Introduction
Kyphoscoliosis is defined as a combined abnormal curvature of the spine in both the sagittal (kyphosis typically >50 degrees) and coronal (scoliosis) planes, often accompanied by axial rotation of the spinal column.[1] Adult scoliosis is characterized by a lateral deviation of the spine >10 degrees in the coronal plane, as measured by the Cobb angle. Lateral deviations of <10 degrees can be attributed to postural variation rather than true scoliosis (see Image. Scoliosis of the Spine).
In the sagittal plane, kyphosis and lordosis describe the normal forward and backward curvatures of the spine, respectively. When viewed laterally, a normal lordotic curve is present in the cervical and lumbar regions, ranging from 35 to 80 degrees, while the thoracic spine demonstrates a physiologic kyphotic curve, typically between 30 and 50 degrees.[2] Notably, the degree of thoracic kyphosis increases with age: averaging 20 to 29 degrees in individuals younger than 40, 53 degrees in those aged 60 to 74, and 66 degrees in individuals older than 75.[3]
Although kyphoscoliosis most commonly affects the thoracolumbar region, this abnormal curvature may also occur in the cervicothoracic spine. Scoliosis is classified as mild when the Cobb angle ranges from 10 to 20 degrees, moderate when it ranges from 20 to 40 degrees, and severe when it exceeds 40 degrees.[4] The severity, location, number of vertebrae involved, and the extent of axial rotation all contribute to the clinical significance of the spinal deformity.[5] These factors can influence both energy expenditure and pulmonary function, often resulting in considerable physiological compromise.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Kyphoscoliosis Etiologies
Kyphoscoliosis is multifactorial in origin, often depending on a patient’s age, genetic background, comorbidities, and functional status. For clinical clarity, etiologies are typically categorized as idiopathic, secondary (acquired or disease-related), congenital, or functional.
Idiopathic etiologies
Kyphoscoliosis with unclear underlying causes includes:
- Adolescent idiopathic scoliosis (AIS): The most prevalent form, characterized by a lateral spinal curvature exceeding 10 degrees without a known cause. It predominantly affects adolescents during periods of rapid growth.[6][7][8]
- Scheuermann disease: Also known as juvenile kyphosis, this condition involves anterior wedging of 3 or more consecutive vertebrae by at least 5 degrees, leading to a rigid kyphotic deformity. The exact etiology remains unclear but is believed to be multifactorial, involving genetic and environmental factors.[9]
Secondary causes
Secondary etiologies of kyphoscoliosis include the following acquired or disease-related conditions associated with abnormal curvature of the spine:
- Degenerative changes: Age-related degeneration of intervertebral discs and facet joints can lead to spinal deformities.
- Posttraumatic deformities: Spinal injuries or fractures can result in abnormal curvatures due to malalignment during healing.
- Iatrogenic causes: Surgical interventions, such as laminectomies or spinal fusions, may inadvertently lead to spinal instability and deformities.
- Neuromuscular disorders: Conditions like cerebral palsy, muscular dystrophy, and spinal muscular atrophy can cause muscle imbalances, leading to spinal curvatures (see Image. Scoliosis with Duchenne Muscular Dystrophy).[10]
- Connective tissue disorders: Diseases, eg, Marfan syndrome and Ehlers-Danlos syndrome, affect the integrity of connective tissues, predisposing individuals to spinal deformities. The kyphoscoliosis type of Ehlers-Danlos syndrome, caused by lysyl hydroxylase deficiency, is characterized by severe congenital kyphoscoliosis, skin fragility, and ocular complications.
- Infectious causes: Infections, eg, tuberculosis, can affect the vertebral bodies, leading to structural deformities.
- Substance abuse [11]
Congenital causes
Congenital etiologies result from vertebral malformations during embryonic development, including:
- Failure of formation: Incomplete development of vertebral structures (eg, hemivertebrae)
- Failure of segmentation: Incomplete separation of vertebrae, leading to block vertebrae [12][13]
Functional causes
Functional etiologies are typically reversible and, unlike structural deformities, do not involve permanent changes to the vertebral anatomy; they often resolve with appropriate interventions. Functional causes of kyphoscoliosis include:
- Postural habits: Prolonged poor posture can lead to adaptive spinal curvatures.
- Muscle spasms: Pain-induced muscle contractions can cause temporary spinal deviations.
Epidemiology
The precise epidemiology of kyphoscoliosis remains difficult to establish due to its heterogeneous etiologies, including idiopathic, congenital, neuromuscular, and syndromic origins. As such, prevalence and demographic trends are better appreciated when examined in the context of specific underlying causes. In population-based studies, the overall prevalence of kyphoscoliosis is estimated to be approximately 1 in 1,000 individuals, although this varies with age and etiology.[14]
Scheuermann disease, a frequent cause of kyphoscoliosis in adolescents, has a reported prevalence ranging from 0.4% to 8%, depending on diagnostic criteria and population sampled.[15] It predominantly affects adolescents between the ages of 12 and 17 years, with a male predominance reported in several studies (male-to-female ratio up to 2:1).[16] Scheuermann disease more commonly involves the thoracic spine, although thoracolumbar variants also exist and may be underdiagnosed.
In neuromuscular conditions, such as Duchenne muscular dystrophy and cerebral palsy, the prevalence of kyphoscoliosis can exceed 50% in nonambulatory individuals, reflecting the impact of muscle imbalance and chronic postural adaptations.[17] In older adults, kyphoscoliosis can result from degenerative spinal changes, with prevalence increasing with age, particularly in women with osteoporosis-related vertebral compression fractures.[18]
Pathophysiology
The pathophysiology of kyphoscoliosis depends on the underlying etiology, such as the following:
- Postural thoracic kyphosis: Often observed in adolescents, this form is attributed to reversible muscular imbalances, particularly weakness in the back extensor muscles. Such imbalances lead to excessive curvature of the thoracic spine.
- Age-related hyperkyphosis: In the older adult, approximately 60% to 70% of hyperkyphosis cases are not due to vertebral compression fractures.[19] Instead, factors like degenerative disc disease, genetic predisposition, and weakness of the back extensor muscles play significant roles. When fractures are involved, they typically present as anterior wedge deformities, leading to progressive curvature and altered spinal load distribution.
- Postinfectious kyphoscoliosis: Conditions, eg, postpolio residual paralysis (PPRP), can compromise the structural integrity of the anterior spinal column, leading to exaggerated spinal curvature. Studies have reported kyphoscoliosis in approximately 12% of patients with PPRP.[20] In patients with postpoliomyelitic kyphoscoliosis, ventilatory control may be impaired due to both respiratory muscle weakness and central drive dysfunction
- Congenital neuromuscular disorders: Diseases like congenital neuromuscular disease with uniform type 1 fibers (CNMDU1) are associated with severe and progressive kyphoscoliosis. Early diagnosis through muscle biopsy is crucial, as these conditions can lead to significant spinal deformities and respiratory complications.[13]
History and Physical
Kyphoscoliosis Clinical History
Kyphoscoliosis presents in various age-specific clinical manifestations, ranging from asymptomatic pediatric cases to adult patients with respiratory or neurological complications.
