Introduction
A hypertensive crisis refers to a severe acute elevation in blood pressure (>180/120 mm Hg) with or without signs of hypertension-mediated organ damage. This condition is classified as a hypertensive emergency when the elevated blood pressure is accompanied by acute hypertension-mediated organ damage (formerly known as end-organ damage). In contrast, in the absence of acute hypertension-mediated organ damage, the condition is termed a hypertensive urgency.[1]
A hypertensive emergency is a potentially life-threatening condition and requires early diagnosis and immediate management. Without treatment, the prognosis is poor. Only 20% of individuals with untreated hypertensive emergencies survive beyond 1 year, and the median survival time is reported to be approximately 10.4 months.[2] However, significant improvement in 1-year outcomes has been observed in patients who receive timely and appropriate treatment following early diagnosis.[3]
While the absolute blood pressure level is important, the rate at which blood pressure rises may be even more critical. Patients with chronic hypertension often tolerate higher blood pressure levels better than those who were previously normotensive or had well-controlled hypertension.[4] This difference underscores the importance of prompt blood pressure reduction in managing hypertensive emergencies to prevent or minimize further damage to target organs. However, returning blood pressure to completely normal levels is not always necessary.[5]
Common manifestations of hypertension-mediated organ damage in hypertensive emergencies include encephalopathy, intracerebral hemorrhage, acute ischemic stroke, acute myocardial infarction, acute left ventricular failure with pulmonary edema, unstable angina pectoris, dissecting aortic aneurysm, acute renal failure, and eclampsia. Patients experiencing hypertension emergencies require admission, and oral antihypertensive medications are not recommended for initial management.[6] Malignant hypertension is a severe and aggressive form of hypertensive emergency, defined by an extreme elevation of blood pressure with hypertension-associated microangiopathies affecting various organs, including the retina, kidneys, and brain.[7] The hallmark feature of malignant hypertension is retinal involvement, presenting with changes such as flame-shaped hemorrhages and papilledema, with and without microangiopathy and disseminated intravascular coagulation.
The hypertension-mediated organ damage in malignant hypertension is not limited to the retina. Patients may also present with hypertensive encephalopathy, pulmonary edema, and acute renal dysfunction. As the name indicates, malignant hypertension is associated with rapid disease progression and a poor prognosis, if not promptly and properly treated.[7] Hypertensive urgency is a form of hypertensive crisis characterized by a severe elevation in blood pressure, typically a systolic blood pressure greater than 180 mm Hg or a diastolic blood pressure exceeding 120 mm Hg, without evidence of acute or imminent target organ damage. Unlike hypertensive emergencies, hypertensive urgency does not involve life-threatening conditions such as stroke, myocardial infarction, acute renal failure, or other forms of end-organ damage that require immediate, aggressive intervention.[8]
Management typically involves gradually reducing blood pressure, usually with oral antihypertensive medications, over several hours to days in a controlled outpatient setting. Patients are often asymptomatic or may present with nonspecific symptoms that are not indicative of acute organ injury. The lifetime prevalence of hypertensive crisis is estimated to be approximately 1% in the general population, while individuals with hypertension face up to a 2% lifetime risk of experiencing a hypertensive crisis.[6] Notably, nearly one-fourth of patients presenting to the emergency department with a hypertensive crisis have no prior diagnosis of hypertension.[9]
Hypertensive crisis is generally more prevalent in women, although some study results have reported a higher prevalence in men.[1][10][11] Individuals with hypertension who are nonadherent with treatment are at a significantly higher risk of developing hypertensive crisis. Additionally, the condition is reported to be more common in patients with secondary hypertension compared to those with essential hypertension.[10]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
The etiology of hypertensive crisis is multifactorial, involving factors such as undiagnosed or poorly managed secondary hypertension, acute illnesses, nonadherence to medications, inadequate management, and illicit drug use. Early recognition and appropriate management of the underlying causes are critical to preventing hypertension-mediated organ damage.[12]
The common etiologies and precipitating factors of hypertensive crises are as follows:
Medication-related factors
- Medication nonadherence
- Withdrawal of antihypertensive medications
- Drug interactions or overdose:
- Monoamine oxidase inhibitors combined with tyramine-rich foods (eg, aged cheeses, red wine)
- Sympathomimetic drugs, such as decongestants, weight-loss drugs, or stimulant medications
Renal causes
- Renovascular diseases, such as renal artery stenosis, polyarteritis nodosa, and Takayasu arteritis
- Renal parenchymal disease, including glomerulonephritis, tubulointerstitial nephritis, systemic sclerosis, hemolytic-uremic syndrome, systemic lupus erythematosus
