Introduction
Intersection syndrome was first described in the literature by Alfred-Armand-Louis-Marie Velpeau, a French anatomist and surgeon, in 1841. However, the term was later officially coined by James H Dobyns at the Mayo Clinic in 1978. Although intersection syndrome is the commonly accepted term today, it has historically been described in the medical literature by other names, such as oarsman wrist, crossover syndrome, abductor pollicis longus bursitis, abductor pollicis longus syndrome, and peritendinitis crepitans.[1][2]
This condition affects the first and second compartments of the dorsal wrist extensors, which are part of a collective of 6 dorsal compartments that are variably responsible for wrist and digital extension. The specific compartments include (see Image. Dorsal Forearm Anatomy):
- First compartment: Abductor pollicis longus and extensor pollicis brevis
- Second compartment: Extensor carpi radialis longus and extensor carpi radialis brevis
- Third compartment: Extensor pollicis longus
- Fourth compartment: Extensor digitorum communis and extensor indicis proprius
- Fifth compartment: Extensor digiti minimi
- Sixth compartment: Extensor carpi ulnaris
The abductor pollicis longus and extensor pollicis brevis tendons of the first dorsal compartment of the wrist have a unique anatomical pathway where they cross over the extensor carpi radialis longus and extensor carpi radialis brevis of the second dorsal compartment proximal to the extensor retinaculum and radial styloid.[1][2][3] The inflammatory process and resulting tenosynovitis occur at this intersection, approximately 4 to 6 cm proximal to Lister tubercle along the dorso-radial distal forearm.[1][2][4] Although this is generally accepted as the underlying cause of intersection syndrome, researchers have also suggested that the condition may reflect pathology isolated to the second compartment (without contribution or involvement from the first dorsal compartment).[5]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Intersection syndrome typically results from repetitive wrist extension and flexion exercises or activities.[6] This repetitive motion is believed to cause friction at the intersection point of the first and second dorsal compartments, leading to localized inflammation and, ultimately, painful tenosynovitis.[7][8]
Epidemiology
This relatively rare syndrome has a purported incidence of less than 1 in 100,000 patients annually and is more commonly observed in athletes participating in activities such as rowing or canoeing, skiing, racquet sports, and horseback riding.[9][10] Studies have found no significant difference in injury patterns between men and women.[1][3][2]
Pathophysiology
In the dorsal forearm, the abductor pollicis longus and extensor pollicis brevis intercept the extensor carpi radialis brevis and extensor carpi radialis longus at approximately 60°.[11] Friction at this site between the muscle bellies of these first compartment structures and the tendons of the second compartment results from repetitive wrist flexion, extension, and, to a certain extent, pronation.[12] Over time, this friction creates a progressive inflammatory response that leads to tenosynovitis.
History and Physical
Clinical History of Intersection Syndrome
A careful and methodical approach to history-taking and physical examination can often lead to a diagnosis of intersection syndrome. Patients with this condition typically present with pain over the dorsal wrist and dorso-radial distal forearm; a history of repetitive wrist motion associated with work or recreational activities may also be present.
Physical Examination Findings of Intersection Syndrome
The physical examination should begin with a focused assessment of the elbow, forearm, and wrist.[1][2][13] As with all musculoskeletal examinations, clinicians must have a structured approach that includes inspection, range of motion, palpation, muscle testing, and other provocative tests. Each joint above and below the site of concern should be assessed.
The hallmark finding is tenderness to palpation along the dorso-radial distal forearm, approximately 4 to 6 cm proximal to Lister tubercle. Associated swelling may be noted at this site. In addition, crepitus at the distal forearm may be palpable with resisted wrist and thumb extension, another finding fairly specific to intersection syndrome.
De Quervain Tenosynovitis Versus Intersection Syndrome
The aforementioned clinical findings aid in differentiating intersection syndrome from de Quervain tenosynovitis, a more common tenosynovitis of the first dorsal compartment, which presents with tenderness to palpation at the radial styloid (more distal than the site of tenderness in intersection syndrome) and no crepitus. Furthermore, patients with de Quervain tenosynovitis may have a positive Finkelstein test, which is described as pain along the radial aspect of the wrist with thumb flexion and wrist ulnar deviation. Careful attention to these distinguishing features is essential to avoid misdiagnosing intersection syndrome as de Quervain tenosynovitis.
Evaluation
Although intersection syndrome is typically considered a clinical diagnosis, imaging studies can be used as adjunctive tools when the history and physical examination findings are equivocal.