Pediatric and adolescent presentations
Children with kyphoscoliosis often present asymptomatically, with concerns typically raised by caregivers noticing physical asymmetries, eg, uneven shoulders or hips, prominence of the spine or scapula, an uneven waistline, or changes in gait. Neurological symptoms like chronic pain, weakness, tingling, or bowel/bladder dysfunction are uncommon in this population and warrant thorough evaluation for underlying pathologies.[21]
A comprehensive history should encompass growth patterns, the age at onset of spinal changes, the presence of neurological symptoms, and the psychosocial impacts. Early referral to orthopedic or neurosurgical specialists is advisable for young children to facilitate timely intervention and alleviate parental concerns.
Adult and older adult presentations
In adults, kyphoscoliosis may manifest with axial back pain, cosmetic concerns, or progressive respiratory dysfunction. A detailed history should assess the duration and progression of symptoms, as well as functional limitations and any neurological or psychosocial issues. In older adult patients, degenerative changes and muscle weakness are common contributors to spinal deformities.
Patients with severe kyphoscoliosis often experience nocturnal hypoventilation, especially during rapid eye movement (REM) sleep, leading to oxygen desaturation, morning headaches due to carbon dioxide retention, and excessive daytime sleepiness.
Kyphoscoliosis Physical Examination Findings
The physical examination should begin with an assessment of posture, spinal alignment, and symmetry. Observation for skin changes, including café-au-lait spots, dimples, or hair tufts, is essential for identifying conditions, eg, neurofibromatosis or spina bifida.[21][22]
The Adams forward bend test is a key screening tool for assessing flexibility. The patient stands with feet shoulder-width apart and bends forward at the waist to a 90-degree angle, allowing the examiner to observe for rib humps or spinal asymmetry. A scoliometer can quantify the angle of trunk rotation; readings of 7 degrees or greater often correlate with a spinal curve of 20 degrees on radiographs. For patients unable to perform this test, modified assessments with caregiver assistance may be utilized. If asymmetry is noted on examination, radiographic images may be obtained to supplement clinical findings.[21]
Neurological evaluation should include assessments of muscle strength, reflexes, sensation, and coordination. Gait analysis and evaluation for limb length discrepancies are also important. Functional tests, eg, the Timed Up and Go, 6-minute walk test, and chair rise test, can provide insights into the patient’s mobility and endurance.[3] (Please refer to the Evaluation section for more information on diagnostic testing.)
Evaluation
A comprehensive evaluation of kyphoscoliosis encompasses a detailed history, physical examination, functional assessment, and imaging studies.
Functional Assessment
The 6-minute walk test serves as a practical tool to assess exercise tolerance and functional capacity in patients with kyphoscoliosis. Studies have demonstrated that desaturation during the 6-minute walk test correlates with the severity of spinal deformity, whereas pulmonary function tests (PFTs) and arterial blood gas (ABG) parameters may not show a direct correlation.[23]
Imaging Studies
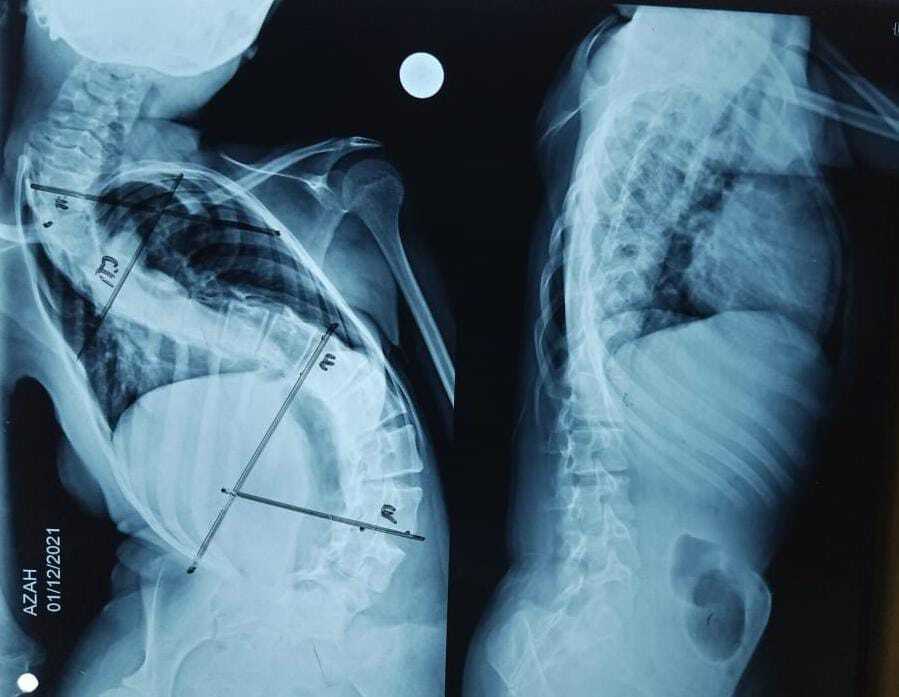
Radiographic imaging is pivotal in evaluating the extent and progression of spinal curvature. Standard imaging includes upright posteroanterior and lateral views of the cervical, thoracic, and lumbar spine. Ensure proper patient positioning and pelvic leveling to avoid apparent limb length discrepancies on radiographs (see Image. Scoliotic Spine).
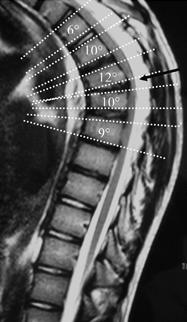
The Cobb angle remains the gold standard for quantifying spinal deformities. Kyphosis is the normal posterior curvature of the thoracic spine, typically measured as a Cobb angle of approximately 20 to 40 degrees in healthy adults. Angles above this range are considered excessive or hyperkyphotic.[21] Measurement involves drawing lines parallel to the superior endplate of the uppermost vertebra and the inferior endplate of the lowermost vertebra involved in the curve; the angle between these lines represents the degree of curvature (see Image. Technique of determining degree of kyphosis on lateral imaging).[1] Assessment of sagittal balance is also crucial. A plumb line dropped from the center of the C7 vertebral body should ideally intersect the posterior superior corner of the S1 vertebral body. Deviation anteriorly indicates positive sagittal balance, while posterior deviation suggests negative sagittal balance.[10] A 3-dimensional computed tomography (CT) reconstruction can aid preoperative planning by delineating complex vertebral anatomy and rib involvement.
Imaging Classification Systems
Adolescent idiopathic scoliosis (AIS) involves structural abnormalities in the coronal, sagittal, and axial planes. In 1983, the King classification was established to describe the 5 thoracic curve types and the spinal arthrodesis recommended for specific vertebral levels.[24] As surgical techniques and equipment evolved, limitations of the King Classification were brought to light, and the system fell out of favor. The Lenke classification system, established in 2001, offers a comprehensive approach by incorporating curve type (1–6), lumbar spine modifier (A, B, C), and sagittal thoracic modifier (-, N, +). This system aids in surgical planning by identifying structural curves requiring fusion. Further details on these classifications and their criteria are beyond the scope of this course.[24][25]
Advanced Imaging and Bone Health
When surgical intervention is contemplated, advanced imaging modalities, eg, MRI, can provide detailed insights into spinal cord and soft tissue involvement. Additionally, bone mineral density (BMD) assessments are recommended, as osteoporosis can influence surgical outcomes and postoperative recovery.
