Introduction
Creutzfeldt-Jakob disease (CJD) is a rapidly progressive, rare, transmissible, and uniformly fatal neurodegenerative condition caused by prion proteins.[1] This condition has a long incubation period.[2][3] CJD was first described in 1920 by Hans Creutzfeldt and later in 1921 and 1923 by Alfons Jakob. Later, Clearance J. Gibbs began using the term "Creutzfeldt-Jakob disease" because the acronym "CJD" was similar to his initials.[4][5]
CJD primarily affects the central nervous system (CNS). The primary functional unit of the CNS is the neuron, a unique cell type that can receive, store, and transmit information. CNS neurons do not regenerate, although some regions of the brain can heal to a limited extent due to the presence of stem cells. Attributes that make the CNS unique from other organ systems include the following:
- Cerebral blood flow autoregulation
- Having the cranium for bony protection
- Unique metabolic substrate requirements
- Absence of a true lymphatic system
- Cerebrospinal fluid (CSF) circulation
- Minimal immunologic surveillance
- Distinct injury response and tissue repair mechanisms
Neurons in the brain are topographically organized, with functional domains existing in anatomically defined regions. For example, the cerebral cortex controls voluntary movements, while the hypothalamus plays a significant role in autonomic responses. The somatotopic organization of brain cells enables various areas of the body to receive sensory and motor input from the CNS, which is beneficial in localizing neurological lesions.
Neurons differ in structure and size. Synapses are formed by axons and dendrites that greatly differ in number from cell to cell. Nissl bodies, which also vary in number, play a crucial role in the synthesis of nerve cell proteins and neurotransmitters. Neurofilaments maintain the cytoskeleton and play an essential role in nerve conduction.
Glia are cells that support the neurons. They include the following:
- Astrocytes are star-shaped glial cells that supply nutrients to the neurons, act as nerve detoxifiers, provide protection from harmful macromolecules, and contribute to CNS repair and scar formation.
- Oligodendrocytes myelinate the CNS axons.
- Ependymal cells line the ventricles and control CSF production and flow.
- Microglia comprise the macrophage system of the CNS.
CJD neuronal inclusions damage brain neurons, manifesting with nonspecific prodromal symptoms early in the disease course and neurologic changes, such as myoclonus, in the later, advanced stages.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
A prion protein (PrP) is a normal neuron protein with a predominantly α-helical and random coil composition. Proteinaceous infectious particles known as "prions" are self-propagating proteins lacking nucleic acids and are primarily comprised of proteinase K-resistant β-pleated sheet aggregates. Prions reproduce by associating with normal PrP cellular isoforms, converting α-helices into indigestible β-pleated sheets. These particles cause CJD and other transmissible spongiform encephalopathies, such as bovine spongiform encephalopathy (also known as mad cow disease), kuru, and scrapie.
CJD can be classified based on the mode of transmission. Sporadic CJD is the most common type of the disease (∼85%) and is due to misfolding of normal PrP isoforms with no apparent triggers. Subtypes of sporadic CJD include sporadic fatal insomnia and variably protease-sensitive prionopathy. Genetic CJD is the second most common type (∼10-15%) and arises from a heritable genetic mutation. Subtypes of this condition include familial CJD, fatal familial insomnia, and Gerstmann-Sträussler-Scheinker syndrome.
Infectious CJD accounts for less than 1% of cases and results from the transmission of prions through an external source. Subtypes include kuru, iatrogenic CJD, and variant CJD. Kuru is a disease of the FORE people of Papua New Guinea who consumed the brains of dead relatives as part of ritualistic cannibalism before the practice was banned in the 1950s. Iatrogenic CJD arises from inadvertent prion inoculation during surgical procedures or through blood transfusion.[6] Variant CJD is associated with the ingestion of infected beef by a mechanism similar to the development of bovine spongiform encephalopathy. Most documented cases of variant CJD have occurred in the United Kingdom and France.[7][8][9]
Epidemiology
CJD affects about 1 individual per million per year worldwide. Approximately 350 cases are diagnosed annually in the United States. Sporadic CJD is the most common form of human prion disease. The condition has a mean age of onset of 62 years, although it has also been reported in younger and older age groups.[10][11] Sporadic CJD has a 1:1 male-to-female ratio. Approximately 1 to 2 new sporadic CJD cases occur per 1,000,000 individuals worldwide each year.[12] Death occurs in nearly 70% of patients within a year of onset. The mean survival of sporadic CJD is 4 to 8 months, with 90% of patients dying within a year.
Genetic CJD is the second most common type of this condition. Patients often have a family history of the disease and mutations in the autosomal-dominant PRNP gene. Acquired cases are rare, occurring in less than 1% of cases, and typically affect young adults with a mean age of 29 years.