Diagnostic Imaging Studies
Magnetic resonance imaging (MRI) of the forearm provides soft tissue images and can aid diagnosis.[3][4][14][15] Fluid-sensitive sequences, such as short tau inversion recovery and fat-suppressed proton density, may demonstrate peritendinous fluid or edema in the first and second dorsal compartments, as well as possible tendinosis and muscle edema.
Ultrasound has also been used as an alternative imaging modality.[4][13][16][17][18] However, its accuracy depends heavily on the skill and experience of the ultrasonographer. As in many musculoskeletal conditions, the anatomy relevant to intersection syndrome is fairly superficial. Therefore, a linear ultrasound probe should be utilized. When evaluating for intersection syndrome under ultrasound guidance, the ideal image is in the transverse plane on the short axis. The finding correlating to the diagnosis is a hypoechoic area between the 2 dorsal compartments, indicating swelling or edema caused by friction. A thickening of the tendon sheaths may also be observed.[13]
Although forearm and wrist radiographs can be obtained to confirm the absence of bony pathology, they are not typically necessary to diagnose intersection syndrome.
Treatment / Management
Conservative Management
The recommended treatment of intersection syndrome predominantly includes nonoperative modalities. First-line conservative approaches, such as a period of rest and activity modification, aim to mitigate repetitive wrist motion and, therefore, minimize friction at the junction between the first and second dorsal compartments. Nonsteroidal anti-inflammatory drugs, such as ibuprofen, naproxen, meloxicam, and diclofenac, may be effective for managing acute injury and pain relief.[2] In addition, immobilization with a wrist brace or splint in a neutral position and wrist stretching and eccentric strengthening exercises can provide relief.
Pharmacologic Management
When conservative measures do not resolve or adequately improve symptoms, second-line treatment with corticosteroid injections can be performed with or without ultrasound guidance.[1][2][19][20] Although many different injectable combinations have been described, the typical injection is a 1:1 mixture of a corticosteroid and anesthetic, such as 0.5 mL to 1 mL of triamcinolone 40 mg/mL and 0.5 mL to 1 mL of a local anesthetic. A 23- to 25-gauge needle measuring 1 to 1.5 inches in length is preferred.[13](B3)
Using the in-plane or out-of-plane needle injection technique, the needle should be guided to the intersection where the first dorsal compartment (abductor pollicis longus and extensor pollicis brevis) is crossed over by the second dorsal compartment (extensor carpi radialis brevis and extensor carpi radialis longus) at the point of maximal tenderness.[13] After the injection, the patient should pronate and supinate the wrist while the clinician observes for crepitus and tenderness with palpation. Resolution of the pain can help further confirm the diagnosis. The steroid requires time to achieve its full potential, which may take several weeks following injection. Rehabilitation exercises can be introduced in tandem with the injection after 3 to 5 days.
Surgical Management
In rare, refractory cases, surgical intervention with debridement and release of the second dorsal compartment is indicated. This procedure may be performed under local or regional anesthesia. A slightly curvilinear longitudinal incision is centered at the intersection between the first and second dorsal compartments, approximately 6 cm proximal to Lister tubercle.
Blunt dissection is then carried down through the subcutaneous tissues until the roof of the second dorsal compartment is visualized. This roof is then completely incised along its entire length to decompress and release the extensor carpi radialis brevis and extensor carpi radialis longus tendons. Any surrounding inflamed tenosynovium is also carefully excised while preserving the integrity of the tendons. A concomitant first dorsal compartment release can also be considered through the same incision, with attention to preserving the superficial radial nerve. Following this, the incision is copiously irrigated with normal saline, the skin is closed with the suture of choice for the surgeon, and a sterile dressing with a splint is applied.
Differential Diagnosis
The differential diagnoses for intersection syndrome include:
Prognosis
Although definitive outcome data with respect to intersection syndrome are lacking in the literature, the majority of patients experience resolution of their symptoms with nonoperative treatment.[11] In particular, resolution of crepitus with active tendon loading typically indicates safe return to high-intensity activities. In addition, a worse postoperative course and poorer outcomes are associated with the presence of tendon sheath fibrosis and adhesions.
Complications
Complications associated with intersection syndrome and its treatment include persistent dorsal forearm and wrist pain, along with progressive stiffness in more refractory cases, potentially impacting daily activities and occupational function. Moreover, potential adverse effects due to steroid injections can occur, including fat atrophy, skin depigmentation, transient increases in blood glucose levels, particularly in diabetic patients, and, if performed repeatedly, extensor tendon damage or rupture. Postoperative complications may manifest as wound infections, extensor tendon lacerations, radial nerve injury, and incomplete relief or persistent symptoms.