Pulmonary Evaluation
Structural spinal deformities in kyphoscoliosis often lead to restrictive lung patterns, characterized by reduced forced vital capacity (FVC) and forced expiratory volume in 1 second (FEV1). Pulmonary function tests are essential in evaluating the extent of respiratory compromise. In severe cases, echocardiography is warranted to assess for pulmonary hypertension and right heart strain.[26][27] When the Cobb angle exceeds 90 to 100 degrees, total lung capacity and vital capacity may be reduced to 30% of the predicted value, severely increasing the work of breathing and the risk of respiratory muscle fatigue.
Additionally, comprehensive polysomnography is recommended to assess for obstructive sleep apnea, central hypoventilation, and nocturnal desaturation, guiding titration of bilevel positive airway pressure therapy where indicated.
Anesthetic Assessment
Kyphoscoliosis can complicate regional anesthesia and intubation due to altered spine anatomy and tracheal distortion, requiring careful preoperative planning and imaging.
Treatment / Management
Management of kyphoscoliosis is tailored based on factors, eg, the underlying etiology, patient age, severity of the deformity, and the presence of neurological deficits. Initial approaches are typically conservative, with surgical interventions considered for progressive or refractory cases. In younger patients, kyphoscoliosis may be an incidental finding with little to no effect on function. However, if pathology is significant enough to cause pain, neurologic changes, concerns of cosmesis, or concerns of progression, then further testing and referral to a specialist are recommended.
Conservative Management Approach
Observation
For asymptomatic or minimally affected individuals, regular monitoring with serial imaging and functional assessments is appropriate to track curvature progression and symptom development.
Pain management
Nonsteroidal anti-inflammatory drugs (NSAIDs) are first-line for pain control. Caution is advised with opioids due to potential respiratory depression, especially in patients with compromised pulmonary function. Muscle relaxants like cyclobenzaprine may be prescribed, but patients should be monitored for sedation and other adverse effects.
Respiratory support
Structural deformities can lead to restrictive lung disease, resulting in hypoventilation and chronic respiratory failure. These may be caused by restriction of thoracic wall movement, decreased chest compliance, and limited diaphragmatic motion.[28] The hypoxemia resulting from these changes may result in a reflexive vasoconstrictive response leading to pulmonary hypertension. Patients should be assessed for associated conditions, including sleep apnea, daytime fatigue, and snoring.[23](B3)
Long-term nocturnal noninvasive positive pressure ventilation
Long-term nocturnal noninvasive positive pressure ventilation (NIPPV) has been shown to improve gas exchange, exercise capacity, and reduce pulmonary hypertension in severe cases. Adjunct therapies may include bronchodilators, diuretics, and chest physiotherapy. Immunizations against influenza and pneumococcus are recommended to prevent respiratory infections.
In patients with pulmonary arterial hypertension, studies have noted the use of endothelin receptor antagonists and inhaled prostanoids. Managing respiratory decline can be difficult and complex, and patients tend to continue to deteriorate despite treatment.[29] Long-term nocturnal NIPPV can normalize daytime carbon dioxide levels, improve sleep quality, and is superior to long-term oxygen therapy alone for chronic respiratory failure in severe kyphoscoliosis.(B3)
Cardiac evaluation
Transthoracic echocardiography (TTE) is essential to assess for right ventricular overload and pulmonary hypertension, which can result from chronic hypoxemia associated with kyphoscoliosis.
Bracing
In skeletally immature patients, orthotic bracing can halt or slow the progression of spinal curvature. Effectiveness is higher when initiated before the curvature exceeds 50 degrees. Modern braces, designed using computer-aided design and manufacturing (CAD/CAM) technology, offer enhanced customization and improved comfort.[30] Bracing can provide support to weakened musculature and corrective pressures on abnormal curvature (see Image. Chêneau Brace).[31][32] (B3)
Physical therapy and exercise
Structured exercise programs focusing on spinal stabilization, flexibility, and posture correction can be beneficial. The Scientific Exercises Approach to Scoliosis (SEAS) is an individualized program that has shown efficacy in managing scoliosis and kyphosis.[33] However, these programs have a minimal impact on improving lumbar lordotic curvature. These exercise programs may also utilize specific methods, eg, Pilates, Williams’ flexion exercises (which combine stretching and strengthening), and Kendall’s theory (which focuses on local corrective exercises that strengthen weakened muscles and stretch shortened musculature).[34] Targeted exercise programs may be effective for older patients with hyperkyphosis.(A1)
Spinal cord stimulation
Spinal cord stimulation (SCS) can be considered for patients with chronic back pain that is refractory to conservative interventions. It may be appropriate for patients who are deemed poor surgical candidates or for those who are averse to corrective surgery. In addition, SCS may be an option for those with failed back surgery syndrome.[35] SCS is a minimally invasive technique that utilizes the delivery of electrical impulses to the spinal cord to interrupt pain signaling to the brain. Research on the use of SCS in kyphoscoliosis is lacking; therefore, success rates, optimal frequency, and complications remain uncertain.[36](B3)
Lifestyle modifications
Encouraging smoking cessation, weight management, and regular physical activity can improve overall health and potentially mitigate symptom progression. Yoga may alleviate pain in some; however, care should be taken to avoid extreme hyperflexion and hyperextension, especially in patients with osteopenia or osteoporosis.[37] Extensive information on the use of yoga appears limited, as several studies have listed the condition as meeting criteria for exclusion.
Psychosocial support
Regular screening for anxiety and depression is important, as chronic musculoskeletal conditions can significantly impact mental health.
Surgical Management
Surgical intervention is considered for patients with:
- Progressive curvature exceeding 45 to 50 degrees.
- Intractable pain unresponsive to conservative measures.
- Neurological deficits or spinal cord compression.[22]
- Severe cosmetic deformity impacting quality of life. (B3)
Surgical correction for a hypermobile spine can include an arthrodesis and the use of hardware, including rods, wires, and screws, whereas osteotomies can be used to relieve rigid spines. In patients without neurological compromise, procedures, such as vertebroplasty and kyphoplasty, have recently gained favor as a means for vertebral augmentation. (see Images. Percutaneous Vertebroplasty and Kyphoplasty and Cement Injection During Percutaneous Kyphoplasty)
Operative management may be indicated in those patients who have failed conservative therapy, experience intractable pain, have an onset of neurologic changes, or have persistent progression despite bracing.[38] In severe, rigid deformities, especially with underlying neurofibromatosis, spinal traction should be used cautiously as it may increase tension on the spinal cord.[39](B3)
Surgical therapies
Specific surgical interventions that may be considered in patients with kyphoscoliosis include:
- Laminectomy alone for kyphotic cord compression is absolutely contraindicated as it does not relieve the anterior compression on the cord and has not been shown to improve the neurological deficits.
