follow-up of untreated carpal tunnel syndrome: a multicenter study. Neurology. 2001 Jun 12:56(11):1459-66 [PubMed PMID: 11402101]
Level 2 (mid-level) evidenceVerdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. The Cochrane database of systematic reviews. 2008 Oct 8:2008(4):CD001552. doi: 10.1002/14651858.CD001552.pub2. Epub 2008 Oct 8 [PubMed PMID: 18843618]
Level 1 (high-level) evidenceGrosu-Bularda A, Vancea CV, Hodea FV, Cretu A, Bordeanu-Diaconescu EM, Dumitru CS, Ratoiu VA, Teodoreanu RN, Lascar I, Hariga CS. Optimizing Peripheral Nerve Regeneration: Surgical Techniques, Biomolecular and Regenerative Strategies-A Narrative Review. International journal of molecular sciences. 2025 Apr 20:26(8):. doi: 10.3390/ijms26083895. Epub 2025 Apr 20 [PubMed PMID: 40332790]
Level 3 (low-level) evidenceMahajan A, Derian A. Local Anesthetic Toxicity. StatPearls. 2024 Jan:(): [PubMed PMID: 29763139]
Sepulveda EA, Pak A. Lipid Emulsion Therapy. StatPearls. 2025 Jan:(): [PubMed PMID: 31751087]
Shi Q, MacDermid JC. Is surgical intervention more effective than non-surgical treatment for carpal tunnel syndrome? A systematic review. Journal of orthopaedic surgery and research. 2011 Apr 11:6():17. doi: 10.1186/1749-799X-6-17. Epub 2011 Apr 11 [PubMed PMID: 21477381]
Level 1 (high-level) evidenceStahl S, Yarnitsky D, Volpin G, Fried A. [Conservative therapy in carpal tunnel syndrome]. Harefuah. 1996 Feb 15:130(4):241-3; 295 [PubMed PMID: 8675116]
Turner A, Kimble F, Gulyás K, Ball J. Can the outcome of open carpal tunnel release be predicted?: a review of the literature. ANZ journal of surgery. 2010 Jan:80(1-2):50-4. doi: 10.1111/j.1445-2197.2009.05175.x. Epub [PubMed PMID: 20575880]
D'Arcy CA, McGee S. The rational clinical examination. Does this patient have carpal tunnel syndrome? JAMA. 2000 Jun 21:283(23):3110-7 [PubMed PMID: 10865306]
MacDermid JC, Wessel J. Clinical diagnosis of carpal tunnel syndrome: a systematic review. Journal of hand therapy : official journal of the American Society of Hand Therapists. 2004 Apr-Jun:17(2):309-19 [PubMed PMID: 15162113]
Level 1 (high-level) evidenceMosier BA, Hughes TB. Recurrent carpal tunnel syndrome. Hand clinics. 2013 Aug:29(3):427-34. doi: 10.1016/j.hcl.2013.04.011. Epub 2013 Jun 27 [PubMed PMID: 23895723]
Bland JD. Carpal tunnel syndrome. BMJ (Clinical research ed.). 2007 Aug 18:335(7615):343-6 [PubMed PMID: 17703044]
MacDonald RI, Lichtman DM, Hanlon JJ, Wilson JN. Complications of surgical release for carpal tunnel syndrome. The Journal of hand surgery. 1978 Jan:3(1):70-6 [PubMed PMID: 621368]
Level 3 (low-level) evidenceWipperman J, Goerl K. Carpal Tunnel Syndrome: Diagnosis and Management. American family physician. 2016 Dec 15:94(12):993-999 [PubMed PMID: 28075090]
Ozturk K, Esenyel CZ, Sonmez M, Esenyel M, Kahraman S, Senel B. Comparison of carpal tunnel injection techniques: a cadaver study. Scandinavian journal of plastic and reconstructive surgery and hand surgery. 2008:42(6):300-4. doi: 10.1080/02844310802401363. Epub [PubMed PMID: 18991172]
Gooding MS, Evangelista V, Pereira L. Carpal Tunnel Syndrome and Meralgia Paresthetica in Pregnancy. Obstetrical & gynecological survey. 2020 Feb:75(2):121-126. doi: 10.1097/OGX.0000000000000745. Epub [PubMed PMID: 32105336]
Level 2 (mid-level) evidence