Postoperative and Rehabilitation Care
The postoperative splint and sutures are removed approximately 2 weeks following surgery, at which point the patient may transition to a removable wrist brace for a brief period of continued immobilization. Referral to an occupational or hand therapist is recommended to restore range of motion and strength. Most patients can return to full activities about 4 to 6 weeks postoperatively.
Deterrence and Patient Education
Intersection syndrome often results from repetitive wrist flexion-extension motions, and its symptoms may have a similar presentation to de Quervain tenosynovitis. Work and activity modifications that limit protracted periods of (especially forceful) wrist motion can help mitigate symptoms. However, patients with persistent dorso-radial distal forearm pain should seek care from a clinician to confirm the diagnosis and guide appropriate treatment options.
Pearls and Other Issues
Key facts to consider about intersection syndrome are as follows:
- Intersection syndrome is an inflammatory tenosynovitis at the intersection of the first and second dorsal compartments of the wrist.
- Patients report pain over the dorso-radial distal forearm and wrist.
- Examination reveals tenderness to palpation of the dorso-radial forearm about 4 to 6 cm proximal to the wrist or Lister tubercle, which is worse with resisted wrist and thumb extension.
- Diagnosis is primarily clinical but may be supported by ultrasound or MRI.
- Treatment is predominantly nonoperative with anti-inflammatories, splinting, and corticosteroid injections. However, surgical debridement or release may be indicated in certain cases.
Enhancing Healthcare Team Outcomes
Accurate diagnosis and effective management of intersection syndrome require a coordinated, interprofessional approach that emphasizes comprehensive skill sets, clear communication, and patient-centered care. Primary care physicians, emergency medicine clinicians, and orthopedists play vital roles in initial assessment and diagnosis, relying on detailed history-taking and focused physical examination to distinguish intersection syndrome from conditions such as de Quervain tenosynovitis. Misdiagnosis may result in inappropriate treatment and prolonged symptoms, making interprofessional collaboration critical for timely and accurate diagnosis. Clinicians must recognize the importance of occupational or hand therapists in delivering conservative management strategies such as activity modification, splinting, and therapeutic exercises. When symptoms persist despite these measures, orthopedic surgeons may be consulted for potential surgical intervention. Each professional must understand their scope of responsibility while contributing their expertise to the shared goal of restoring function and alleviating pain.