- Spinal fusion: Posterior or anterior spinal fusion stabilizes the spine and prevents further curvature progression
- Osteotomies
- Smith-Petersen osteotomy (posterior column wedge osteotomy with the opening of the anterior column) is used for Scheuermann disease and flat-back syndrome.
- Ponte osteotomy (posterior closing wedge osteotomy) is used for the treatment of Scheuermann disease.
- Pedicle subtraction osteotomy is employed to correct rigid deformities (posterior closing wedge osteotomy) for the treatment of Scheuermann disease.
- Vertebral column resection (VCR): In severe, rigid deformities, VCR allows for significant correction by removing ≥1 vertebral segments.
- Growth-friendly techniques: In pediatric patients, techniques like the hybrid growing rod allow for deformity correction while accommodating spinal growth.[20] (B3)
Postoperative care includes pain management, monitoring for neurological changes, and respiratory support as needed. Surgical risks are higher in older adult patients due to comorbidities and decreased bone quality; thus, careful patient selection is crucial.[10][3](A1)
Differential Diagnosis
Kyphoscoliosis can occur as an isolated idiopathic finding, particularly in adolescents, or as a manifestation of a broader underlying pathology. In clinical evaluation, the goal is to distinguish between primary spinal deformities and those secondary to systemic, neuromuscular, or structural causes. Identifying associated features, including age of onset, progression rate, neurologic findings, cutaneous markers, or systemic symptoms, can be pivotal in narrowing the differential.
Rather than approaching kyphoscoliosis as a standalone diagnosis, clinicians are advised to assess the underlying etiology, especially when it presents alongside other abnormalities or signs suggestive of congenital, neuromuscular, metabolic, or infectious processes.
Differential diagnoses that should also be considered include:
- Idiopathic kyphoscoliosis: Most common in adolescents; the diagnosis is made by exclusion. Patients are typically otherwise healthy and present during periods of rapid growth.
- Adolescent idiopathic scoliosis (AIS): A structural curvature of the spine in individuals 10 years or older, with no underlying neurologic or musculoskeletal cause. The curvature involves rotation and typically lacks significant kyphotic changes (see Image. Adolescent Idiopathic Scoliosis).
- Infantile idiopathic scoliosis with kyphosis: Occurs in children under 3 years old. It may spontaneously resolve or progress rapidly and should prompt early orthopedic referral.
- Scheuermann disease: A structural hyperkyphosis seen in adolescents, characterized by anterior wedging of at least 3 contiguous vertebrae, endplate irregularities, and Schmorl nodes on imaging (see Image. Hyperkyphosis). Scheuermann disease may be mistaken for postural kyphosis, but it typically presents with rigidity and pain.
- Osteoporosis: Common in older adults and may cause compression fractures leading to progressive kyphosis. Consider especially in postmenopausal women and individuals on long-term corticosteroids.
- Age-related hyperkyphosis: Often multifactorial due to degenerative disc disease, vertebral compression fractures, and muscular weakness. Distinguished from structural kyphoscoliosis by its gradual onset and age of presentation.
- Vertebral compression fractures: Can cause acute or progressive kyphotic deformity, particularly in older adult patients or those with trauma or metastatic bone disease.
- Infections: Spinal infections (eg, tuberculosis, echinococcus granulosus, Potts disease) can lead to vertebral destruction and angular kyphosis. Hydatid disease can also involve the spine, especially in endemic regions, and should be considered when imaging reveals cystic lesions.[40]
- Spinal tumors: Primary or metastatic spinal tumors can cause vertebral collapse, instability, and deformity. Neurological signs, eg, radiculopathy or myelopathy, may be present.
- Congenital malformations: Genetic or syndromic causes (eg, Kniest dysplasia, hemivertebrae) involve vertebral segmentation defects, dwarfism, and other musculoskeletal abnormalities.
- Neuromuscular disorders
- Friedreich ataxia: A hereditary neurodegenerative condition often associated with scoliosis, gait disturbance, and cardiomyopathy. Kyphoscoliosis is common and may progress rapidly.
- Cerebral palsy, muscular dystrophies, and spinal muscular atrophy: All can lead to progressive spinal deformities due to muscle imbalance and weakness.
- Connective tissue disorders: Conditions, eg, Marfan syndrome or Ehlers-Danlos syndrome, can cause spinal instability and abnormal curvature.
- Myelomeningocele and neurofibromatosis Type 1 (NF1): These congenital disorders may manifest with spinal deformities, skin findings (eg, café-au-lait spots and subcutaneous nodules), and neurological involvement.
Prognosis
The prognosis for kyphoscoliosis is guarded and is dependent on the underlying etiology contributing to disease progression. Kyphoscoliosis complicated by pulmonary hypertension is associated with high mortality.[29]
Complications
Kyphoscoliosis, particularly when severe or progressive, can lead to a wide range of complications that affect musculoskeletal, cardiopulmonary, neurological, and psychosocial domains. Complications may arise from the natural progression of the deformity, the underlying etiology, or as a result of treatment interventions, including both conservative and surgical approaches.
Complications associated with kyphoscoliosis often develop gradually and may remain unnoticed, particularly those involving pulmonary function. Consistent monitoring of respiratory status, spinal curvature progression, and general health remains essential for early intervention and risk mitigation.
Pulmonary Complications
Restrictive lung disease represents one of the most frequent and severe consequences of kyphoscoliosis. The deformity limits the thoracic cavity volume, impairs diaphragmatic excursion, and reduces chest wall compliance, resulting in compromised ventilation. Chronic hypercapnic respiratory failure often develops due to persistent alveolar hypoventilation, particularly in individuals with severe thoracic curvature.
Sleep-disordered breathing, including obstructive sleep apnea and hypoventilation syndromes, may emerge and exacerbate daytime fatigue while increasing cardiovascular risk. Impaired airway clearance and decreased pulmonary reserve contribute to the recurrence of respiratory infections. Many patients adopt a rapid, shallow breathing pattern to minimize the effort required for ventilation, but this adaptation increases dead space and promotes atelectasis. Chronic hypoxia from progressive respiratory compromise frequently results in vascular remodeling, elevated pulmonary artery pressure, and the eventual onset of pulmonary hypertension and cor pulmonale.[41]
Cardiovascular Complications
Right ventricular hypertrophy and failure may occur secondary to long-standing hypoxemia and pulmonary hypertension. Exercise tolerance diminishes significantly due to the combined burden of respiratory restriction and cardiovascular strain.
Neurological Complications
Spinal cord compression can develop from progressive deformity or structural anomalies, eg, herniated discs, osteophytes, or tethered cord, leading to myelopathy. Radiculopathy or peripheral neuropathy may result from nerve root compression or narrowing of the neural foramina. High-risk deformity correction surgeries carry the potential for postoperative neurologic injury.
