Introduction
Finger joint dislocations are common hand injuries that may occur at the metacarpophalangeal (MCP), proximal interphalangeal (PIP), or distal interphalangeal (DIP) joints, with varying frequency. The complex and extensive anatomy of the finger permits coordinated digital function. Each digit has 3 primary joints: the MCP, PIP, and DIP. The MCP joint is a condyloid articulation between the metacarpal and proximal phalanx. The PIP joint is a hinge joint between the proximal and middle phalanges. The DIP is also a hinge joint between the middle and distal phalanges.
The range of motion of these joints allows for flexion and extension, which provides grasping, pinching, clawing, and reaching functions of the fingers. The MCP joint typically achieves 90° of flexion; the PIP and DIP often reach 100° and 80°, respectively. While flexion and extension of the digit are possible at the MCP joint, this joint can also perform adduction, abduction, and circumduction.[1] See Image. First Metacarpophalangeal (MCP) Joint Dorsal Dislocation.
The finger joints have important soft tissue stabilizers that provide necessary support during motion.[2] These joint stabilizers are both static and dynamic. Static stabilizers consist of noncontractile tissues, including the radial and ulnar collateral ligaments, volar plate, dorsal capsule, and sagittal bands, which surround the MCP joint. The volar plate is a crucial stabilizer, as it reinforces the volar aspect of the joint capsule and maintains stability by preventing hyperextension of the finger joints.[3] The collateral ligaments provide stabilization against radial and ulnar (lateral) deviation of the interphalangeal joints.
Sagittal bands encircle the MCP joint to keep the extensor tendon centralized. Dynamic stabilizers include extrinsic and intrinsic tendons and muscles, and 3 important dynamic stabilizers are the central slip, terminal tendon, and flexor tendons. The central slip is found dorsally and allows for PIP joint extension, while the terminal tendon inserts at the dorsal base of the distal phalanx and facilitates DIP joint extension. The flexor digitorum profundus and flexor digitorum superficialis tendons serve as additional restraints against hyperextension of the DIP and PIP joints, respectively.[4]
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Finger dislocations typically result from a direct blow to the digit or a fall onto an outstretched hand. These may occur in the dorsal, volar, or lateral planes, and they are categorized according to the position of the distal bone relative to the more proximal bone.[5] As such, finger dislocations can be classified as:
- Dorsal dislocations
- Volar dislocations
- Lateral dislocations
- Either radial or ulnar
- Rotatory dislocations
- Commonly occurs with a volar dislocation of the PIP joint with a rotational component due to rupture of only 1 collateral ligament
- Fracture-dislocations
- Also occur, but are beyond the scope of this course [6]
Dislocations are further classified as either "simple," in which the articular surfaces maintain some contact between the condyles, or "complex," where there is a complete loss of contact, often accompanied by bayonet apposition and interposition of the volar plate.[7]
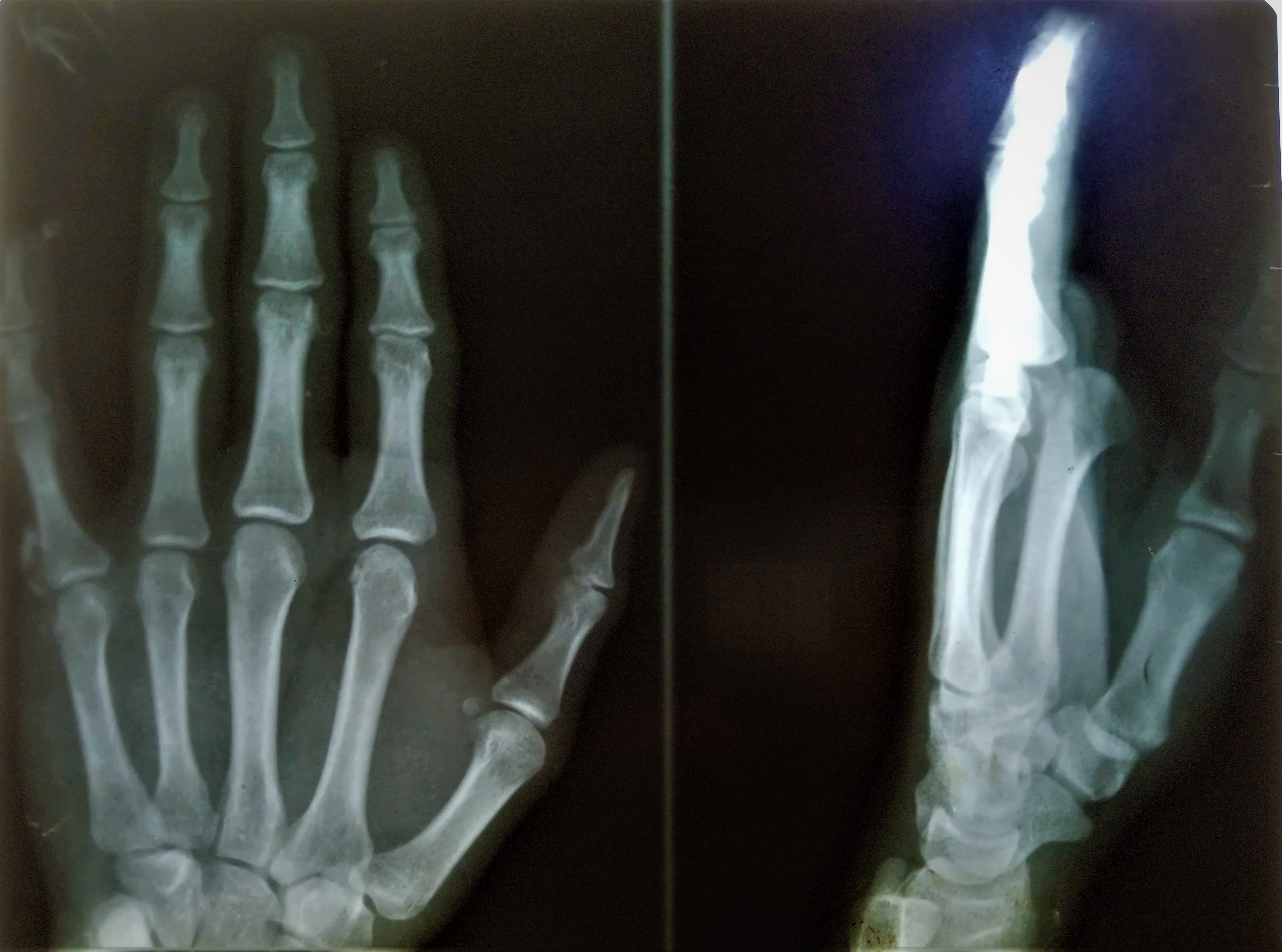