Effective interprofessional communication and ongoing care coordination enhance patient safety, outcomes, and team performance. Nurses often serve as the central link between team members, providing patient education, monitoring progress, and reinforcing treatment plans. Pharmacists ensure the safe and effective use of medications, such as nonsteroidal anti-inflammatory drugs, to manage inflammation and pain. Occupational therapists provide critical feedback to the team on a patient's functional improvements and limitations, guiding decisions about the need for advanced interventions. Timely and structured follow-up among all team members ensures that changes in the patient's condition are promptly addressed. Fostering a collaborative culture—where each health professional's input is valued and integrated—supports a seamless continuum of care that prioritizes the patient's recovery, minimizes complications, and promotes optimal outcomes.
Media
(Click Image to Enlarge)
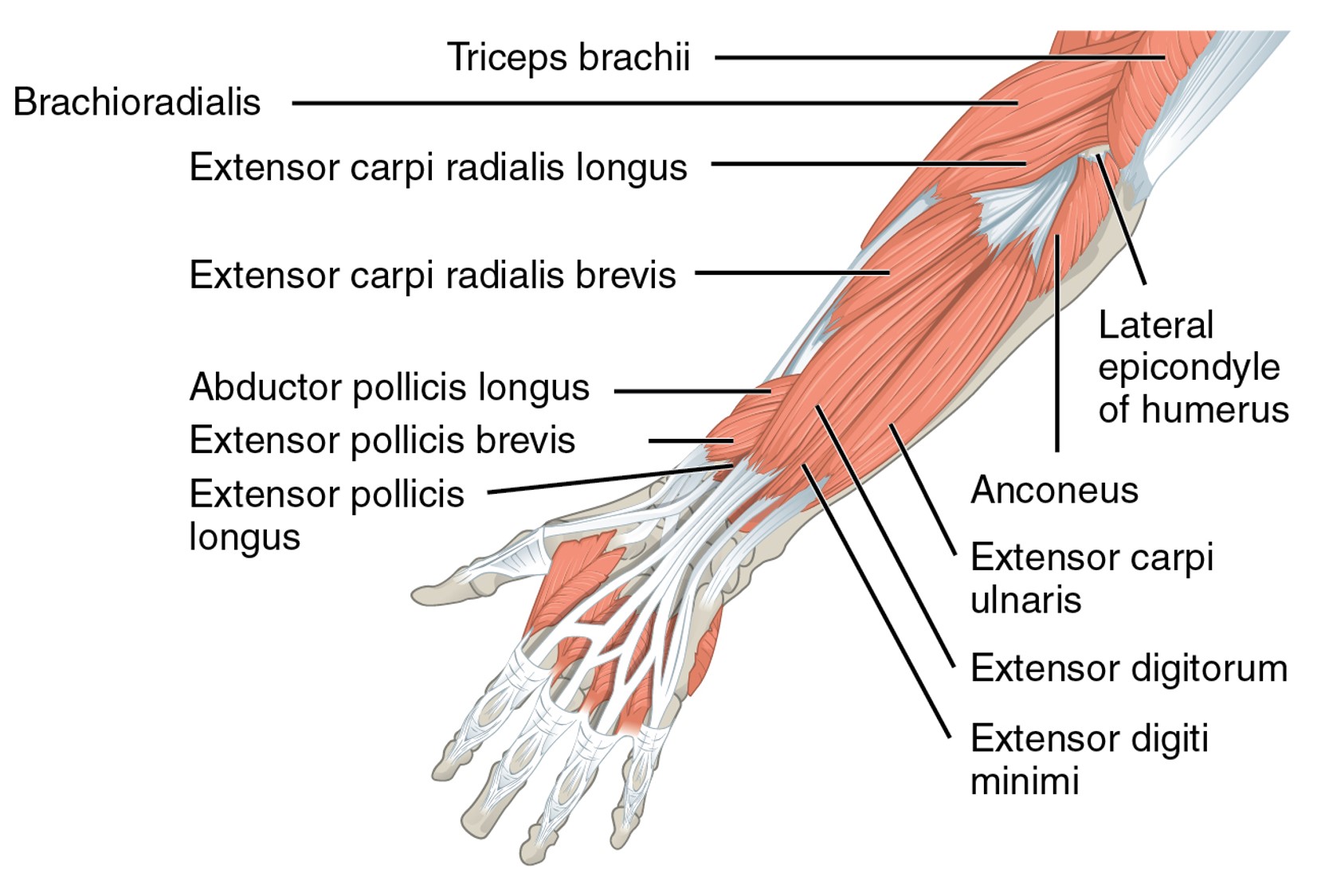
Dorsal Forearm Anatomy. Intersection syndrome affects the first and second compartments of the dorsal wrist extensors. These extensors are part of a collective of 6 dorsal compartments that are variably responsible for wrist and digital extension.
CFCF, Public Domain, via Wikimedia Commons
References
Browne J, Helms CA. Intersection syndrome of the forearm. Arthritis and rheumatism. 2006 Jun:54(6):2038 [PubMed PMID: 16736508]
Level 3 (low-level) evidenceServi JT. Wrist pain from overuse: detecting and relieving intersection syndrome. The Physician and sportsmedicine. 1997 Dec:25(12):41-4. doi: 10.3810/psm.1997.12.1401. Epub [PubMed PMID: 20086879]
McNally E, Wilson D, Seiler S. Rowing injuries. Seminars in musculoskeletal radiology. 2005 Dec:9(4):379-96 [PubMed PMID: 16315119]
Costa CR, Morrison WB, Carrino JA. MRI features of intersection syndrome of the forearm. AJR. American journal of roentgenology. 2003 Nov:181(5):1245-9 [PubMed PMID: 14573413]
Patrick NC, Hammert WC. Hand and Wrist Tendinopathies. Clinics in sports medicine. 2020 Apr:39(2):247-258. doi: 10.1016/j.csm.2019.10.004. Epub [PubMed PMID: 32115083]
Adams JE, Habbu R. Tendinopathies of the Hand and Wrist. The Journal of the American Academy of Orthopaedic Surgeons. 2015 Dec:23(12):741-50. doi: 10.5435/JAAOS-D-14-00216. Epub 2015 Oct 28 [PubMed PMID: 26510626]
Prasad N, LaPorte DM. Tendinitis Around the Wrist and Hand. Instructional course lectures. 2025:74():143-154 [PubMed PMID: 39745557]
Tan YL, Eide SE, Hallinan JTPD. Intersection Syndrome: A Proximal Cause of Radial-Sided Wrist Pain. American journal of physical medicine & rehabilitation. 2024 Mar 1:103(3):e35. doi: 10.1097/PHM.0000000000002362. Epub 2023 Oct 30 [PubMed PMID: 37903628]
Skinner TM. Intersection Syndrome: The Subtle Squeak of an Overused Wrist. Journal of the American Board of Family Medicine : JABFM. 2017 Jul-Aug:30(4):547-551. doi: 10.3122/jabfm.2017.04.170053. Epub [PubMed PMID: 28720637]
Sunagawa T, Dohi D, Shinomiya R. Distal Intersection Syndrome Combined With Partial Attritional Changes of the Extensor Carpi Radialis Brevis in Tennis Players. Journal of hand surgery global online. 2021 Jul:3(4):224-227. doi: 10.1016/j.jhsg.2021.04.005. Epub 2021 May 20 [PubMed PMID: 35415554]