Musculoskeletal Complications
Chronic back pain and muscular fatigue arise from mechanical imbalance and sustained muscular effort. Instability of the spine often develops in the presence of vertebral fractures, degenerative changes, or failed surgical constructs. Despite bracing or conservative therapy, curvature progression may continue, especially in skeletally immature patients.
Postsurgical Complications
Surgical interventions carry risks, eg, infection, which may involve the wound or implanted hardware. Hardware failure—including breakage, loosening, or displacement of rods, plates, or screws—can compromise surgical outcomes. Pseudoarthrosis, or failure of spinal fusion, occurs more frequently in long fusion segments or among patients with diminished bone quality.
Proximal junctional kyphosis (PJK) develops at the upper end of a fusion construct, leading to abnormal angulation and potential clinical deterioration. Perioperative pulmonary or cardiac decompensation is a serious concern in patients with existing cardiopulmonary dysfunction. Cement leakage during vertebroplasty or kyphoplasty also poses a significant risk during intraoperative procedures (see Image. Cement Injection During Percutaneous Kyphoplasty).
Psychosocial Complications
Many patients, especially adolescents or those with prominent spinal deformity, experience body image disturbance. Depression and anxiety frequently accompany chronic pain, physical limitations, and reduced social engagement. A diminished quality of life stems from ongoing discomfort, impaired respiratory function, and a loss of independence.
Deterrence and Patient Education
Patients should be educated on how these structural changes may result in physical limitations, an increased risk of falls, diminished strength, reduced pulmonary function, and an increased mortality rate.[3]
Enhancing Healthcare Team Outcomes
Effective management of kyphoscoliosis demands a multidisciplinary strategy rooted in comprehensive interprofessional collaboration. Physicians and advanced practitioners play a central role in initial assessment, diagnosis, and conservative management, often initiating treatment plans that include physical therapy, pain control, bracing, and monitoring of disease progression. When the curvature rapidly advances or symptoms such as intractable pain or neurologic deficits emerge, timely referral to an orthopedic or neurosurgical specialist becomes essential. Surgeons then evaluate the need for operative correction, while pulmonologists assess and manage associated respiratory complications that frequently accompany severe thoracic deformities. Continuous communication between these clinicians ensures appropriate escalation of care and coordinated planning for perioperative and long-term management.
Nurses and therapists contribute significantly by providing ongoing education, reinforcing home care instructions, and monitoring functional capacity. Physical and occupational therapists help patients improve posture, balance, and mobility, while orthotists design and adjust braces to minimize curve progression in growing patients. Pharmacists offer vital input on medication safety, especially in managing chronic pain, avoiding respiratory depressants in vulnerable patients, and supporting respiratory therapies. Incorporating patients and families into care decisions fosters shared understanding and promotes adherence to treatment regimens. This integrated, patient-centered model enhances safety, preserves independence, and improves both short- and long-term health outcomes, while strengthening the overall performance of the care team.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
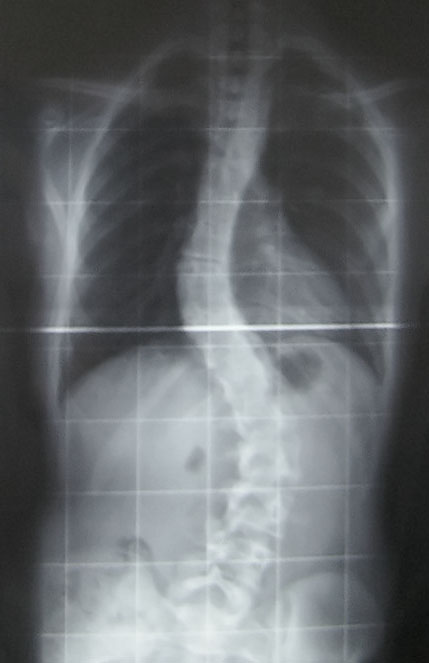
Adolescent Idiopathic Scoliosis. This image is a posterior-to-anterior radiograph of an adolescent idiopathic scoliosis case. There is a thoracic curve of 30° and a lumbar curve of 53° (Cobb angle). This image was taken at the Royal National Orthopaedic Hospital. The largest curve (53°) is typically near the lower surgery boundary, although many factors decide whether surgery is necessary in a scoliosis case.
Silverjohnny, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
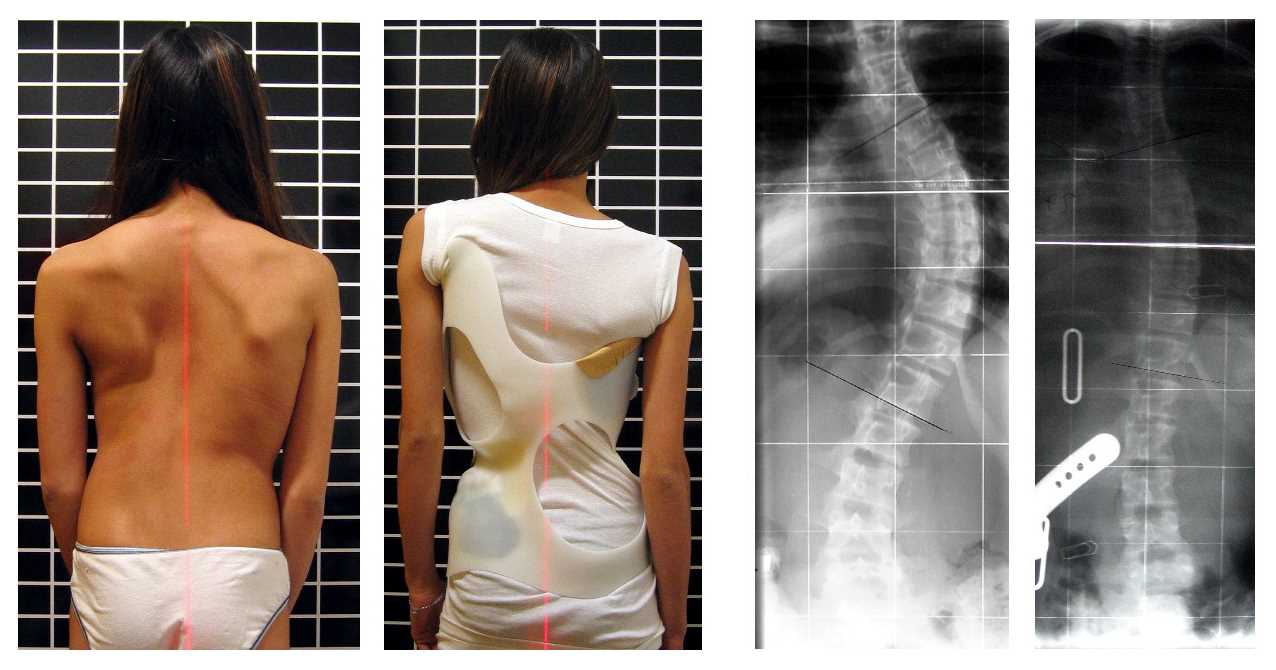
Chêneau Brace. The image shows a patient with scoliosis wearing a Chêneau brace, which has corrected the spinal curvature from 56° to 27° Cobb (primary correction of 52%).