Hyperextension or high-energy axial loads at the MCP joint can result in a dislocation. However, MCP joint dislocations occur infrequently due to protection against hyperextension afforded by the volar plate and the stability against radial and ulnar deviation provided by the collateral ligaments (see Image. Metacarpophalangeal [MCP] Joint Dorsal Dislocation, Radiograph). While MCP joint dislocations most commonly occur at the index finger, dislocations at the middle finger occur more frequently when subjected to ulnar stress during hyperextension.[3] Most MCP joint dislocations are dorsal.[5][8]
Proximal interphalangeal (PIP) joint dislocations are common in athletic settings and are sometimes referred to as “coach’s finger” due to their frequent occurrence and tendency to be underestimated or improperly managed in sports environments. (see Image. Proximal Interphalangeal [PIP] Joint Dorsal Dislocation, Radiograph). Similar to MCP dislocations, PIP dislocations are typically dorsal. Dorsal dislocation results from longitudinal compression and hyperextension, commonly by a ball hitting the fingertip. These most commonly occur at the middle finger and are associated with volar plate, collateral ligament, and dorsal joint capsular injuries. Swan neck deformities may occur in dorsal dislocations from volar plate injury.
Additionally, interposition of the volar plate within the joint may occur, causing malalignment, oblique rotation, and challenging or unsuccessful reduction. Volar dislocation of the PIP joint can occur with and without rotation of the intermediate phalanx. These dislocations are infrequent and can be associated with injury to the central slip of the extensor mechanism. An untreated rupture of the central slip after a PIP joint dislocation is associated with a boutonniere deformity. Lateral PIP dislocations can also occur and involve disruption of the collateral ligaments. Finally, rotary volar dislocations may occur when the phalanx displaces and rotates around 1 collateral ligament, allowing the proximal phalanx to wedge between the lateral band and extensor mechanism. The classic lateral radiographic finding has the colloquial description of the “finger trap”.[1]
Dorsal DIP joint dislocations occur most frequently and are associated with fractures and skin injuries. (see Image. Distal Interphalangeal [DIP] Joint Dorsal Dislocation, Radiograph). They are not always associated with flexor tendon avulsions but may have an interposed volar plate causing a nonreducible dislocation. Volar DIP joint dislocations are similar to volar PIP joint dislocations, as both are associated with extensor tendon injuries. The lateral DIP joint is more likely to have postreduction instability than volar or dorsal dislocations. An isolated DIP joint dislocation without related injuries to the soft tissues or fractures is rare and is commonly managed with closed reduction and splinting.[9]
Epidemiology
Overall, dislocations of the fingers are fairly common injuries, with an estimated incidence of 11.1 per 100,000 person-years in the United States.[10] Most of these injuries involve the PIP and DIP joints, while MCP dislocations are associated with an incidence of less than 1 per 100,000 person-years annually. Most dislocations occur in adolescent or young adult men between the ages of 15 and 19 and commonly occur in basketball and football players.