Endocrine disorders
- Pheochromocytoma
- Cushing disease
- Primary hyperaldosteronism
- Renin-secreting tumors
Cardiovascular abnormalities
- Coarctation of the aorta
Central nervous system disorders
- Head injury
- Cerebral infarction
- Intracerebral hemorrhage
Substance use and withdrawal
- Illicit drug use:
- Cocaine
- Phencyclidine
- Amphetamines and metamphetamines
- Excessive alcohol consumption, especially during binge drinking or withdrawal
Psychosocial and physiologic stress
- Severe emotional stress
- Acute pain
- Anxiety
Epidemiology
The reported prevalence of hypertensive crises varies across the literature mainly due to inconsistencies in definition, differences in study populations, and variations in methodology, including study protocols and inclusion and exclusion criteria. Despite these differences, it is estimated that approximately 1 in 100 individuals with hypertension will experience a hypertensive crisis during their lifetime.[5] Overall, 0.5% to 3% of all emergency department visits involve patients presenting with a suspected hypertensive emergency, and 25% of those are confirmed to have a hypertensive emergency and require immediate intervention to reduce blood pressure to safe levels. [13]
Results from one study suggest that hypertensive crises are more prevalent in African American or Black populations living in urban areas, with a significantly higher prevalence compared to the overall United States population. However, the identified predictors of hypertensive emergencies included advanced age, male sex, renal insufficiency, and coronary artery disease. Notably, race was not reported as an independent predictor of presenting with a hypertensive emergency.[14]
Pathophysiology
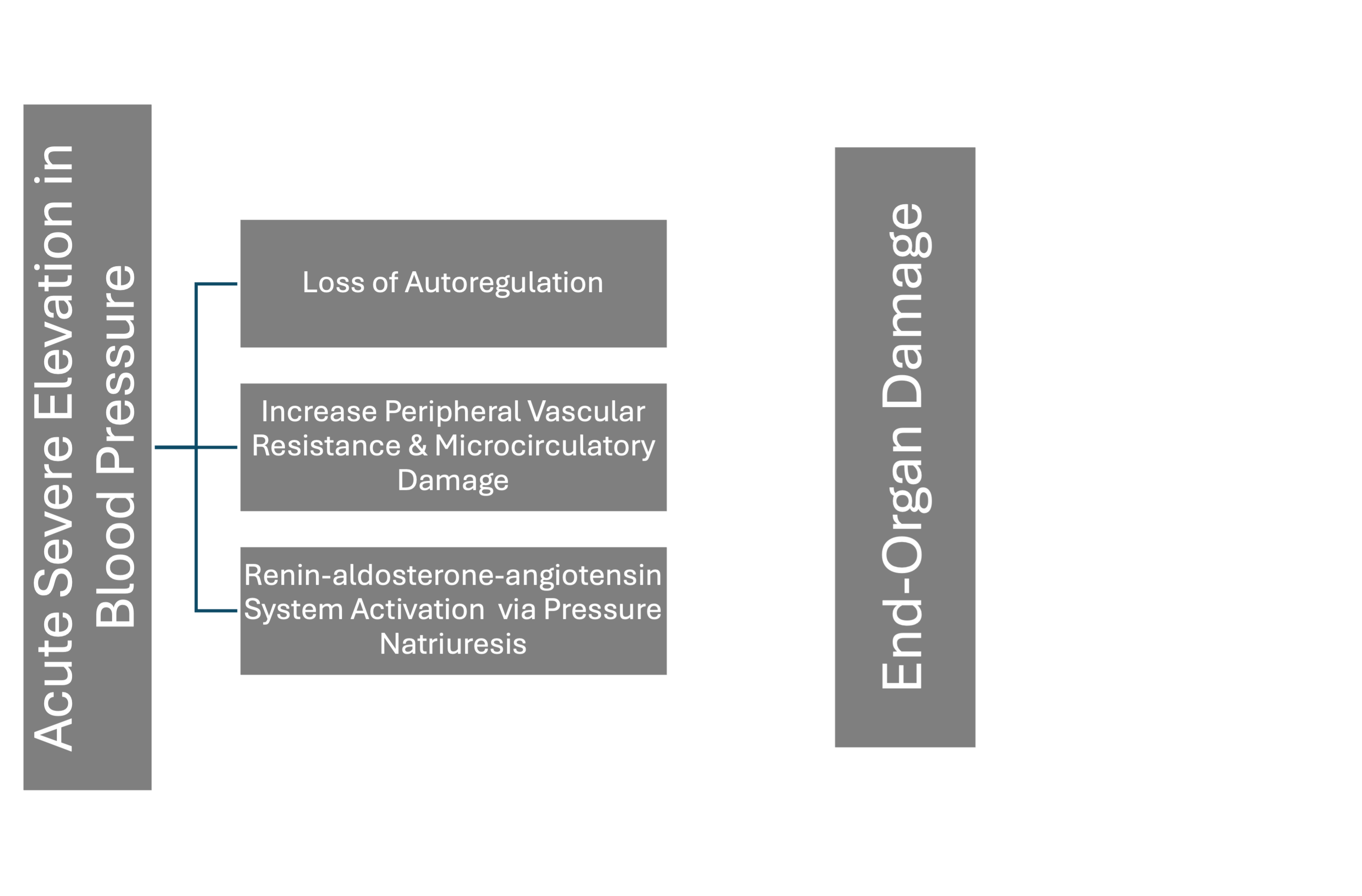
Hypertensive emergencies occur when blood pressure increases rapidly and significantly over a short period. The mechanism underlying hypertension-mediated organ damage is complex and involves a combination of vascular, neurohormonal, and endothelial dysfunction (see Image. Pathophysiology of Hypertension-Mediated Organ Damage). A key factor is increased systemic vascular resistance primarily due to enhanced vasoconstriction mediated by renin-angiotensin system activation. Additional contributing mechanisms include pressure natriuresis, tissue hypoperfusion, and ischemia, all of which play crucial roles in the development of end-organ damage.[15]
A characteristic histopathological feature of hypertension-mediated vascular injury is fibrinoid necrosis of the small vessels. Additionally, red cell destruction commonly occurs as erythrocytes pass through narrowed or obstructed vessels, resulting in microangiopathic hemolytic anemia. Another feature of hypertensive emergencies is the loss of cerebral autoregulation, which may result in hypertensive encephalopathy.[16] This condition is characterized by severe headache, nausea, vomiting, altered mental status, and, in severe cases, seizures or coma, reflecting acute cerebral dysfunction caused by elevated blood pressure.
Endothelial Dysfunction
Endothelial injury plays a central role in the pathophysiology of hypertension-mediated organ damage. Elevated blood pressure increases shear stress on the endothelial cells, disrupting the balance between vasodilation and vasoconstriction. This promotes vascular permeability and triggers an inflammatory response. In response to this stress, the endothelium releases proinflammatory cytokines, which increase vascular permeability and lead to plasma leakage into surrounding tissues. Elevated blood pressure also stimulates vascular smooth muscle contraction, further increasing peripheral vascular resistance and exacerbating the hypertensive crisis.[17] This creates a cycle where rising vascular resistance perpetuates elevated blood pressure, accelerating the progression of organ damage if not promptly interrupted.
Disruption in Autoregulation of Blood Flow
Under normal circumstances, many organs, particularly the brain and kidneys, possess autoregulation mechanisms that maintain stable blood flow despite fluctuations in systemic blood pressure. However, during a hypertensive emergency, this autoregulation becomes overwhelmed, resulting in the inability to maintain adequate perfusion.[18] The failure of the protective autoregulatory mechanism can lead to cerebral edema or hemorrhagic stroke due to the rupture of fragile blood vessels. Similarly, it can precipitate acute kidney injury due to damage to renal vasculature and impairment of glomerular filtration.
Neurohumoral Activation
In response to severe hypertension, the body activates several neurohormonal systems that further exacerbate the situation. Increased sympathetic activity and renal hypoperfusion stimulate the renin-angiotensin-aldosterone system, leading to sodium retention and fluid expansion, further elevating blood pressure and accelerating organ damage. Renin-angiotensin-aldosterone system activation also contributes to oxidative stress and the formation of peroxynitrite, which impairs nitric oxide bioactivity, leading to endothelial dysfunction and vascular damage.[19] Activating the sympathetic nervous system causes vasoconstriction and increases afterload, further straining the cardiovascular system. Additionally, elevated blood pressure enhances the release of endothelin-1, a potent vasoconstrictor, contributing to vasospasm and worsening organ damage.