Weiss HR, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Image to Enlarge)
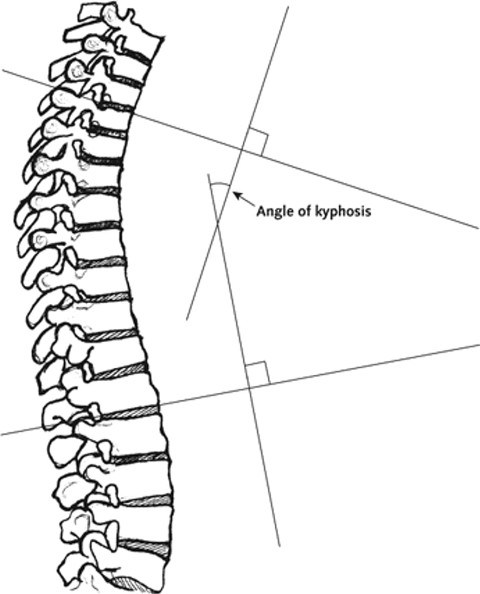
Kyphosis Imaging Techniques. The following technique is used for determining degree of kyphosis on lateral imaging: 1) Line is drawn along the superior endplate of the most tilted vertebrae on the cephalad portion of the kyphotic curve; 2) Line is drawn along the inferior endplate of the most tilted vertebrae on the caudal portion of the kyphotic curve; and 3) The angle formed by the intersection of lines perpendicular to the above described lines is the measured Cobb angle.
Kado DM, Prenovost K, Crandall C. Narrative review: hyperkyphosis in older persons. Ann Int Med. 2007;147:330–338.
(Click Image to Enlarge)
(Click Image to Enlarge)
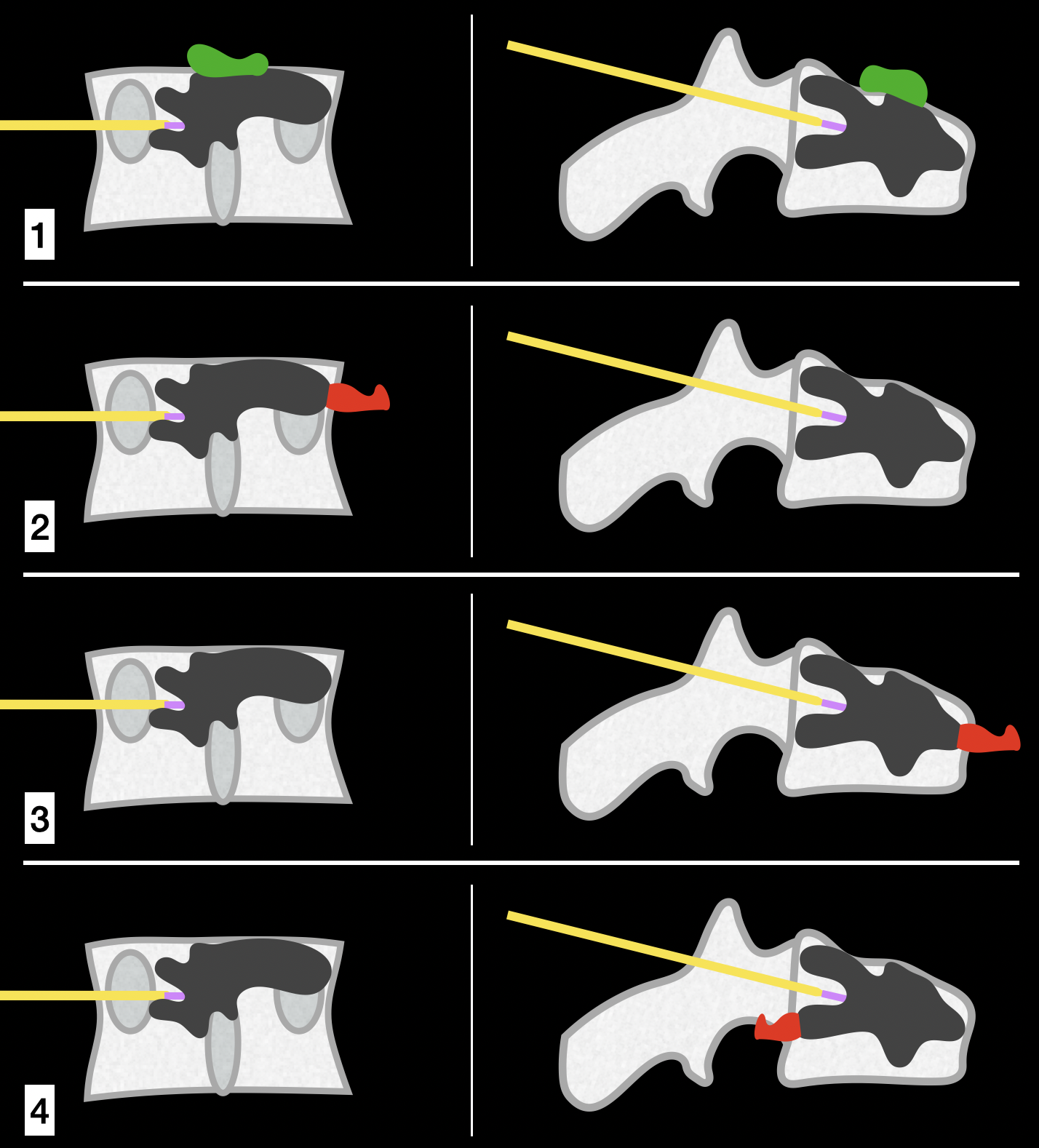
Cement Leakage Complications in Vertebroplasty and Kyphoplasty. The left-sided image for each type of cement leakage represents the anteroposterior fluoroscopic view, and the right-sided image shows the lateral fluoroscopic view. (1) Cement leakage superiorly (green) or inferiorly (not shown) into the disc space. This type of leakage is typically tolerated and is visible on both anteroposterior and lateral views. (2) Cement leakage laterally (dangerous-red). This type of leakage is visible only on anteroposterior views. (3) Cement leakage anteriorly (dangerous-red). This type of leakage is visible only on lateral views. (4) Cement leakage posteriorly (dangerous-red). This type of leakage is visible only on lateral views.