History and Physical
Examiners must conduct a thorough history, which includes the mechanism of injury, hand dominance, previous finger injuries, risk factors such as Ehlers-Danlos syndrome, occupation, and recreational activities. Patients with finger dislocations typically present with joint-specific pain, associated swelling that may extend to adjacent areas, and an observable deformity at the injury site. Some dislocations are reduced by the patient or another individual before presentation, so clinicians should specifically inquire whether a reduction was attempted before evaluation.
During physical examination, the inspection should include an evaluation of any clinical deformities, skin integrity, swelling, and ecchymosis.[11] Dimpling or puckering of skin may indicate soft tissue interposition. If the examiner identifies a deformity, the examiner must also determine if there is any malrotation or angulation. To assess this, the patient is asked to make a fist (if possible) with the fingertips pointing toward the scaphoid. Overlapping or "scissoring" indicates a rotational component to the injury. Alternatively, the digital cascade can be evaluated through the tenodesis effect by passively flexing and extending both wrists.
The alignment of the fingers can then be compared. Furthermore, palpation can be used to determine the location of maximal tenderness.[5] Each joint should also be assessed for both active and passive range of motion, as tolerated by the patient.[12] Moreover, a thorough neurovascular examination is imperative in evaluating the injured hand. To identify a potential digital nerve injury (such as traction neuropraxia), the injured digit should be compared to the same digit on the unaffected hand for light touch, pinprick, and/or 2-point discrimination. On the opposite hand, the digital artery can be evaluated by comparison to an unaffected digit using capillary refill.
Stability testing of the injured joint should be performed (typically following reduction) to assess the functional competency of the stabilizing soft tissue structures. Increased laxity or gross instability on testing suggests injury to 1 or more of these structures. A dorsally directed force at the joint is used to evaluate the integrity of the volar plate, while a volarly directed force assesses the dorsal capsule and extensor coverage. Lateral stress testing should be performed with the affected joint in both full (neutral) extension and at 30° of flexion. A radially-directed force tests the ulnar collateral ligament, while an ulnarly-directed force tests the radial collateral ligament.
In addition, in the setting of a suspected (volar) PIP dislocation, the Elson test should be performed to evaluate the integrity of the central slip. This is done by placing the affected digit over the edge of a table and flexing the PIP joint to 90°. The examiner places their finger over the patient's middle phalanx and asks the patient to actively extend the digit against resistance. If the central slip is intact, the patient exhibits strong PIP extension, and the DIP joint is flaccid. However, a central slip rupture would be suspected if there is weak PIP extension while the DIP becomes rigid.
Evaluation
The standard of care for the initial evaluation of injuries to the hand is plain film imaging (see Image. Left Proximal Interphalangeal Dislocation, Radiograph). Posteroanterior (or anteroposterior), oblique, and true lateral radiographic views are necessary for each affected digit. The films must demonstrate an unobstructed view of the affected finger. Widening of the joint space may indicate soft tissue interposition (such as the volar plate). In the setting of an MCP dislocation, sesamoid entrapment strongly indicates a complex dislocation.[13] Examiners should remember that rotational deformities are more commonly diagnosed on physical examination than plain films.[5] In addition to plain radiographs, ultrasound remains an active area of investigation for its potential to detect associated fractures and tendon ruptures in finger dislocations.[14]
Treatment / Management
The treatment of MCP, PIP, and DIP joint dislocations may be nonoperative or operative, predominantly depending upon the ease of reduction and postreduction joint stability.[15][16] Before any reduction attempt, a digital nerve block using lidocaine, bupivacaine, or a similar anesthetic should be administered to provide adequate anesthesia.[17] Posttreatment splinting and/or buddy taping protocols vary by the type of dislocation, resultant stability, and clinician preference. (A1)
Metacarpophalangeal Joint Dislocation
Nonoperative management
Nonoperative management of MCP joint dislocations consists of closed reduction and splinting. The clinician can achieve closed reduction of a dorsal dislocation by applying extension and axial compression to the proximal phalanx, thereby relocating pressure over the phalangeal base to glide it into position. This approach differs from the traction technique used in PIP joint dislocations. Multiple reduction attempts should be avoided, as the inability to reduce may indicate volar plate interposition requiring open reduction.