Pathophysiology
Normal cellular prion protein (PrPc) transforms into the disease-causing form PrP scrapie (PrPSc) either spontaneously or as a result of PrPSc infection. PrPSc self-propagates and accumulates throughout the brain. The highly chemically stable β-pleated aggregates cause derangements in intracellular protein folding, ubiquitination, and trafficking in affected neurons. Additionally, astrocytes may swell and degrade in reaction to prion-induced injury. Neurodegeneration results from these changes.[13]
Histopathology
Gross pathological examination of affected brains may not reveal any abnormalities. However, the following features are commonly observed during light microscopy (see Image. Neuropathological Confirmation of Creutzfeldt-Jacob Disease):
- Vacuolation or spongiform degeneration, most notably in the cerebral cortex, caudate nucleus, thalamus, putamen, and the molecular layer of the cerebellum
- Neuronal loss
- Astrocytic gliosis or fibrous proliferation of the astrocytes, primarily in the gray matter
Amyloid plaques can be found in some individuals.
History and Physical
CJD presents in variable ways, depending on the subtype. The manifestations arise from the involvement of various parts of the CNS. The table below summarizes the symptoms that may manifest in patients with CJD.
Table. Symptoms of Creutzfeldt-Jakob Disease
| Neuropsychiatric symptoms: |
|
Involuntary movements:
|
Cerebellar manifestations:[18]
|
Signs related to the corticospinal tract:
|
Atypical features include cranial nerve abnormalities, peripheral nervous system involvement, and vestibulocochlear dysfunction. Although found rarely in association with CJD, these manifestations should raise suspicion of another potential diagnosis. The neurologic examination must be as detailed as possible for all patients suspected of CJD.
Sporadic CJD
In the early stages of sporadic CJD, patients may develop nonspecific symptoms like vertigo, headache, fatigue, and sleep disorders. However, memory problems, agitation, irritability, depression, apathy, mood swings, and sensory changes such as visual loss can also occur. As the disease progresses, patients may develop rapidly worsening confusion, disorientation, and cognitive problems. Most patients display coordination and movement abnormalities, including ataxia, involuntary jerky movements, myoclonus, muscle stiffness, and involuntary muscle twitching. Myoclonus persists during sleep and may be elicited by loud sounds or bright lights.
Extrapyramidal symptoms can include bradykinesia, dystonia, and rigidity. Patients gradually lose mobility, the ability to speak, and progress into a comatose state. Certain infections, such as pneumonia, can be fatal.
Patients with sporadic CJD are typically between 55 and 75 years of age. Death occurs within a year of onset, with the median duration of illness being 4 to 5 months. The median age of death in individuals with sporadic CJD is 68 years. Sporadic CJD is similar to dementia in its presentation, but progresses much more rapidly.
CJD subtyping is based on genetic polymorphism, prion protein characteristics, and the associated symptoms. Methionine/methionine type 1 (MM1) and methionine/valine type 1 (MV1) comprise 70% of cases and correlate with the classic CJD phenotype. The condition has a mid- to late-life onset and presents with rapidly progressive dementia (RPD) and early myoclonus and ataxia.
Methionine/valine type 2 (MV2) is the kuru plaque variant, accounting for approximately 10% of sporadic CJD cases. The condition presents with progressive dementia with prominent psychiatric features and has a longer duration of approximately 17 months.[19] The valine/valine type 2 (VV2) variant is also known as the ataxic variant. This condition presents with ataxia at the onset or as an isolated feature. The VV2 subtype has a duration of illness of around 7 to 9 months.[20]
The methionine/methionine type 2 (MM2) subtype may be classified as either thalamic or cortical. The thalamic MM2 subtype is also known as sporadic fatal insomnia and is present in 2% of cases. The mean disease duration is 15.6 months. The most frequent symptoms include psychomotor hyperactivity, ataxia, insomnia, and cognitive impairment, resembling fatal familial insomnia.[21] The cortical MM2 subtype also comprises 2% of sporadic CJD cases. Dementia is the predominant clinical manifestation of this subtype. The average disease duration is 15.7 months. Visual and cerebellar signs are rarely described at presentation.[22]
The valine/valine 1 (VV1) subtype accounts for 1% of cases and typically has a younger age of onset. Individuals with this condition present with progressive dementia. The VV1 subtype has an average duration of 15.3 months.[23]
Inherited CJD
Genetic CJD has phenotypic variability that may be attributed to the low penetrance of PRNP mutations. Patients with genetic CJD are usually younger than individuals with sporadic CJD, manifesting behavioral and cognitive changes initially, and incoordination and movement abnormalities over the next few months. A family history of similar neurologic manifestations may be elicited.
Inherited CJD is fatal, though the duration of illness varies among individuals. For example, Gerstmann–Straussler–Scheinker syndrome has a slow progression, and death may be delayed for up to 10 years.[32]
Variant CJD
Patients with variant CJD are often younger than patients with sporadic CJD, initially presenting with psychiatric symptoms, behavioral changes, and painful dysesthesias. Movement disorders may develop early, but dementia is usually a late sign. A history of having a neurosurgical procedure or ingestion of infected meat may be elicited. The median duration of illness is between 13 and 14 months, while the median age at death is 28 years.