Contributed by K Margetis, MD, PhD
References
Papaliodis DN, Bonanni PG, Roberts TT, Hesham K, Richardson N, Cheney RA, Lawrence JP, Carl AL, Lavelle WF. Computer Assisted Cobb Angle Measurements: A novel algorithm. International journal of spine surgery. 2017:11(3):21. doi: 10.14444/4021. Epub 2017 Jun 30 [PubMed PMID: 28765805]
Ailon T, Smith JS, Shaffrey CI, Lenke LG, Brodke D, Harrop JS, Fehlings M, Ames CP. Degenerative Spinal Deformity. Neurosurgery. 2015 Oct:77 Suppl 4():S75-91. doi: 10.1227/NEU.0000000000000938. Epub [PubMed PMID: 26378361]
Ailon T, Shaffrey CI, Lenke LG, Harrop JS, Smith JS. Progressive Spinal Kyphosis in the Aging Population. Neurosurgery. 2015 Oct:77 Suppl 4():S164-72. doi: 10.1227/NEU.0000000000000944. Epub [PubMed PMID: 26378354]
Fabijan A, Zawadzka-Fabijan A, Fabijan R, Zakrzewski K, Nowosławska E, Polis B. Assessing the Accuracy of Artificial Intelligence Models in Scoliosis Classification and Suggested Therapeutic Approaches. Journal of clinical medicine. 2024 Jul 9:13(14):. doi: 10.3390/jcm13144013. Epub 2024 Jul 9 [PubMed PMID: 39064053]
Johari J, Sharifudin MA, Ab Rahman A, Omar AS, Abdullah AT, Nor S, Lam WC, Yusof MI. Relationship between pulmonary function and degree of spinal deformity, location of apical vertebrae and age among adolescent idiopathic scoliosis patients. Singapore medical journal. 2016 Jan:57(1):33-8. doi: 10.11622/smedj.2016009. Epub [PubMed PMID: 26831315]
Grivas TB, Vasiliadis E, Soultanis K, Lykissas M, Katzouraki G, Sekouris N, Lykouris D, Mazioti C, Mamzeri A, Papagianni D, Potamiti E, Kastrinis A, Theodosopoulos E. Idiopathic Scoliosis Progression: Presenting Rib and Segmental Rib Index as Predictors-A Literature Review. Medical sciences (Basel, Switzerland). 2025 May 21:13(2):. doi: 10.3390/medsci13020062. Epub 2025 May 21 [PubMed PMID: 40407557]
Kubat O, Ovadia D. Frontal and sagittal imbalance in patients with adolescent idiopathic deformity. Annals of translational medicine. 2020 Jan:8(2):29. doi: 10.21037/atm.2019.10.49. Epub [PubMed PMID: 32055620]
Menger RP, Sin AH. Adolescent Idiopathic Scoliosis. StatPearls. 2025 Jan:(): [PubMed PMID: 29763083]
Hershkovich O, Gordon B, Derazne E, Tzur D, Afek A, Lotan R. Hypermobility Among Adolescents and the Association With Spinal Deformities: A Large Cross-Sectional Study. Journal of the American Academy of Orthopaedic Surgeons. Global research & reviews. 2024 Jul 1:8(7): [PubMed PMID: 38996221]
Level 2 (mid-level) evidenceYaman O, Dalbayrak S. Kyphosis and review of the literature. Turkish neurosurgery. 2014:24(4):455-65. doi: 10.5137/1019-5149.JTN.8940-13.0. Epub [PubMed PMID: 25050667]
Level 1 (high-level) evidenceRezvani M, Sadeghi SM, Masaeli F, Thapa A, Shah A, Mahmoudi F. Exploring "Intoxicated Syndrome": A rare case of cervical kyphoscoliosis due to drug abuse. Clinical case reports. 2025 Apr:13(4):e9531. doi: 10.1002/ccr3.9531. Epub 2025 Apr 22 [PubMed PMID: 40264730]
Level 3 (low-level) evidenceSato T, Takahashi I, Watanabe Y, Yokoyama D, Shimokawa N. Congenital kyphoscoliosis: Analysis of vertebral abnormalities using model animals (Review). Experimental and therapeutic medicine. 2024 Nov:28(5):416. doi: 10.3892/etm.2024.12705. Epub 2024 Sep 4 [PubMed PMID: 39301254]
Level 3 (low-level) evidenceImagama S, Kawakami N, Tsuji T, Ohara T, Ishiguro N. Kyphoscoliosis associated with congenital neuromuscular disease with uniform type 1 fibers. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012 Jun:21 Suppl 4(Suppl 4):S499-504. doi: 10.1007/s00586-011-2128-4. Epub 2011 Dec 23 [PubMed PMID: 22193842]
Level 3 (low-level) evidenceWalters S, Barkham B, Bishop T, Bernard J, Coroyannakis C, Thilaganathan B, Lui DF. Fetal Scoliosis: Natural History and Outcomes. Journal of the American Academy of Orthopaedic Surgeons. Global research & reviews. 2024 Jun 1:8(6): [PubMed PMID: 38996079]
Lowe TG, Line BG. Evidence based medicine: analysis of Scheuermann kyphosis. Spine. 2007 Sep 1:32(19 Suppl):S115-9 [PubMed PMID: 17728677]
Sebaaly A, Farjallah S, Kharrat K, Kreichati G, Daher M. Scheuermann's kyphosis: update on pathophysiology and surgical treatment. EFORT open reviews. 2022 Dec 7:7(11):782-791. doi: 10.1530/EOR-22-0063. Epub 2022 Dec 7 [PubMed PMID: 36475554]
Berven S, Bradford DS. Neuromuscular scoliosis: causes of deformity and principles for evaluation and management. Seminars in neurology. 2002 Jun:22(2):167-78 [PubMed PMID: 12524562]
Katzman WB, Wanek L, Shepherd JA, Sellmeyer DE. Age-related hyperkyphosis: its causes, consequences, and management. The Journal of orthopaedic and sports physical therapy. 2010 Jun:40(6):352-60. doi: 10.2519/jospt.2010.3099. Epub [PubMed PMID: 20511692]
Roghani T, Zavieh MK, Manshadi FD, King N, Katzman W. Age-related hyperkyphosis: update of its potential causes and clinical impacts-narrative review. Aging clinical and experimental research. 2017 Aug:29(4):567-577. doi: 10.1007/s40520-016-0617-3. Epub 2016 Aug 18 [PubMed PMID: 27538834]
Level 3 (low-level) evidenceAhuja V, Gombar S, Singla D. A rare case of postpoliomyelitis quadriparetic patient with severe kyphoscoliosis. Journal of anaesthesiology, clinical pharmacology. 2015 Apr-Jun:31(2):266-8. doi: 10.4103/0970-9185.155206. Epub [PubMed PMID: 25948920]
Level 3 (low-level) evidenceSheehan DD, Grayhack J. Pediatric Scoliosis and Kyphosis: An Overview of Diagnosis, Management, and Surgical Treatment. Pediatric annals. 2017 Dec 1:46(12):e472-e480. doi: 10.3928/19382359-20171113-01. Epub [PubMed PMID: 29227524]
Level 3 (low-level) evidenceSingh K, Samartzis D, An HS. Neurofibromatosis type I with severe dystrophic kyphoscoliosis and its operative management via a simultaneous anterior-posterior approach: a case report and review of the literature. The spine journal : official journal of the North American Spine Society. 2005 Jul-Aug:5(4):461-6 [PubMed PMID: 15996618]