Additionally, repeated attempts at MCP reduction have the potential complication of displacing the volar plate or flexor tendons between articular surfaces. Once reduced, a dorsal-block splint should be applied, followed by early range of motion exercises. A volar MCP dislocation is typically reduced by flexing the joint while applying a dorsally-directed force over the proximal phalanx volarly. The finger should then be splinted for approximately 3 weeks to 6 weeks, followed by an additional 2 weeks of buddy taping.
Operative management
Operative intervention is indicated for irreducible MCP joint dislocations, as volar plate involvement is highly likely in these cases. Open reduction of the MCP joint can be performed using either a dorsal or volar approach. However, the dorsal approach is preferable as it carries a lower risk of neurovascular injury. After surgery, the wrist is splinted in 30° of extension with the MCP joint in slight flexion for 2 weeks. The recommendation is that the PIP and DIP joints not be immobilized. Recovery of preinjury motion may take several weeks to months.[18]
Volar approach for MCP joint dislocation
To prevent neurovascular damage, a volar Bruner-like incision is made over the MCP joint, between the proximal and distal volar creases, while the patient is under general anesthesia. The flexor tendons are on the ulnar side, whereas the neurovascular bundle is on the radial side. The volar plate's proximal connection on the metacarpal is usually ruptured. By releasing the A1 pulley, the tension created by the muscle-tendon constriction around the metacarpal neck is released. Superficial transverse ligament, natatory ligament, and palmar fascia are then incised. The joint can be manually reduced following a longitudinal incision in the volar plate. The volar plate's free slips are wrapped around the metacarpal head and secured using sutures. A dorsal-block splint is applied following skin closure. After healing, active flexion activities are promoted. The splint is removed approximately 3 weeks later, and active extension exercises are introduced.[7]
Dorsal approach for MCP joint dislocation
Over the MCP joint, a dorsally curved incision is made either on the ulnar or radial aspect. Usually, a dorsoradial incision is made for the first and second MCP joints, but a dorsoulnar incision is preferred for the fourth and fifth MCP joints. The skin flaps are raised, protecting sensory nerve branches and longitudinal vasculature. The extensor mechanism is incised longitudinally along the extensor digitorum tendon. A capsulotomy of the MCP joint is made longitudinally. An elevator is used to shift the intervening volar plate volarly, which reduces the MCP joint. Clinical testing is performed upon reduction to assess stability. Following surgery, the MCP joint is immobilized for 2 weeks at 30° of flexion, and then dorsal-block splinting is performed for 4 weeks.[19] (B3)
The benefits of the dorsal open reduction method include adequate volar plate visibility and prevention of digital neurovascular injury. However, this procedure could require longitudinal division of the volar plate and extensor apparatus, potentially impairing MCP stability.[20] The volar open reduction method offers several benefits, including clear visibility of the MCP joint, which facilitates the surgical removal and realignment of the volar plate. In a volar approach to the MCP joint, the radial digital nerve and the neurovascular structures volar to the lumbrical muscles are at risk.[21] The dorsal approach has been shown to be safe for the open reduction of complex MCP dislocations. In this procedure, the deep transverse ligament does not need to be divided. Both approaches provide a stable MCP joint with appropriate functional outcomes.[22](B3)
Proximal Interphalangeal Joint Dislocation
Nonoperative management
For closed reduction of dorsal PIP joint dislocations, the clinician should apply slight extension with longitudinal traction and, with the other hand, apply volarly-directed pressure to the dorsal aspect of the middle phalanx. After reduction, the examiner should evaluate the joint for stability in all planes and then obtain postreduction radiographs. The normal contour of the dorsal aspect of the PIP joint on lateral plain film is "C"-shaped. If, after reduction, this contour presents a "V" shape, it may indicate persistent dorsal subluxation, which can lead to severe stiffness and post-traumatic osteoarthritis.[3] Dorsal PIP joint dislocations are often stable after reduction and are treated with buddy taping for 3 to 6 weeks. However, if unstable following reduction, a dorsal-block splint at 30° of flexion is applied. Volar PIP dislocations are the least common, but reducing the volar PIP joint dislocation is generally successful. The reduction is performed by applying mild traction with the PIP and MCP joints in flexion. After reducing the volar dislocation, an extension splint is applied for 6 to 8 weeks.