Evaluation
Creutzfeldt-Jakob disease is often a diagnostic challenge as it presents similarly to other conditions presenting with rapidly progressive dementia (RPD). The following are the recommended initial screening tests for evaluating RPD:
- Complete blood count
- Complete metabolic panel
- Blood magnesium level
- Rapid plasma reagin
- Erythrocyte sedimentation rate
- Antinuclear antibody
- C-reactive protein
- Thyroid function tests
- Vitamin B12 level
- HIV test
- Lyme disease titer
- Autoimmune antibodies
- Urinalysis
- CSF studies, including glucose, oligoclonal bands, and cell count with differential
- CSF 14-3-3 protein (a specific test for prion disease)
- Venereal disease research laboratory (VDRL) test
Among imaging studies, computed tomography (CT) may be ordered initially. However, brain magnetic resonance imaging (MRI) with or without contrast, along with related modalities such as fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted imaging (DWI), can provide more detailed information about the involved regions. CJD may be diagnosed when imaging is combined with clinical, laboratory, and electroencephalogram (EEG) findings.[24][25][26]
The World Health Organization published diagnostic criteria for CJD in 1998, which relied on the clinical, EEG, and CSF findings. However, advanced diagnostic procedures, such as MRI and genetic testing, have rendered those criteria obsolete.
Brain MRI is a more sensitive and specific test for variant CJD than the CSF 14–3–3 protein and was found to be accurate in about 90% of cases (see Image. Brain MRI of a Patient with Early-Stage Creutzfeldt-Jakob Disease).[27] Brain MRI with T2-weighted scanning, DWI, and apparent diffusion coefficient (ADC) sequences can often reveal abnormalities in the cortical gray matter, like cortical ribboning, and in the deep nuclei in sporadic CJD. MRI with DWI or FLAIR imaging has a sensitivity of 98% and specificity of 93%. DWI typically demonstrates hyperintensities within the basal ganglia, thalamus, and cortex. The "hockey stick" or "pulvinar" sign indicates variant, infectious, or acquired CJD, although it is also seen in other forms of CJD. CSF 14-3-3 can be more sensitive for CJD than other prion diseases when combined with the typical EEG findings.
CSF protein biomarkers, including the 14–3–3 protein, total tau (T-tau), and neuron-specific enolase (NSE), are markers of rapid neurodegeneration. While these tests can support the diagnosis of CJD, they are not specific to the disease. An elevated tau level (greater than 1150 picograms/mL) has greater accuracy and specificity than the 14-3-3 protein as a diagnostic test for CJD, although both tests can produce significant false-negative and false-positive results.[28]
In 2012, the American Academy of Neurology recommended ordering CSF 14-3-3 only when CJD is strongly suspected. A recent comparison of these non-prion-specific CSF biomarkers with MRI revealed that DWI had a diagnostic accuracy of 97%, surpassing that of the T-tau (79.6%), 14-3-3 protein (70.4%), and NSE (71.4%) tests. Detection of these traditional surrogate marker proteins is accurate in approximately three-fourths of cases. Routine CSF analysis, which includes glucose, total protein, white blood cell count, total cell count, and oligoclonal IgG, is generally unremarkable in CJD patients.
The National Prion Disease Pathology Surveillance Center launched a new diagnostic test in April 2015 called "second-generation Real Time-Quaking-Induced Conversion (RT-QuIC)," which is highly sensitive and specific for CJD. RT-QuIC can accurately detect pathogenic prion protein in the CSF of patients with CJD. RT-QuIC directly detects the pathogenic prion protein, in contrast to the 14-3-3 protein, T-tau, and NSE, which are indirect tests.
Several studies have revealed that RT-QuIC exhibits modest sensitivity (greater than 80%) but high specificity (approximately 98%) for sporadic CJD.[29] Most patients with the VV2 sporadic CJD subtype have negative CSF RT-QuIC tests. Although it is not as sensitive as MRI, RT-QuIC is often positive in many forms of genetic prion disease, some of which lack the classic MRI findings of sporadic CJD.
RT-QuIC may be more sensitive using olfactory epithelium brushings as a specimen rather than CSF. Recent studies have shown that RT-QuIC is comparable to brain biopsy in terms of accuracy in diagnosing CJD.[30] RT-QulC is less invasive compared to brain biopsy. However, the existing CJD guidelines do not include newer, less invasive diagnostic modalities.
EEG is not as sensitive as brain MRI or CSF studies in detecting CJD; however, the typical findings associated with the condition in its late stages include periodic sharp wave complexes (PSWCs). Bi- or triphasic PSWC is found in 67% to 95% of patients with sporadic CJD. This finding is considered supportive rather than diagnostic and is characterized by the following features:
- Generalized or lateralized complexes
- A minimum of 5 repetitive intervals with a duration difference of less than 500 milliseconds to exclude semiperiodic activity
- Strictly periodic cerebral potentials, the majority with an intercomplex interval of 500 to 2000 milliseconds and a duration of 100 to 600 milliseconds
Among patients with sporadic CJD, the MM1 and MV2 subtypes frequently manifest with PSWCs, while the MV2 subtype exhibits PSWCs infrequently. PSWCs are not found in patients with Gerstmann-Sträussler-Scheinker syndrome, variant CJD, kuru, or fatal familial insomnia. PSWCs are occasionally observed in patients with genetic CJD, particularly in those with the codon 200 mutation.[31]
Brain tissue biopsy or postmortem examination of the brain confirms the diagnosis of CJD. However, not all areas of the brain are affected by the disease. Imaging studies should target subcortical structures, where abnormal features are most likely to be found. Surgery has inherent risks and may not always be able to access the area of involved brain tissue. CJD confirmation does not alter the clinical outcome of the patient. Therefore, a brain biopsy is only indicated when a reversible condition is suspected in the differential diagnosis.