Level 3 (low-level) evidenceMenon B, Aggarwal B. Influence of spinal deformity on pulmonary function, arterial blood gas values, and exercise capacity in thoracic kyphoscoliosis. Neurosciences (Riyadh, Saudi Arabia). 2007 Oct:12(4):293-8 [PubMed PMID: 21857548]
Slattery C, Verma K. Classifications in Brief: The Lenke Classification for Adolescent Idiopathic Scoliosis. Clinical orthopaedics and related research. 2018 Nov:476(11):2271-2276. doi: 10.1097/CORR.0000000000000405. Epub [PubMed PMID: 30179943]
Banno T, Yamato Y, Hasegawa T, Yoshida G, Arima H, Oe S, Ide K, Yamada T, Kurosu K, Murakami Y, Matsuyama Y. Waistline Asymmetry Patterns and Clinical Impact in Patients with Adolescent Idiopathic Scoliosis. Spine. 2025 Apr 9:():. doi: 10.1097/BRS.0000000000005351. Epub 2025 Apr 9 [PubMed PMID: 40202283]
Villamor GA, Andras LM, Redding G, Chan P, Yang J, Skaggs DL. A Comparison of Maximal Voluntary Ventilation and Forced Vital Capacity in Adolescent Idiopathic Scoliosis Patients. Spine deformity. 2019 Sep:7(5):729-733. doi: 10.1016/j.jspd.2019.02.007. Epub [PubMed PMID: 31495472]
Augustine DX, Coates-Bradshaw LD, Willis J, Harkness A, Ring L, Grapsa J, Coghlan G, Kaye N, Oxborough D, Robinson S, Sandoval J, Rana BS, Siva A, Nihoyannopoulos P, Howard LS, Fox K, Bhattacharyya S, Sharma V, Steeds RP, Mathew T. Echocardiographic assessment of pulmonary hypertension: a guideline protocol from the British Society of Echocardiography. Echo research and practice. 2018 Sep:5(3):G11-G24. doi: 10.1530/ERP-17-0071. Epub [PubMed PMID: 30012832]
Huang SW, Wu CL, Lin CC, Hung CL, Kuo LK, Weng YL, Lee SY. Effect of long term intermittent nocturnal non-invasive positive pressure ventilation on patient with severe kyphoscoliosis and hypoxaemia. BMJ case reports. 2009:2009():. pii: bcr08.2008.0737. doi: 10.1136/bcr.08.2008.0737. Epub 2009 Mar 5 [PubMed PMID: 21686653]
Level 3 (low-level) evidenceTellermann J, Sablinskis M, Machado PRR, Sablinskis K, Skride A. Long-Term Response to Vasoactive Treatment in a Case of Kyphoscoliosis-Associated Pulmonary Hypertension. The American journal of case reports. 2019 Oct 13:20():1505-1508. doi: 10.12659/AJCR.917154. Epub 2019 Oct 13 [PubMed PMID: 31606732]
Level 3 (low-level) evidenceKarimi MT, Rabczuk T. Scoliosis conservative treatment: A review of literature. Journal of craniovertebral junction & spine. 2018 Jan-Mar:9(1):3-8. doi: 10.4103/jcvjs.JCVJS_39_17. Epub [PubMed PMID: 29755230]
Weiss HR, Tournavitis N, Nan X, Borysov M, Paul L. Workflow of CAD / CAM Scoliosis Brace Adjustment in Preparation Using 3D Printing. The open medical informatics journal. 2017:11():44-51. doi: 10.2174/1874431101711010044. Epub 2017 Oct 24 [PubMed PMID: 29204227]
Kim H, Chang SY, Chang BS, Lee JY, Jang S, Kim ST. The Efficacy of a Novel Hybrid Brace in the Treatment of Adolescent Idiopathic Scoliosis: A Prospective Case-Series Study. Children (Basel, Switzerland). 2025 Mar 5:12(3):. doi: 10.3390/children12030328. Epub 2025 Mar 5 [PubMed PMID: 40150610]
Level 3 (low-level) evidenceGonzález-Gálvez N, Gea-García GM, Marcos-Pardo PJ. Effects of exercise programs on kyphosis and lordosis angle: A systematic review and meta-analysis. PloS one. 2019:14(4):e0216180. doi: 10.1371/journal.pone.0216180. Epub 2019 Apr 29 [PubMed PMID: 31034509]
Level 1 (high-level) evidenceFeng Q, Wang M, Zhang Y, Zhou Y. The effect of a corrective functional exercise program on postural thoracic kyphosis in teenagers: a randomized controlled trial. Clinical rehabilitation. 2018 Jan:32(1):48-56. doi: 10.1177/0269215517714591. Epub 2017 Jun 14 [PubMed PMID: 28610442]
Level 1 (high-level) evidenceAtallah J, Armah FA, Wong D, Weis PA, Fahy BG. Use of spinal cord stimulator for treatment of lumbar radiculopathy in a patient with severe kyphoscoliosis. Pain physician. 2008 Jul-Aug:11(4):555-9 [PubMed PMID: 18690284]
Level 3 (low-level) evidenceMoens M, De Smedt A, Goudman L, Mariën P, Nijs J, Herregodts P, Brouns R. HF10 Therapy for Chronic Back Pain in Patients with Nonoperated Kyphoscoliosis: The Importance of Preoperative Assessment. Pain medicine (Malden, Mass.). 2017 Feb 1:18(2):392-294. doi: 10.1093/pm/pnw205. Epub [PubMed PMID: 28204731]
Lee M, Huntoon EA, Sinaki M. Soft Tissue and Bony Injuries Attributed to the Practice of Yoga: A Biomechanical Analysis and Implications for Management. Mayo Clinic proceedings. 2019 Mar:94(3):424-431. doi: 10.1016/j.mayocp.2018.09.024. Epub 2019 Feb 18 [PubMed PMID: 30792066]
Yaman O, Dalbayrak S. Idiopathic scoliosis. Turkish neurosurgery. 2014:24(5):646-57. doi: 10.5137/1019-5149.JTN.8838-13.0. Epub [PubMed PMID: 25269032]
Leng Y, Yin F, Yi Y, Zhao D, Liang Y. Treatment for paraplegia due to severe kyphoscoliosis associated with neurofibromatosis type 1 via halo-pelvic traction: a case report. Journal of medical case reports. 2025 May 19:19(1):235. doi: 10.1186/s13256-025-05293-0. Epub 2025 May 19 [PubMed PMID: 40390097]
Level 3 (low-level) evidenceThaler M, Gabl M, Lechner R, Gstöttner M, Bach CM. Severe kyphoscoliosis after primary Echinococcus granulosus infection of the spine. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2010 Sep:19(9):1415-22. doi: 10.1007/s00586-010-1398-6. Epub 2010 Jun 1 [PubMed PMID: 20514501]
Level 3 (low-level) evidenceTunçay E, Güngör S, Ertam BN, Ocaklı B, Aksoy E, Yazıcıoğlu Moçin Ö, Güngor G, Adıgüzel N, Karakurt Z. The Impact of Comorbidities and Intensive Care Unit (ICU) Admissions on Survival in Kyphoscoliosis-Related Respiratory Failure: A Retrospective Cohort Study. Journal of clinical medicine. 2025 May 17:14(10):. doi: 10.3390/jcm14103516. Epub 2025 May 17 [PubMed PMID: 40429511]
Level 2 (mid-level) evidence