Lateral dislocations may be more likely to require operative intervention. Closed reduction requires relaxation of the extensor tendon and lateral bands through wrist extension and MCP flexion, respectively. Then, the middle phalanx is gently rotated back into position. If the lateral PIP joint reduction affords a full range of motion without subluxation, then the joint is not grossly unstable. Splinting and reassessment in 2 to 3 weeks are recommended in these cases, although buddy taping has also been described as an alternative approach. A recent randomized controlled trial compared buddy taping versus aluminum digital splinting treatment of hyperextension-type injuries and found no difference in strength, pain, or function at 3 weeks. However, the buddy tape did show an earlier range of motion and decreased edema.[23](A1)
Operative management
Unstable dislocations require referral for orthopedic evaluation and possible open treatment. Indications for operative intervention for PIP joint dislocations include persistent joint instability, significant ligament/soft tissue/tendon injuries, or dislocations that are not reducible.[24]
Dorsal approach for PIP joint dislocation
For volar PIP dislocations, the dorsal approach is indicated.[25] Midline longitudinal, curvilinear, and lazy "S" incisions are used for the dorsal approach of the PIP joint. Full-thickness skin flaps are elevated, preserving the sensory nerve branches and the longitudinal superficial vasculature, while the transverse vein may be ligated. After exposing the extensor aponeurosis, there are 3 ways to approach the PIP joint capsule: between the central and lateral slips, splitting the central slip (Swanson approach), and flap elevation of the central slip (Chamay approach).[26][27] A capsulotomy is made transversely, preserving the central slip and extensor tendons.
Volar approach for PIP joint dislocation
A Bruner or zigzag incision is made between the flexor crease and the PIP joint. After raising thick skin flaps, flexor pulleys are released (C1, A3, C2). The A2 and A4 pulleys should not be incised as they could lead to bowstringing of the flexor tendons. The flexor tendons are then retracted, and the joint capsule is incised. The volar plate is mobilized, the joint is reduced, and a layered closure is performed.[28](B2)
Lateral approach for PIP joint dislocation
A mid-axial incision is made over the PIP joint, and a plane is developed between the dorsal extensor tendon and the volar digital neurovascular bundle. The transverse retinacular and collateral ligaments are incised to expose the PIP joint, which is later repaired after reduction.[29]
Distal Interphalangeal Joint Dislocation
Nonoperative management
Dorsal dislocations are reduced with longitudinal traction and a volarly-directed force on the dorsal distal phalanx with the DIP joint in flexion. Often, the reduction occurs with relative ease, followed by splinting of the DIP joint in 10° to 20° of flexion for 2 to 3 weeks if persistent instability persists.[9] A dorsally-directed force at the distal phalanx, coupled with traction, is used to reduce a volar DIP dislocation, typically followed by 6 weeks of extension splinting.
Operative management
Irreducible dislocations are typically due to volar plate (for dorsal dislocations), flexor digitorum profundus (for open dorsal dislocations), or terminal tendon (for volar dislocations) interposition and require surgical intervention. A zigzag or mid-axial incision is made centered over the DIP joint. The entrapped volar plate, flexor digitorum profundus, or terminal tendon, is mobilized to reduce the DIP joint. After confirming concentric reduction and stability, range of motion exercises are initiated immediately after operative reduction.
Differential Diagnosis
The differential diagnosis for finger dislocations includes:
- Fracture-dislocation
- Isolated collateral ligament injuries/sprains
- Boutonniere or pseudo-Boutonniere deformity
- Mallet finger
- Swan neck deformity
- Dupuytren contracture
Prognosis
The prognosis for finger dislocations varies depending on the joint and injury characteristics. MCP joint dislocations often require operative intervention due to the complexity of the surrounding anatomy, and recovery to preinjury range of motion may take several months to achieve.[18] In contrast, most PIP joint dislocations are stable following reduction; however, lateral PIP dislocations can present with ongoing instability and may require additional management. Isolated DIP joint dislocations are rare, but similar to PIP injuries, lateral DIP dislocations may also demonstrate persistent instability following reduction.[9]
Complications
Complications for finger dislocations include:
- Chronic stiffness
- Persistent pain
- Post-traumatic arthritis
- Residual deformities
- Persistent swelling
- Loss of hand function
- Overtreatment
- This includes prolonged splinting and multiple attempts at reduction of volar PIP joint dislocations, which increases the likelihood of volar plate scarring and flexion contractures.