Micro and Macroangiopathy
Damage to small blood vessels, particularly in the retina, kidneys, and brain, is a hallmark of hypertensive emergencies. In the retina, severe hypertension can cause hypertensive retinopathy, characterized by flame-shaped hemorrhages, cotton wool spots, and papilledema.[7] In addition to microvascular damage, macrovascular complications, such as stroke, acute coronary syndromes, and aortic dissection, can occur due to the effect of elevated blood pressure on larger blood vessels. These events contribute significantly to the morbidity and mortality associated with hypertensive crises.
Activation of Inflammatory and Coagulation Pathways
Elevated blood pressure can activate the coagulation cascade, increasing the risk of thrombosis and microthrombi formation. The coagulation cascade activation leads to thrombotic obliteration of small vessels, disseminated intravascular coagulation, and thrombotic microangiopathy.[20] These processes further compromise tissue perfusion, worsening ischemia and contributing to organ damage, particularly in the brain (ie, ischemic stroke) or kidneys (ie, acute kidney injury). Inflammatory mediators, such as cytokines and chemokines, are released in response to endothelial injury, amplifying inflammation and accelerating tissue damage. This inflammatory cascade can also recruit immune cells to the affected sites, perpetuating vascular injury and contributing to the progression of hypertension-mediated organ damage.
History and Physical
The symptoms of a hypertensive crisis vary depending on the organ involved and the severity of the condition. Patients with hypertensive urgency are often asymptomatic and may be diagnosed incidentally after elevated blood pressure is detected. However, some individuals may experience nonspecific symptoms such as body aches, headaches, or anxiety. In contrast, the symptoms of hypertensive emergency are directly related to hypertensive-mediated organ damage. Common presenting symptoms include headaches, visual disturbances, chest pain, and shortness of breath. Patients with hypertensive encephalopathy or malignant hypertension often present with dizziness, lethargy, visual symptoms (blindness), seizures, and unconsciousness.[21]
Severely elevated blood pressure is the characteristic feature of patients presenting with hypertensive crises. At the same time, other clinical findings depend on the presence and severity of acute or worsening organ damage caused by the elevated pressure. Blood pressure should be measured in both arms, as a significant difference between the right and left arm readings may indicate aortic dissection involving the subclavian artery.
Assessment of the distal pulses is equally important, and a radio-radial or radio-femoral delay is another key clinical finding suggestive of aortic dissection.[22] Additionally, diminished or absent pulses in the limbs may indicate compromised blood flow due to vessel obstruction or rupture. In patients with hypertension-mediated heart failure or acute coronary syndrome, findings such as elevated jugular venous distension, bilateral pulmonary rales, and the presence of S3 or S4 heart sounds may be observed. Meanwhile, oliguria can be an indicator of hypertension-induced renal dysfunction.
Fundoscopy is an essential component of clinical examination in patients with suspected hypertension emergencies. Individuals with severe forms, such as hypertensive emergency (malignant hypertension), often exhibit retinopathy findings including flame-shaped hemorrhages, cotton wool spots, and papilledema.[23] Acute confusion is commonly seen in hypertensive encephalopathy, whereas focal neurological deficit may be present in patients experiencing acute cerebrovascular accidents. Prompt neurological assessment is crucial for distinguishing between these conditions and guiding appropriate imaging and management decisions.
Evaluation
A thorough history and physical examination are essential for evaluating patients presenting with severely elevated blood pressure or an acute rise from a previously normal baseline, even if the presenting blood pressure is less than 180/120 mm Hg. The history should primarily focus on the patient's hypertension management, including treatment adherence, and should also assess for the presence of symptoms suggestive of acute hypertension-mediated organ damage. A comprehensive history should be followed by a thorough system examination to diagnose and evaluate the severity of hypertension-mediated organ damage. The clinical findings should guide additional investigations to confirm the extent of organ damage.[12]
The following investigations are recommended to evaluate the severity of hypertensive crisis and its associated complications:
- Electrocardiography: Useful for assessing acute coronary syndrome and arrhythmia
- Chest x-ray: Helps confirm pulmonary edema and may help diagnose acute aortic syndrome
- Urinalysis: For evaluating hypertension-mediated renal dysfunction
- Findings such as hematuria and proteinuria indicate renal dysfunction.
- Electrolytes and creatinine: Important for determining the extent of renal dysfunction and guiding the selection of antihypertensive medications
- Cardiac biomarkers: Indicated when there is clinical suspicion of acute coronary syndrome or heart failure based on history and physical examination
- Toxicology screen: Maybe considered in selected patients to identify possible triggers of a hypertensive crisis
- Neuroimaging, eg computed tomography (CT) or magnetic resonance imaging: Recommended where there is clinical suspicion of head trauma, intracranial hemorrhage, stroke, or hypertensive encephalopathy
- Echocardiogram, eg, transthoracic or transesophageal echocardiogram: Indicated when aortic dissection is suspected
- Alternatively, a CT angiogram or magnetic resonance angiogram can be used to confirm the diagnosis.[20]
Treatment / Management
The acute management of hypertension in stroke and intracranial hemorrhage is the only scenario that has been rigorously studied in randomized controlled trials. In contrast, the management of other forms of hypertensive emergencies primarily relies on observational studies and expert consensus guidelines.[24] Patients presenting with severely elevated blood pressures without evidence of acute or worsening hypertension-mediated organ damage (hypertensive urgency) typically do not require hospital admission. These cases are often managed by adjusting existing antihypertensive therapy or adding oral agents. However, if not adequately treated, they remain at risk of developing a hypertensive emergency. Therefore, timely outpatient follow-up is crucial for monitoring blood pressure control.
Importantly, rapid blood pressure reduction with intravenous antihypertensive medications, in this patient population, has not been shown to improve outcomes and may be harmful. Thus, it is not recommended.[25] Such abrupt reductions can compromise organ perfusion, particularly in patients with chronic hypertension whose autoregulatory mechanisms are adapted to higher baseline pressures.