Prions have been detected in the blood and urine of patients with symptomatic variant CJD. Caution should be exercised when handling body fluids and tissues from patients with variant CJD until prion infectivity has been excluded.
Treatment / Management
CJD has no definitive treatment, and supportive care is the mainstay of clinical management.[32] Most trial drugs for CJD have not demonstrated any clear benefit to date. However, intraventricular pentosan polysulfate has been shown in rodent studies to inhibit PrPSc formation. An apparent survival extension of 37 to 114 months was observed in four patients.[33] More research is needed to find a cure for this fatal condition.(A1)
Early detection of a PRNP mutation may help families at risk for the genetic form of CJD. Patients affected by the condition can make earlier arrangements for end-of-life planning. Psychosocial support and supportive care may improve patients' quality of life. Genetic counseling and family planning help prevent the transmission of disease to the offspring of individuals with the PRNP mutation.
Differential Diagnosis
Rapidly progressive dementia (RPD) has a broad differential diagnosis that includes vascular, neurodegenerative, autoimmune, infectious, thromboembolic, neoplastic, iatrogenic, and toxic metabolic conditions. Vascular conditions like stroke, multiple infarcts, cerebral amyloid angiopathy, or hypertensive encephalopathy can likewise lead to RPD. Vasculitis and intravascular lymphoma may also manifest as RPD.
These conditions may be distinguished from CJD by a thorough medical evaluation. Imaging studies can help exclude vascular and neoplastic causes of RPD. Blood and CSF examinations can detect autoimmune, infectious, metabolic, and neurodegenerative conditions.[34][35]
Prognosis
The prognosis for CJD is extremely poor despite all the advances that have helped to understand this disease. The condition is invariably fatal. Death occurs within one year of symptom onset, except in some rare cases.
Complications
CJD's complications encompass both physical and psychosocial difficulties. Individuals affected by CJD often withdraw from friends and family and ultimately lose their ability to recognize or relate to them. Patients also lose their capacity for self-care and often gradually progress into a coma. CJD has a 100% fatality rate.
Deterrence and Patient Education
CJD is a progressive, fatal disease. Fortunately, very few cases are reported in the USA, so the risk of contracting the disease is extremely low. Strategies focus on prevention, with blood centers prohibiting first-degree relatives of individuals with CJD from donating blood. Hunters who plan to consume or handle elk or deer meat should consider having the meat tested for safety before consumption. Families at risk for the genetic type of CJD may practice contraception to prevent disease transmission to their offspring.
Pearls and Other Issues
The most important points to remember when managing CJD are the following:
- CJD is an invariably fatal prion disease.
- The condition presents in variable forms, but cases are generally classified as either sporadic, genetic, or infectious.
- CJD's manifestations are primarily neurologic, with dementia, myoclonus, and EEG PSWCs being the most common features.
- Supportive treatment and psychosocial care are the cornerstones of CJD management.
- Early detection does not alter the disease course, though it can improve the quality of life and prevent disease transmission in families with the genetic subtype.
- Diagnosis is possible when clinical evaluation is combined with blood and CSF testing, imaging, and EEG.[36]
Prion diseases like CJD should be considered when evaluating patients with RPD.
Enhancing Healthcare Team Outcomes
The management of CJD requires an interdisciplinary approach due to its complex nature and widespread impact on patient health. The interprofessional team may include the following members:
- Neurologists diagnose and manage the condition and counsel patients and families about how CJD affects brain function.
- Neurosurgeons may perform neurosurgical procedures for diagnosis and symptom management in patients with CJD.
- Infectious disease specialists may contribute their expertise in managing prion transmission and implementing infection control measures.
- Intensivists provide treatment to CJD patients requiring intensive care.
- Mental health practitioners provide emotional and psychological support to patients with CJD and their families, helping them to cope with the mental health challenges associated with the disease.
- Neuroradiologists lend their expertise in interpreting imaging studies, aiding in the diagnosis of CJD and monitoring the progression of brain changes on imaging.
- Pathologists examine brain tissue samples to confirm the diagnosis of CJD
- Nurses provide direct patient care, administer treatments, monitor symptoms, and support patients and families. Nurses often serve as a crucial link between the healthcare team, patients, and their families.
- The rehabilitation team, including physical and occupational therapists, helps manage symptoms and maintain functional abilities.
- Speech-language pathologists assist in managing communication difficulties that can arise due to CJD-related neurological changes.
- Palliative care specialists provide symptom management, pain relief, and support to patients with CJD and families facing end-of-life care. These providers focus on improving the quality of life for patients with CJD.