Balakatounis K, Angoules AG, Angoules NA, Panagiotopoulou K. Synthesis of evidence for the treatment of intersection syndrome. World journal of orthopedics. 2017 Aug 18:8(8):619-623. doi: 10.5312/wjo.v8.i8.619. Epub 2017 Aug 18 [PubMed PMID: 28875127]
Yokota H, Yasui M, Hirai S, Hatayama N, Ohshima S, Nakano T, Naito M. Evaluation of the pressure on the dorsal surface of the distal radius using a cadaveric and computational model: clinical considerations in intersection syndrome and Colles' fracture. Anatomical science international. 2020 Jan:95(1):38-46. doi: 10.1007/s12565-019-00491-5. Epub 2019 Jun 4 [PubMed PMID: 31165418]
Giovagnorio F, Miozzi F. Ultrasound findings in intersection syndrome. Journal of medical ultrasonics (2001). 2012 Oct:39(4):217-20. doi: 10.1007/s10396-012-0370-y. Epub 2012 May 8 [PubMed PMID: 27279107]
Tas N, Ogul H, Kantarci M. Intersection syndrome. Joint bone spine. 2024 Jul:91(4):105710. doi: 10.1016/j.jbspin.2024.105710. Epub 2024 Feb 22 [PubMed PMID: 38401622]
Plotkin B, Sampath SC, Sampath SC, Motamedi K. MR Imaging and US of the Wrist Tendons. Radiographics : a review publication of the Radiological Society of North America, Inc. 2016 Oct:36(6):1688-1700 [PubMed PMID: 27726753]
Naredo E, Murillo-González J, Mérida Velasco JR, Olivas Vergara O, Kalish RA, Gómez-Moreno C, García-Carpintero Blas E, Fuensalida-Novo G, Canoso JJ. Examining the Forearm Intersection through Palpation and Ultrasonography. Diagnostics (Basel, Switzerland). 2024 Jan 4:14(1):. doi: 10.3390/diagnostics14010116. Epub 2024 Jan 4 [PubMed PMID: 38201426]
Giray E, Keles Ercisli A, İlleez ÖG, Aktaş İ, Yağcı İ. How can you examine intersection syndrome via ultrasound? A technical description. Archives of rheumatology. 2023 Jun:38(2):324-325. doi: 10.46497/ArchRheumatol.2023.9830. Epub 2022 Nov 4 [PubMed PMID: 37680506]
Flores DV, Murray T, Jacobson JA. Diagnostic and Interventional US of the Wrist and Hand: Quadrant-based Approach. Radiographics : a review publication of the Radiological Society of North America, Inc. 2023 Aug:43(8):e230046. doi: 10.1148/rg.230046. Epub [PubMed PMID: 37498783]
Pujalte GGA, Vomer R, Shah N. Injections of the Hand and Wrist: Part II. Carpal Tunnel Syndrome, Ganglion Cyst, Intersection Syndrome, Triangular Fibrocartilage Complex Injury, and de Quervain Tenosynovitis. American family physician. 2024 Oct:110(4):402-410 [PubMed PMID: 39418544]
Waryasz GR, Tambone R, Borenstein TR, Gil JA, DaSilva M. A Review of Anatomical Placement of Corticosteroid Injections for Uncommon Hand, Wrist, and Elbow Pathologies. Rhode Island medical journal (2013). 2017 Mar 1:100(2):31-34 [PubMed PMID: 28246658]
Satteson E, Tannan SC. De Quervain Tenosynovitis. StatPearls. 2025 Jan:(): [PubMed PMID: 28723034]
Gregush RE, Habusta SF. Ganglion Cyst. StatPearls. 2025 Jan:(): [PubMed PMID: 29262133]
Anthony JH, Hadeed A, Hoffler CE. Cheiralgia Paresthetica. StatPearls. 2025 Jan:(): [PubMed PMID: 31424784]
Hayat Z, Varacallo M. Scaphoid Wrist Fracture. StatPearls. 2024 Jan:(): [PubMed PMID: 30725592]
Beutel BG, Konstanty J, Beeker RW, Rehman UH. Carpal Ligament Instability. StatPearls. 2025 Jan:(): [PubMed PMID: 32491661]