Treating patients presenting with a hypertensive emergency is determined by the clinical presentation as well as the type and extent of organ damage. Common manifestations of hypertension emergencies include cerebrovascular accidents (ischemic or hemorrhagic stroke), malignant hypertension (acute hypertensive microangiopathy), hypertensive encephalopathy, acute coronary syndrome, acute decompensated heart failure or pulmonary edema, acute aortic disease, and preeclampsia or eclampsia.
The primary goal in managing hypertensive emergencies is to minimize organ damage through a controlled reduction in blood pressure within a healthcare setting. This is typically achieved using intravenous antihypertensive medications administered under close hemodynamic monitoring to avoid complications that can arise from an abrupt fall in blood pressure. Adequate therapy, including the choice of the medication and the blood pressure target, must be tailored to the specific hypertensive emergency and the organ systems involved.[26][27][28][29]
A rapid or excessive reduction in blood pressure is not recommended, as it may lead to ischemic injury in vascular territories that have adapted to chronically elevated pressures. In most hypertensive emergencies, the goal is to reduce blood pressure by no more than 25% within the first hour, followed by a gradual reduction to normal levels over the next 24 to 48 hours (see Table. Intravenous Medications for Hypertensive Emergencies). However, certain conditions, such as aortic dissection, eclampsia, and pheochromocytoma crisis, require a more immediate and aggressive blood pressure lowering to reduce the risk of life-threatening complications.
Table. Intravenous Medications for Hypertensive Emergencies
| Class | Drugs | Dose | Special Consideration |
| Dihydropyridine calcium channel blockers | 1. Nicardipine |
Initial 5 mg/h, increasing every 5 min by 2.5 mg/h to a maximum of 15 mg/h |
Contraindicated in advanced aortic stenosis; no dose adjustment needed for older patients. |
|
2. Clevidipine
|
Initial 1–2 mg/h, doubling every 90 s until blood pressure approaches target, then increasing by less than double every 5–10 min; maximum dose 32 mg/h; maximum duration 72 h |
Contraindicated in patients with soybean, soy product, egg, and egg product allergy and patients with defective lipid metabolism (eg, pathological hyperlipidemia, lipoid nephrosis, or acute pancreatitis). Use a low-end dose range for older patients. |
|
|
Nitric oxide-dependent vasodilators |
1. Sodium nitroprusside
|
Initial 0.3–0.5 mcg/kg/min; increase in increments of 0.5 mcg/kg/min to achieve target blood pressure; maximum dose 10 mcg/kg/min; duration of treatment as short as possible. For infusion rates of 4–10 mcg/kg/min or duration >30 min, thiosulfate can be coadministered to prevent cyanide toxicity. |
Intra-arterial blood pressure monitoring is recommended to prevent “overshoot.” Lower dosing adjustment is required for older individuals. Tachyphylaxis is common with extended use. Cyanide toxicity with prolonged use can result in irreversible neurological changes and cardiac arrest. |
|
2. Nitroglycerin |
Initial 5 mcg/min; increase in increments of 5 mcg/ min every 3–5 min to a maximum of 20 mcg/min. | Use only in patients with acute coronary syndrome and/or acute pulmonary edema. Do not use in volume-depleted patients. | |
| Direct vasodilators | Hydralazine | Initial 10 mg via slow intravenous infusion (maximum initial dose 20 mg); repeat every 4–6 h as needed. | Blood pressure decreases within 10–30 min, and the fall lasts 2–4 h. However, the unpredictability of response and prolonged duration of action do not make hydralazine a desirable first-line agent for acute treatment in most patients. |
| Adrenergic blockers |
1. Esmolol: Selective beta blocker |
Loading dose 500–1000 mcg/kg/min over 1 min, followed by a 50-mcg/kg/min infusion. The bolus dose is repeated for additional dosing, and the infusion is increased in 50-mcg/kg/min increments as needed to a maximum of 200 mcg/kg/min. |
Contraindicated in patients with concurrent β-blocker therapy, bradycardia, or decompensated heart failure. Monitor for bradycardia. This may worsen heart failure. Higher doses may block beta2 receptors and impact lung function in reactive airway disease. |
|
2. Labetalol: Combined alpha and nonselective beta blocker |
Initial 0.3–1.0-mg/kg dose (maximum 20 mg), slow intravenous injection every 10 min or 0.4–1.0-mg/kg/h intravenous infusion up to 3 mg/kg/h. Adjust rate up to a total cumulative dose of 300 mg. This dose can be repeated every 4–6 h. |
Contraindicated in reactive airways disease or chronic obstructive pulmonary disease. Especially useful in hyperadrenergic syndromes. May worsen heart failure and should not be given to patients with second- or third-degree heart block or bradycardia. |
|
|
3. Phentolamine: Nonselective alpha blocker |
Intravenous bolus dose 5 mg. Additional bolus doses every 10 min as needed to lower blood pressure to the target. | Used in hypertensive emergencies induced by catecholamine excess (pheochromocytoma, interactions between monoamine oxidase inhibitors and other drugs or food, cocaine toxicity, amphetamine overdose, or clonidine withdrawal). | |
| Angiotensin-converting enzyme inhibitors | Enalaprilat | Initial 1.25 mg over a 5-min period. Doses can be increased to 5 mg every 6 h to achieve the blood pressure target. |
Contraindicated in pregnancy and should not be used in acute myocardial infarction or bilateral renal artery stenosis. Mainly valuable for hypertensive emergencies associated with high plasma renin activity. The dose is not easily adjusted. Relatively slow onset of action (15 min) and unpredictable response. |
| Selective dopamine agonist | Fenoldopam | Initial 0.1–0.3 mcg/kg/min; may be increased in increments of 0.05–0.1 mcg/kg/min every 15 min until target BP is reached. Maximum infusion rate 1.6 mcg/kg/min. | Contraindicated in patients at risk of increased intraocular pressure (glaucoma) or intracranial pressure and those with sulphite allergy. |
If frequent noninvasive cuff measurements can potentially lead to inaccurate blood pressure assessment or if end-organ damage is threatening, arterial catheterization should be considered to obtain precise, beat-to-beat blood pressure monitoring, enabling more accurate medication titration.