- Social workers assist the treatment team in coordinating care. These professionals also aid patients and their families in accessing care and navigating the challenges associated with CJD.
- Genetic counselors provide information, support, and counseling about familial risks and genetic testing to patients at risk for the inherited type of CJD.
Collaboration among team members is vital for rendering the best care to individuals affected by CJD.
Most patients with CJD die within a year of the onset of symptoms. Preparations for hospice care should be addressed early. Counseling for the family is essential because the condition has no effective cure, and death is inevitable.
Media
(Click Image to Enlarge)
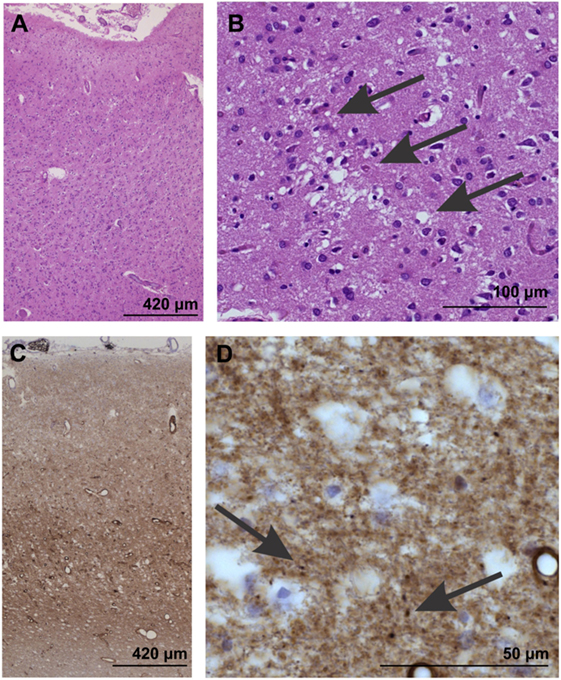
Neuropathological Confirmation of Creutzfeldt-Jakob Disease. Neuropathological confirmation of Creutzfeldt-Jacob disease morphologically by neuron loss and astrogliosis in the temporal neocortex (area 35) as evident in the overview magnification of a hematoxylin and eosin-stained section (A). Spongiform changes become visible at higher magnification [arrows in (B)]. (C, D) In the temporal neocortex of Brodmann area 35, the synaptic pattern. of the pathological prion protein deposits becomes evident (C). At higher magnification (D), some more condensed, dot-like deposits can be seen (arrows), whereas no plaques or plaque-like lesions were seen. Prion protein antibody used: 3F4, proteinase K, and formic acid pretreatment, 1/100.
Wiels WA, Du Four S, Seynaeve L, et al. Early-onset Creutzfeldt-Jakob disease mimicking immune-mediated encephalitis. Front Neurol. 2018;10:9:242. doi: 10.3389/fneur.2018.00242.
(Click Image to Enlarge)
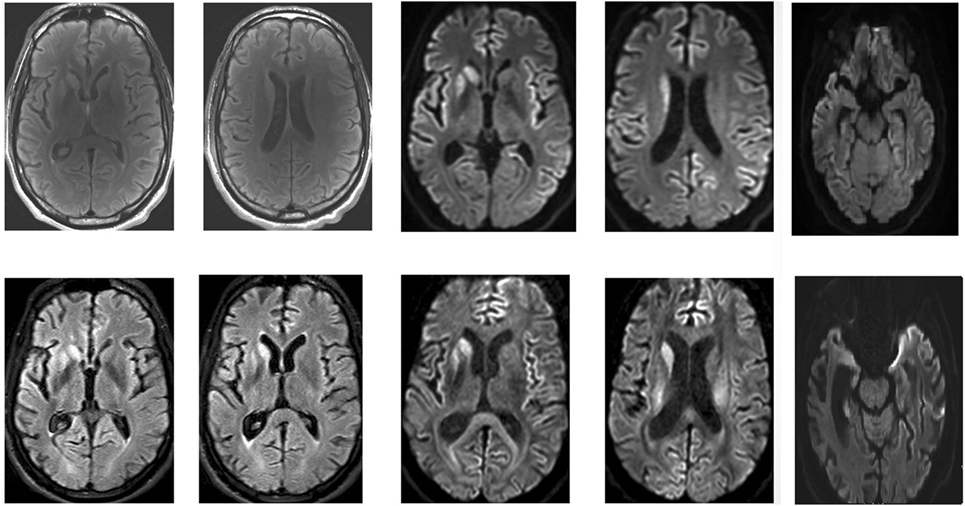
Brain MRI of a Patient With Early-Stage Creutzfeldt-Jakob Disease. Top: April 2016. Bottom: May 2016. Asymmetric T2, fluid-attenuation inversion recovery, and diffusion-weighted hyperintensities in the putamen and caudate. Frontal and temporal cortical regions of restricted diffusion are clearly visible.
Wiels WA, Du Four S, Seynaeve L, et al. Early-onset Creutzfeldt-Jakob disease mimicking immune-mediated encephalitis. Front. Neurol. 2018;10:9:242. doi: 10.3389/fneur.2018.00242.
References
Zerr I, Ladogana A, Mead S, Hermann P, Forloni G, Appleby BS. Creutzfeldt-Jakob disease and other prion diseases. Nature reviews. Disease primers. 2024 Feb 29:10(1):14. doi: 10.1038/s41572-024-00497-y. Epub 2024 Feb 29 [PubMed PMID: 38424082]
Ishibashi D, Homma T, Nakagaki T, Fuse T, Sano K, Satoh K, Mori T, Atarashi R, Nishida N. Type I interferon protects neurons from prions in in vivo models. Brain : a journal of neurology. 2019 Apr 1:142(4):1035-1050. doi: 10.1093/brain/awz016. Epub [PubMed PMID: 30753318]
Gao LP, Shi Q, Xiao K, Wang J, Zhou W, Chen C, Dong XP. The genetic Creutzfeldt-Jakob disease with E200K mutation: analysis of clinical, genetic and laboratory features of 30 Chinese patients. Scientific reports. 2019 Feb 12:9(1):1836. doi: 10.1038/s41598-019-38520-y. Epub 2019 Feb 12 [PubMed PMID: 30755683]
Navid J, Day GS, Strain J, Perrin RJ, Bucelli RC, Dincer A, Wisch JK, Soleimani-Meigooni D, Morris JC, Benzinger TLS, Ances BM. Structural signature of sporadic Creutzfeldt-Jakob disease. European journal of neurology. 2019 Aug:26(8):1037-1043. doi: 10.1111/ene.13930. Epub 2019 Mar 25 [PubMed PMID: 30735286]
Aslam S, Fritz MA, Cordes L, Sabbagh MN. What Promises the CJD Diagnosis in a Case of Rapidly Progressive Dementia? Journal of Alzheimer's disease & Parkinsonism. 2018:8(5):. pii: 452. doi: 10.4172/2161-0460.1000452. Epub 2018 Oct 30 [PubMed PMID: 30733890]
Level 3 (low-level) evidencePozzo di Borgo A, Rochette S, Gaussen A, O'Brien SF, Germain M, Renaud C, Lewin A. Transmission of Variant Creutzfeldt-Jakob Disease Through Blood Transfusion and Plasma-Derived Products: A Narrative Review of Observed and Modeled Risks. Transfusion medicine reviews. 2023 Jul:37(3):150747. doi: 10.1016/j.tmrv.2023.150747. Epub 2023 Jun 16 [PubMed PMID: 37827587]
Level 3 (low-level) evidenceDuyckaerts C, Clavaguera F, Potier MC. The prion-like propagation hypothesis in Alzheimer's and Parkinson's disease. Current opinion in neurology. 2019 Apr:32(2):266-271. doi: 10.1097/WCO.0000000000000672. Epub [PubMed PMID: 30724769]
Level 3 (low-level) evidenceHayashi Y. Pathological and/or clinical work-up are required in atypical Creutzfeldt-Jakob disease cases with periodic lateralised epileptiform discharge. Psychogeriatrics : the official journal of the Japanese Psychogeriatric Society. 2019 Sep:19(5):519-520. doi: 10.1111/psyg.12411. Epub 2019 Feb 5 [PubMed PMID: 30723966]
Level 3 (low-level) evidenceMugilan SR, Joseph JP. A case of probable sporadic Creutzfeldt-Jacob Disease in a tertiary care hospital in Malaysia. The Medical journal of Malaysia. 2018 Dec:73(6):433-435 [PubMed PMID: 30647225]
Level 3 (low-level) evidenceJohnson RT, Gonzalez RG, Frosch MP. Case records of the Massachusetts General Hospital. Case 27-2005. An 80-year-old man with fatigue, unsteady gait, and confusion. The New England journal of medicine. 2005 Sep 8:353(10):1042-50 [PubMed PMID: 16148290]
Level 3 (low-level) evidenceLadogana A, Puopolo M, Croes EA, Budka H, Jarius C, Collins S, Klug GM, Sutcliffe T, Giulivi A, Alperovitch A, Delasnerie-Laupretre N, Brandel JP, Poser S, Kretzschmar H, Rietveld I, Mitrova E, Cuesta Jde P, Martinez-Martin P, Glatzel M, Aguzzi A, Knight R, Ward H, Pocchiari M, van Duijn CM, Will RG, Zerr I. Mortality from Creutzfeldt-Jakob disease and related disorders in Europe, Australia, and Canada. Neurology. 2005 May 10:64(9):1586-91 [PubMed PMID: 15883321]
Klug GM, Wand H, Simpson M, Boyd A, Law M, Masters CL, Matěj R, Howley R, Farrell M, Breithaupt M, Zerr I, van Duijn C, Ibrahim-Verbaas C, Mackenzie J, Will RG, Brandel JP, Alperovitch A, Budka H, Kovacs GG, Jansen GH, Coulthard M, Collins SJ. Intensity of human prion disease surveillance predicts observed disease incidence. Journal of neurology, neurosurgery, and psychiatry. 2013 Dec:84(12):1372-7. doi: 10.1136/jnnp-2012-304820. Epub 2013 Aug 21 [PubMed PMID: 23965290]