The major exceptions to gradual blood pressure lowering over the first day are as follows:
- Acute ischemic stroke: The benefits of immediate blood pressure reduction are uncertain. Antihypertensive treatment is generally avoided in patients not receiving thrombolysis or thrombectomy unless blood pressure exceeds 220/120 mm Hg. In such cases, a cautious reduction of 10% to 15%, over several hours, may be considered.[1][15]
- Acute aortic dissection: The systolic blood pressure should be reduced to 120 mm Hg within the first hour, with a target heart rate of around 60 bpm to decrease aortic shear stress.[30][31][32] First-line treatment is typically a beta blocker.[30][33]
- Acute intracerebral hemorrhage: Aggressive blood pressure lowering to less than 140 in the acute phase of intracranial hemorrhage (within 6 hours) has not shown improved outcomes and may increase risks.[34] Current guidelines recommend a gradual reduction in patients with systolic blood pressure of 220 mm Hg or higher, using intravenous antihypertensive drugs under close hemodynamic monitoring.[35]
- Acute myocardial infarction: Nitroglycerin is the drug of choice for blood pressure management unless the patient has used phosphodiesterase inhibitors (eg, sildenafil or tadalafil) within the previous 48 hours.
- Pheochromocytoma crisis: A rapid reduction of systolic blood pressure to less than 140 mm Hg within the first hour is recommended.[1] Preferred agents include phentolamine, clevidipine, and nicardipine.
- Preeclampsia and eclampsia: Immediate blood pressure control is necessary. First-line drugs include hydralazine, labetalol, and nicardipine, typically in conjunction with magnesium sulphate for seizure prophylaxis. (A1)
Following stabilization, intravenous antihypertensive therapy is tapered, and patients are transitioned to oral medications for continued blood pressure control. The underlying cause of the hypertensive emergency, patient comorbidities, and response to initial therapy should guide the choice of oral agents.
Differential Diagnosis
Hypertensive crisis has a broad differential diagnosis, encompassing various conditions that may present with or contribute to hypertension-mediated organ dysfunction. These include:
- Aortic coarctation
- Aortic dissection
- Chronic kidney disease
- Eclampsia
- Hypercalcemia
- Hyperthyroidism
- Pheochromocytoma
- Renal artery stenosis
- Subarachnoid hemorrhage
Prognosis
The prognosis for patients with an untreated hypertensive crisis is poor. The 1-year mortality rate exceeds 79%, with a median survival of just 10.4 months in the absence of treatment.[1] However, timely and appropriate management significantly improves outcomes. Mortality is closely associated with the degree of blood pressure elevation and the extent of organ damage. Early intervention to prevent or limit organ injury is essential to improving survival rates.
With early diagnosis and appropriate treatment, the prognosis of hypertensive emergencies has improved significantly over the last few decades.[36] Despite better survival rates, patients presenting with a hypertensive emergency remain at substantially higher risk for long-term cardiovascular and renal complications compared to those with hypertension without a history of hypertensive emergency. Moreover, patients admitted to a coronary care unit for hypertensive emergencies have more than 5 times the mortality rate as those without hospitalization.[37][38]
While the short-term prognosis for most patients with malignant hypertension is favorable with appropriate treatment, long-term outcomes can be compromised by frequent exacerbations. Patients who are noncompliant with therapy are at increased risk for serious complications, including stroke, vision loss, kidney damage, and adverse cardiac events.[39] Elevated cardiac troponins and renal dysfunction at presentation are associated with poor short-term outcomes. Over the long term, the risk of renal complications is influenced by the severity of proteinuria and the effectiveness of blood pressure control following recovery.[40][41]
Complications
A hypertensive crisis can lead to life-threatening complications, especially when it progresses to a hypertensive emergency with acute target organ damage. Major complications include:
- Cardiovascular
- Myocardial infarction
- Heart failure
- Aortic Dissection
- Neurological
- Stroke
- Hypertensive encephalopathy
- Intracerebral hemorrhage
- Renal
- Renal impairment
- Acute kidney injury
- Ocular
- Ocular damage
- Hypertensive retinopathy with potential damage
- Pregnancy
- Eclampsia
- HELLP (hemolysis, elevated liver enzymes, and low platelet count) syndrome
- Placental abruption
Prompt recognition and controlled blood pressure reduction are crucial for preventing irreversible damage and improving outcomes. Patients with hypertensive emergencies experience significant cardiovascular and renal morbidity and mortality and are at higher risk of subsequent hospitalization.[42]
Deterrence and Patient Education
Effective patient education is essential for preventing hypertensive crises and reducing the risk of recurrence. Education should focus on a combination of lifestyle modification, medication adherence, and awareness of the warning signs and symptoms of hypertensive emergencies. Patients should be counseled on the importance of monitoring blood pressure and adhering to prescribed antihypertensive medications, even when they are asymptomatic. Lifestyle changes—reducing sodium intake, maintaining a healthy weight, engaging in regular physical activity, limiting alcohol consumption, and quitting smoking—should be strongly encouraged.
Additionally, patients must be informed about the signs and symptoms of a hypertensive crisis, including severe headache, chest pain, shortness of breath, visual disturbances, and confusion. They should seek immediate medical attention if any of these symptoms occur. Regular follow-up with clinicians is critical to ensure continued blood pressure control. Education about the long-term risks of uncontrolled hypertension, such as stroke, heart attack, kidney failure, and vision loss, can help reinforce the importance of adherence and ongoing care.
Pearls and Other Issues
Key facts to keep in mind about hypertensive crisis include the following:
- Hypertensive crisis includes hypertensive urgency and hypertensive emergency.
- Hypertensive emergency is defined as severe hypertension (usually >180/120 mm Hg) with signs of acute target organ damage.
- Hypertensive urgency involves severe hypertension without acute target organ damage.
- Common signs of organ damage include encephalopathy, stroke, myocardial infarction, heart failure, aortic dissection, and acute kidney injury.
- Immediate reduction in blood pressure is required in a hypertensive emergency, but lowering must be controlled to avoid ischemia.
- In most cases, blood pressure should be reduced by no more than 25% within the first hour and gradually returned to normal over 24–48 hours.
- Exceptions requiring rapid blood pressure reduction include aortic dissection, eclampsia, and pheochromocytoma crisis.
- First-line intravenous drugs include nicardipine, clevidipine, labetalol, esmolol, nitroglycerin (for ischemia), and sodium nitroprusside.
- Oral medications are used for hypertensive urgency; rapid intravenous treatment is not indicated.
- In malignant hypertension, Fundoscopy may reveal papilledema, flame hemorrhages, or cotton wool spots.
- A CT scan of the brain is indicated if stroke or encephalopathy is suspected.