Level 2 (mid-level) evidenceBrandel JP. [Prion diseases or transmissible spongiform encephalopathies]. La Revue de medecine interne. 2022 Feb:43(2):106-115. doi: 10.1016/j.revmed.2021.05.002. Epub 2021 Jun 18 [PubMed PMID: 34148672]
Krasnianski A, Bohling GT, Heinemann U, Varges D, Meissner B, Schulz-Schaeffer WJ, Reif A, Zerr I. Neuropsychological Symptoms in Sporadic Creutzfeldt-Jakob Disease Patients in Germany. Journal of Alzheimer's disease : JAD. 2017:59(1):329-337. doi: 10.3233/JAD-161129. Epub [PubMed PMID: 28598840]
Krasnianski A, Bohling GT, Harden M, Zerr I. Psychiatric symptoms in patients with sporadic Creutzfeldt-Jakob disease in Germany. The Journal of clinical psychiatry. 2015 Sep:76(9):1209-15. doi: 10.4088/JCP.13m08915. Epub [PubMed PMID: 25938948]
Landolt HP, Glatzel M, Blättler T, Achermann P, Roth C, Mathis J, Weis J, Tobler I, Aguzzi A, Bassetti CL. Sleep-wake disturbances in sporadic Creutzfeldt-Jakob disease. Neurology. 2006 May 9:66(9):1418-24 [PubMed PMID: 16682677]
Thompson A, MacKay A, Rudge P, Lukic A, Porter MC, Lowe J, Collinge J, Mead S. Behavioral and psychiatric symptoms in prion disease. The American journal of psychiatry. 2014 Mar:171(3):265-74. doi: 10.1176/appi.ajp.2013.12111460. Epub [PubMed PMID: 24585329]
Rabinovici GD, Wang PN, Levin J, Cook L, Pravdin M, Davis J, DeArmond SJ, Barbaro NM, Martindale J, Miller BL, Geschwind MD. First symptom in sporadic Creutzfeldt-Jakob disease. Neurology. 2006 Jan 24:66(2):286-7 [PubMed PMID: 16434680]
Collins SJ, Sanchez-Juan P, Masters CL, Klug GM, van Duijn C, Poleggi A, Pocchiari M, Almonti S, Cuadrado-Corrales N, de Pedro-Cuesta J, Budka H, Gelpi E, Glatzel M, Tolnay M, Hewer E, Zerr I, Heinemann U, Kretszchmar HA, Jansen GH, Olsen E, Mitrova E, Alpérovitch A, Brandel JP, Mackenzie J, Murray K, Will RG. Determinants of diagnostic investigation sensitivities across the clinical spectrum of sporadic Creutzfeldt-Jakob disease. Brain : a journal of neurology. 2006 Sep:129(Pt 9):2278-87 [PubMed PMID: 16816392]
Cooper SA, Murray KL, Heath CA, Will RG, Knight RS. Sporadic Creutzfeldt-Jakob disease with cerebellar ataxia at onset in the UK. Journal of neurology, neurosurgery, and psychiatry. 2006 Nov:77(11):1273-5 [PubMed PMID: 16835290]
Level 2 (mid-level) evidenceParchi P, Capellari S, Chin S, Schwarz HB, Schecter NP, Butts JD, Hudkins P, Burns DK, Powers JM, Gambetti P. A subtype of sporadic prion disease mimicking fatal familial insomnia. Neurology. 1999 Jun 10:52(9):1757-63 [PubMed PMID: 10371520]
Level 3 (low-level) evidenceNozaki I, Hamaguchi T, Noguchi-Shinohara M, Ono K, Shirasaki H, Komai K, Kitamoto T, Yamada M. The MM2-cortical form of sporadic Creutzfeldt-Jakob disease presenting with visual disturbance. Neurology. 2006 Aug 8:67(3):531-3 [PubMed PMID: 16894125]
Level 3 (low-level) evidenceRhoads DD, Wrona A, Foutz A, Blevins J, Glisic K, Person M, Maddox RA, Belay ED, Schonberger LB, Tatsuoka C, Cohen ML, Appleby BS. Diagnosis of prion diseases by RT-QuIC results in improved surveillance. Neurology. 2020 Aug 25:95(8):e1017-e1026. doi: 10.1212/WNL.0000000000010086. Epub 2020 Jun 22 [PubMed PMID: 32571851]
Li JSY, Lim KC, Lim WEH, Chen RC. Clinics in diagnostic imaging (193). Sporadic Creutzfeldt-Jakob disease (sCJD). Singapore medical journal. 2018 Dec:59(12):634-641. doi: 10.11622/smedj.2018146. Epub [PubMed PMID: 30631881]
Kolářová K, Marešová M, Manďáková Z, Kynčl J. Prion diseases with a focus on Creutzfeldt-Jakob disease, a summary of the incidence of Creutzfeldt-Jakob disease in the Czech Republic over the last 17 years, 2000-2017. Epidemiologie, mikrobiologie, imunologie : casopis Spolecnosti pro epidemiologii a mikrobiologii Ceske lekarske spolecnosti J.E. Purkyne. 2018 Winter:67(4):155-160 [PubMed PMID: 30630318]
Rudge P, Jaunmuktane Z, Hyare H, Ellis M, Koltzenburg M, Collinge J, Brandner S, Mead S. Early neurophysiological biomarkers and spinal cord pathology in inherited prion disease. Brain : a journal of neurology. 2019 Mar 1:142(3):760-770. doi: 10.1093/brain/awy358. Epub [PubMed PMID: 30698738]
Macfarlane RG, Wroe SJ, Collinge J, Yousry TA, Jäger HR. Neuroimaging findings in human prion disease. Journal of neurology, neurosurgery, and psychiatry. 2007 Jul:78(7):664-70 [PubMed PMID: 17135459]
Forner SA, Takada LT, Bettcher BM, Lobach IV, Tartaglia MC, Torres-Chae C, Haman A, Thai J, Vitali P, Neuhaus J, Bostrom A, Miller BL, Rosen HJ, Geschwind MD. Comparing CSF biomarkers and brain MRI in the diagnosis of sporadic Creutzfeldt-Jakob disease. Neurology. Clinical practice. 2015 Apr:5(2):116-125 [PubMed PMID: 26137420]
Hermann P, Appleby B, Brandel JP, Caughey B, Collins S, Geschwind MD, Green A, Haïk S, Kovacs GG, Ladogana A, Llorens F, Mead S, Nishida N, Pal S, Parchi P, Pocchiari M, Satoh K, Zanusso G, Zerr I. Biomarkers and diagnostic guidelines for sporadic Creutzfeldt-Jakob disease. The Lancet. Neurology. 2021 Mar:20(3):235-246. doi: 10.1016/S1474-4422(20)30477-4. Epub [PubMed PMID: 33609480]
Cazzaniga FA, Bistaffa E, De Luca CMG, Bufano G, Indaco A, Giaccone G, Moda F. Sporadic Creutzfeldt-Jakob disease: Real-Time Quaking Induced Conversion (RT-QuIC) assay represents a major diagnostic advance. European journal of histochemistry : EJH. 2021 Oct 15:65(s1):. doi: 10.4081/ejh.2021.3298. Epub 2021 Oct 15 [PubMed PMID: 34657408]
Brown P, Gibbs CJ Jr, Rodgers-Johnson P, Asher DM, Sulima MP, Bacote A, Goldfarb LG, Gajdusek DC. Human spongiform encephalopathy: the National Institutes of Health series of 300 cases of experimentally transmitted disease. Annals of neurology. 1994 May:35(5):513-29 [PubMed PMID: 8179297]
Level 3 (low-level) evidenceMiranda LHL, Oliveira AFPH, Carvalho DM, Souza GMF, Magalhães JGM, Júnior JAC, Lima PTMBQ, Júnior RMA, Filho SPL, Melo HMA. Systematic review of pharmacological management in Creutzfeldt-Jakob disease: no options so far? Arquivos de neuro-psiquiatria. 2022 Aug:80(8):837-844. doi: 10.1055/s-0042-1755341. Epub 2022 Oct 17 [PubMed PMID: 36252593]
Level 1 (high-level) evidenceTodd NV, Morrow J, Doh-ura K, Dealler S, O'Hare S, Farling P, Duddy M, Rainov NG. Cerebroventricular infusion of pentosan polysulphate in human variant Creutzfeldt-Jakob disease. The Journal of infection. 2005 Jun:50(5):394-6 [PubMed PMID: 15907546]
Level 3 (low-level) evidenceTavares-Júnior JWL, Carvalho RO, Feitosa RRP, Rolim FPS, Rocha FA, Pitombeira MS, Malveira GLS, de Carvalho JJF, Frota NAF, Dias DA. Diagnostic approach in a patient with Creutzfeldt-Jakob disease. Dementia & neuropsychologia. 2022 Jul-Sep:16(3):361-364. doi: 10.1590/1980-5764-DN-2021-0110. Epub 2022 May 23 [PubMed PMID: 36619848]
Noor H, Baqai MH, Naveed H, Naveed T, Rehman SS, Aslam MS, Lakdawala FM, Memon WA, Rani S, Khan H, Imran A, Farooqui SK. Creutzfeldt-Jakob disease: A comprehensive review of current understanding and research. Journal of the neurological sciences. 2024 Dec 15:467():123293. doi: 10.1016/j.jns.2024.123293. Epub 2024 Nov 12 [PubMed PMID: 39546829]
Level 3 (low-level) evidenceRyan R, Hill S, Lowe D, Allen K, Taylor M, Mead C. Notification and support for people exposed to the risk of Creutzfeldt-Jakob disease (CJD) (or other prion diseases) through medical treatment (iatrogenically). The Cochrane database of systematic reviews. 2011 Mar 16:(3):CD007578. doi: 10.1002/14651858.CD007578.pub2. Epub 2011 Mar 16 [PubMed PMID: 21412905]
Level 1 (high-level) evidence