- Renal function and urinalysis help evaluate hypertensive nephropathy.
- Aortic dissection may present with chest or back pain and BP differences between limbs.
- Long-term control includes lifestyle modification and strict medication adherence.
Enhancing Healthcare Team Outcomes
Managing a hypertensive crisis requires a coordinated interprofessional approach involving an internist, nephrologist, cardiologist, neurologist, and nursing staff. Uncontrolled elevated blood pressure is associated with high morbidity and mortality, along with significant healthcare costs. Therefore, primary clinicians, including nurse practitioners and physician assistants, play a critical role in regular blood pressure monitoring and emphasizing adherence to antihypertensive therapy.
Hospital admission is not recommended for asymptomatic individuals with severely elevated blood pressure and no evidence of acute target organ damage. However, patients presenting with symptoms should be closely monitored, and consultation with appropriate specialists may be necessary to assess for end-organ damage. Blood pressure should not be lowered too quickly or excessively, as rapid reductions can cause ischemic injury in vascular beds that have adapted to chronic hypertension. An interprofessional team approach ensures careful monitoring and coordination between clinicians, nurses, and pharmacists to individualize treatment plans and titrate medications safely, minimizing the risk of complications.
All patients with hypertension should be encouraged to attend regular outpatient follow-ups. Lifestyle changes, such as a low-salt diet, are beneficial. Interprofessional team members should emphasize the importance of medication adherence and encourage patients to monitor their blood pressure at home on a regular basis.
Media
(Click Image to Enlarge)
References
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2018 May 15:71(19):e127-e248. doi: 10.1016/j.jacc.2017.11.006. Epub 2017 Nov 13 [PubMed PMID: 29146535]
Level 1 (high-level) evidenceKeith NM, Wagener HP, Barker NW. Some different types of essential hypertension: their course and prognosis. The American journal of the medical sciences. 1974 Dec:268(6):336-45 [PubMed PMID: 4616627]
Fragoulis C, Polyzos D, Mavroudis A, Tsioufis PA, Kasiakogias A, Leontsinis I, Mantzouranis E, Kalos T, Sakalidis A, Ntalakouras J, Andrikou I, Dimitriadis K, Konstantinidis D, Thomopoulos C, Tsioufis K. One-year outcomes following a hypertensive urgency or emergency. European journal of internal medicine. 2024 Feb:120():107-113. doi: 10.1016/j.ejim.2023.10.020. Epub 2023 Oct 21 [PubMed PMID: 37872037]
Leiba A, Cohen-Arazi O, Mendel L, Holtzman EJ, Grossman E. Incidence, aetiology and mortality secondary to hypertensive emergencies in a large-scale referral centre in Israel (1991-2010). Journal of human hypertension. 2016 Aug:30(8):498-502. doi: 10.1038/jhh.2015.115. Epub 2015 Dec 17 [PubMed PMID: 26674757]
Kulkarni S, Glover M, Kapil V, Abrams SML, Partridge S, McCormack T, Sever P, Delles C, Wilkinson IB. Management of hypertensive crisis: British and Irish Hypertension Society Position document. Journal of human hypertension. 2023 Oct:37(10):863-879. doi: 10.1038/s41371-022-00776-9. Epub 2022 Nov 22 [PubMed PMID: 36418425]
Astarita A, Covella M, Vallelonga F, Cesareo M, Totaro S, Ventre L, Aprà F, Veglio F, Milan A. Hypertensive emergencies and urgencies in emergency departments: a systematic review and meta-analysis. Journal of hypertension. 2020 Jul:38(7):1203-1210. doi: 10.1097/HJH.0000000000002372. Epub [PubMed PMID: 32510905]
Level 1 (high-level) evidenceBoulestreau R, van den Born BH, Lip GYH, Gupta A. Malignant Hypertension: Current Perspectives and Challenges. Journal of the American Heart Association. 2022 Apr 5:11(7):e023397. doi: 10.1161/JAHA.121.023397. Epub 2022 Mar 15 [PubMed PMID: 35289189]
Level 3 (low-level) evidenceKhan NN, Zurayyir EJ, Alghamdi AM, Alghamdi SF, Alqahtani MA, Abdalla EM, Jurays NS, Alassiri AM, Alzahrani HA, Althabet AA. Management Strategies for Hypertensive Crisis: A Systematic Review. Cureus. 2024 Aug:16(8):e66694. doi: 10.7759/cureus.66694. Epub 2024 Aug 12 [PubMed PMID: 39262522]
Level 1 (high-level) evidenceVarounis C, Katsi V, Nihoyannopoulos P, Lekakis J, Tousoulis D. Cardiovascular Hypertensive Crisis: Recent Evidence and Review of the Literature. Frontiers in cardiovascular medicine. 2016:3():51. doi: 10.3389/fcvm.2016.00051. Epub 2017 Jan 10 [PubMed PMID: 28119918]
Pinna G, Pascale C, Fornengo P, Arras S, Piras C, Panzarasa P, Carmosino G, Franza O, Semeraro V, Lenti S, Pietrelli S, Panzone S, Bracco C, Fiorini R, Rastelli G, Bergandi D, Zampaglione B, Musso R, Marengo C, Santoro G, Zamboni S, Traversa B, Barattini M, Bruno G. Hospital admissions for hypertensive crisis in the emergency departments: a large multicenter Italian study. PloS one. 2014:9(4):e93542. doi: 10.1371/journal.pone.0093542. Epub 2014 Apr 2 [PubMed PMID: 24695800]
Ebinger JE, Liu Y, Driver M, Ji H, Bairey Merz CN, Rader F, Albert CM, Cheng S. Sex-Specific Temporal Trends in Hypertensive Crisis Hospitalizations in the United States. Journal of the American Heart Association. 2022 Feb 15:11(4):e021244. doi: 10.1161/JAHA.121.021244. Epub 2022 Jan 27 [PubMed PMID: 35083929]
McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, Christodorescu RM, Daskalopoulou SS, Ferro CJ, Gerdts E, Hanssen H, Harris J, Lauder L, McManus RJ, Molloy GJ, Rahimi K, Regitz-Zagrosek V, Rossi GP, Sandset EC, Scheenaerts B, Staessen JA, Uchmanowicz I, Volterrani M, Touyz RM, ESC Scientific Document Group. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. European heart journal. 2024 Oct 7:45(38):3912-4018. doi: 10.1093/eurheartj/ehae178. Epub [PubMed PMID: 39210715]
Paini A, Aggiusti C, Bertacchini F, Agabiti Rosei C, Maruelli G, Arnoldi C, Cappellini S, Muiesan ML, Salvetti M. Definitions and Epidemiological Aspects of Hypertensive Urgencies and Emergencies. High blood pressure & cardiovascular prevention : the official journal of the Italian Society of Hypertension. 2018 Sep:25(3):241-244. doi: 10.1007/s40292-018-0263-2. Epub 2018 Jun 18 [PubMed PMID: 29916180]
Level 2 (mid-level) evidenceWaldron FA, Benenson I, Jones-Dillon SA, Zinzuwadia SN, Adeboye AM, Eris E, Mbadugha NE, Vicente N, Over A. Prevalence and risk factors for hypertensive crisis in a predominantly African American inner-city community. Blood pressure. 2019 Apr:28(2):114-123. doi: 10.1080/08037051.2019.1568183. Epub 2019 Jan 22 [PubMed PMID: 30669866]
Peixoto AJ. Acute Severe Hypertension. The New England journal of medicine. 2019 Nov 7:381(19):1843-1852. doi: 10.1056/NEJMcp1901117. Epub [PubMed PMID: 31693807]
Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovascular and brain metabolism reviews. 1990 Summer:2(2):161-92 [PubMed PMID: 2201348]
Gallo G, Volpe M, Savoia C. Endothelial Dysfunction in Hypertension: Current Concepts and Clinical Implications. Frontiers in medicine. 2021:8():798958. doi: 10.3389/fmed.2021.798958. Epub 2022 Jan 20 [PubMed PMID: 35127755]
Rossi GP, Rossitto G, Maifredini C, Barchitta A, Bettella A, Latella R, Ruzza L, Sabini B, Seccia TM. Management of hypertensive emergencies: a practical approach. Blood pressure. 2021 Aug:30(4):208-219. doi: 10.1080/08037051.2021.1917983. Epub 2021 May 8 [PubMed PMID: 33966560]
Rossi GP, Seccia TM, Barton M, Danser AHJ, de Leeuw PW, Dhaun N, Rizzoni D, Rossignol P, Ruilope LM, van den Meiracker AH, Ito S, Hasebe N, Webb DJ. Endothelial factors in the pathogenesis and treatment of chronic kidney disease Part II: Role in disease conditions: a joint consensus statement from the European Society of Hypertension Working Group on Endothelin and Endothelial Factors and the Japanese Society of Hypertension. Journal of hypertension. 2018 Mar:36(3):462-471. doi: 10.1097/HJH.0000000000001600. Epub [PubMed PMID: 29135628]
Level 3 (low-level) evidencevan den Born BH, Lip GYH, Brguljan-Hitij J, Cremer A, Segura J, Morales E, Mahfoud F, Amraoui F, Persu A, Kahan T, Agabiti Rosei E, de Simone G, Gosse P, Williams B. ESC Council on hypertension position document on the management of hypertensive emergencies. European heart journal. Cardiovascular pharmacotherapy. 2019 Jan 1:5(1):37-46. doi: 10.1093/ehjcvp/pvy032. Epub [PubMed PMID: 30165588]
Miller JB, Hrabec D, Krishnamoorthy V, Kinni H, Brook RD. Evaluation and management of hypertensive emergency. BMJ (Clinical research ed.). 2024 Jul 26:386():e077205. doi: 10.1136/bmj-2023-077205. Epub 2024 Jul 26 [PubMed PMID: 39059997]
Slaven J, Evans M, Partyka C, Aneman A, Middleton PM. Characteristics, clinical findings and outcomes of acute aortic dissection: A comparison between an Australian emergency department and the International Registry of Acute Aortic Dissection. Emergency medicine Australasia : EMA. 2022 Dec:34(6):927-935. doi: 10.1111/1742-6723.14024. Epub 2022 May 30 [PubMed PMID: 35636964]
Boulestreau R, Śpiewak M, Januszewicz A, Kreutz R, Guzik TJ, Januszewicz M, Muiesan ML, Persu A, Sarafidis P, Volpe M, Zaleska-Żmijewska A, van den Born BH, Messerli FH. Malignant Hypertension:A Systemic Cardiovascular Disease: JACC Review Topic of the Week. Journal of the American College of Cardiology. 2024 Apr 30:83(17):1688-1701. doi: 10.1016/j.jacc.2024.02.037. Epub [PubMed PMID: 38658108]
Balahura AM, Moroi ȘI, Scafa-Udrişte A, Weiss E, Japie C, Bartoş D, Bădilă E. The Management of Hypertensive Emergencies-Is There a "Magical" Prescription for All? Journal of clinical medicine. 2022 May 31:11(11):. doi: 10.3390/jcm11113138. Epub 2022 May 31 [PubMed PMID: 35683521]
Grossman E, Messerli FH, Grodzicki T, Kowey P. Should a moratorium be placed on sublingual nifedipine capsules given for hypertensive emergencies and pseudoemergencies? JAMA. 1996 Oct 23-30:276(16):1328-31 [PubMed PMID: 8861992]
Smith M. Refractory Intracranial Hypertension: The Role of Decompressive Craniectomy. Anesthesia and analgesia. 2017 Dec:125(6):1999-2008. doi: 10.1213/ANE.0000000000002399. Epub [PubMed PMID: 28806209]
Brokmann JC, Rossaint R, Müller M, Fitzner C, Villa L, Beckers SK, Bergrath S. Blood pressure management and guideline adherence in hypertensive emergencies and urgencies: A comparison between telemedically supported and conventional out-of-hospital care. Journal of clinical hypertension (Greenwich, Conn.). 2017 Jul:19(7):704-712. doi: 10.1111/jch.13026. Epub 2017 May 30 [PubMed PMID: 28560799]
Shah M, Patil S, Patel B, Arora S, Patel N, Garg L, Agrawal S, Jacobs L, Steigerwalt SP, Martinez MW. Trends in Hospitalization for Hypertensive Emergency, and Relationship of End-Organ Damage With In-Hospital Mortality. American journal of hypertension. 2017 Jul 1:30(7):700-706. doi: 10.1093/ajh/hpx048. Epub [PubMed PMID: 28430850]
van der Merwe W, van der Merwe V. Malignant hypertension: a preventable emergency. The New Zealand medical journal. 2013 Aug 16:126(1380):39-45 [PubMed PMID: 24126748]
Writing Committee Members, Isselbacher EM, Preventza O, Hamilton Black Iii J, Augoustides JG, Beck AW, Bolen MA, Braverman AC, Bray BE, Brown-Zimmerman MM, Chen EP, Collins TJ, DeAnda A Jr, Fanola CL, Girardi LN, Hicks CW, Hui DS, Jones WS, Kalahasti V, Kim KM, Milewicz DM, Oderich GS, Ogbechie L, Promes SB, Ross EG, Schermerhorn ML, Times SS, Tseng EE, Wang GJ, Woo YJ. 2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2022 Dec 13:80(24):e223-e393. doi: 10.1016/j.jacc.2022.08.004. Epub 2022 Nov 2 [PubMed PMID: 36334952]
Level 1 (high-level) evidenceCzerny M, Grabenwöger M, Berger T, Aboyans V, Della Corte A, Chen EP, Desai ND, Dumfarth J, Elefteriades JA, Etz CD, Kim KM, Kreibich M, Lescan M, Di Marco L, Martens A, Mestres CA, Milojevic M, Nienaber CA, Piffaretti G, Preventza O, Quintana E, Rylski B, Schlett CL, Schoenhoff F, Trimarchi S, Tsagakis K, EACTS/STS Scientific Document Group. EACTS/STS Guidelines for diagnosing and treating acute and chronic syndromes of the aortic organ. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 2024 Feb 1:65(2):. pii: ezad426. doi: 10.1093/ejcts/ezad426. Epub [PubMed PMID: 38408364]
Malaisrie SC, Szeto WY, Halas M, Girardi LN, Coselli JS, Sundt TM 3rd, Chen EP, Fischbein MP, Gleason TG, Okita Y, Ouzounian M, Patel HJ, Roselli EE, Shrestha ML, Svensson LG, Moon MR, AATS Clinical Practice Standards Committee: Adult Cardiac Surgery. 2021 The American Association for Thoracic Surgery expert consensus document: Surgical treatment of acute type A aortic dissection. The Journal of thoracic and cardiovascular surgery. 2021 Sep:162(3):735-758.e2. doi: 10.1016/j.jtcvs.2021.04.053. Epub 2021 Apr 30 [PubMed PMID: 34112502]
Level 3 (low-level) evidenceHiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, Eagle KA, Hermann LK, Isselbacher EM, Kazerooni EA, Kouchoukos NT, Lytle BW, Milewicz DM, Reich DL, Sen S, Shinn JA, Svensson LG, Williams DM, American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, Society for Vascular Medicine. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with Thoracic Aortic Disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons, and Society for Vascular Medicine. Circulation. 2010 Apr 6:121(13):e266-369. doi: 10.1161/CIR.0b013e3181d4739e. Epub 2010 Mar 16 [PubMed PMID: 20233780]
Level 1 (high-level) evidenceSheth KN. Spontaneous Intracerebral Hemorrhage. The New England journal of medicine. 2022 Oct 27:387(17):1589-1596. doi: 10.1056/NEJMra2201449. Epub [PubMed PMID: 36300975]
Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, Hemphill JC 3rd, Johnson R, Keigher KM, Mack WJ, Mocco J, Newton EJ, Ruff IM, Sansing LH, Schulman S, Selim MH, Sheth KN, Sprigg N, Sunnerhagen KS, American Heart Association/American Stroke Association. 2022 Guideline for the Management of Patients With Spontaneous Intracerebral Hemorrhage: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2022 Jul:53(7):e282-e361. doi: 10.1161/STR.0000000000000407. Epub 2022 May 17 [PubMed PMID: 35579034]
Lane DA, Lip GY, Beevers DG. Improving survival of malignant hypertension patients over 40 years. American journal of hypertension. 2009 Nov:22(11):1199-204. doi: 10.1038/ajh.2009.153. Epub 2009 Aug 20 [PubMed PMID: 19696746]
Amraoui F, Van Der Hoeven NV, Van Valkengoed IG, Vogt L, Van Den Born BJ. Mortality and cardiovascular risk in patients with a history of malignant hypertension: a case-control study. Journal of clinical hypertension (Greenwich, Conn.). 2014 Feb:16(2):122-6. doi: 10.1111/jch.12243. Epub 2013 Dec 27 [PubMed PMID: 24373528]
Level 2 (mid-level) evidenceGonzález R, Morales E, Segura J, Ruilope LM, Praga M. Long-term renal survival in malignant hypertension. Nephrology, dialysis, transplantation : official publication of the European Dialysis and Transplant Association - European Renal Association. 2010 Oct:25(10):3266-72. doi: 10.1093/ndt/gfq143. Epub 2010 Mar 17 [PubMed PMID: 20299339]
Liu S, Song A, Zhou X, Kong X, Li WA, Wang Y, Liu Y. Malignant pheochromocytoma with multiple vertebral metastases causing acute incomplete paralysis during pregnancy: Literature review with one case report. Medicine. 2017 Nov:96(44):e8535. doi: 10.1097/MD.0000000000008535. Epub [PubMed PMID: 29095319]
Level 3 (low-level) evidenceCremer A, Amraoui F, Lip GY, Morales E, Rubin S, Segura J, Van den Born BJ, Gosse P. From malignant hypertension to hypertension-MOD: a modern definition for an old but still dangerous emergency. Journal of human hypertension. 2016 Aug:30(8):463-6. doi: 10.1038/jhh.2015.112. Epub 2015 Nov 19 [PubMed PMID: 26582411]
Shantsila A, Shantsila E, Beevers DG, Lip GYH. Predictors of 5-year outcomes in malignant phase hypertension: the West Birmingham Malignant Hypertension Registry. Journal of hypertension. 2017 Nov:35(11):2310-2314. doi: 10.1097/HJH.0000000000001446. Epub [PubMed PMID: 28622157]
Siddiqi TJ, Usman MS, Rashid AM, Javaid SS, Ahmed A, Clark D 3rd, Flack JM, Shimbo D, Choi E, Jones DW, Hall ME. Clinical Outcomes in Hypertensive Emergency: A Systematic Review and Meta-Analysis. Journal of the American Heart Association. 2023 Jul 18:12(14):e029355. doi: 10.1161/JAHA.122.029355. Epub 2023 Jul 8 [PubMed PMID: 37421281]
Level 1 (high-level) evidence