Postoperative and Rehabilitation Care
After the reduction of simple dislocations, early range of motion is permitted if joint stability has been restored. In the setting of a dorsal dislocation, a dorsal extension blocking splint may be needed to restrict extension past neutral. After the reduction of complex dislocations, a few weeks of joint immobilization is performed in 30° of flexion with a removable dorsal extension blocking splint. Gentle mobilization and range of motion exercises are started intermittently. Following the removal of the splint, several exercises are started: fist-making, finger lifting, passive stretching, full range of motion, and eccentric exercises to strengthen the intrinsic and extrinsic muscles.[23][30]
Deterrence and Patient Education
Finger joint dislocations are common injuries that can occur following a fall or other form of direct digital trauma. Patients with a gross deformity or finger instability should seek prompt care from a clinician. Concentric reduction of the dislocated joint should be performed acutely to mitigate the risk of chronic pain, stiffness, swelling, and post-traumatic arthritis.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)

Proximal Interphalangeal (PIP) Joint Dorsal Dislocation, Radiograph. PIP joint dislocations are common in athletic settings and are sometimes referred to as “coach’s finger” due to their frequent occurrence and tendency to be underestimated or improperly managed in sports environments.
Contributed by M Taqi, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Prucz RB, Friedrich JB. Finger joint injuries. Clinics in sports medicine. 2015 Jan:34(1):99-116. doi: 10.1016/j.csm.2014.09.002. Epub 2014 Nov 25 [PubMed PMID: 25455398]
Lapegue F, André A, Lafourcade F, Filliole A, Lambeaux C, Van VT, Adamski E, Bachour R, Goumarre C, Chiavassa H, Faruch Bilfeld M, Sans N. Finger Sprains, Ultrasound Anatomy, and Pathology of Finger Ligaments. Seminars in musculoskeletal radiology. 2024 Dec:28(6):694-707. doi: 10.1055/s-0044-1791732. Epub 2024 Nov 19 [PubMed PMID: 39561751]
Sundaram N, Bosley J, Stacy GS. Conventional radiographic evaluation of athletic injuries to the hand. Radiologic clinics of North America. 2013 Mar:51(2):239-55. doi: 10.1016/j.rcl.2012.09.015. Epub [PubMed PMID: 23472589]
Minami A, An KN, Cooney WP 3rd, Linscheid RL, Chao EY. Ligament stability of the metacarpophalangeal joint: a biomechanical study. The Journal of hand surgery. 1985 Mar:10(2):255-60 [PubMed PMID: 3980940]
Hile D, Hile L. The emergent evaluation and treatment of hand injuries. Emergency medicine clinics of North America. 2015 May:33(2):397-408. doi: 10.1016/j.emc.2014.12.009. Epub 2015 Feb 26 [PubMed PMID: 25892728]
Hubbard LF. Metacarpophalangeal dislocations. Hand clinics. 1988 Feb:4(1):39-44 [PubMed PMID: 3277978]
An MT, Kelley JP, Fahrenkopf MP, Kelpin JP, Adams NS, Do V. Complex Metacarpophalangeal Dislocation. Eplasty. 2020:20():ic3 [PubMed PMID: 32499843]
Kabbani KT, Dimos K, Kosmas D, Kampani N, Papathanasiou G, Tsiomita E, Chouskoglou M. Volar Metacarpophalangeal Dislocation of Fingers: Review of the Literature. Journal of hand surgery global online. 2021 Jul:3(4):228-232. doi: 10.1016/j.jhsg.2021.04.001. Epub 2021 May 2 [PubMed PMID: 35415557]
Wang QC, Johnson BA. Fingertip injuries. American family physician. 2001 May 15:63(10):1961-6 [PubMed PMID: 11388710]
Golan E, Kang KK, Culbertson M, Choueka J. The Epidemiology of Finger Dislocations Presenting for Emergency Care Within the United States. Hand (New York, N.Y.). 2016 Jun:11(2):192-6. doi: 10.1177/1558944715627232. Epub 2016 Feb 19 [PubMed PMID: 27390562]
Buruian A, Gameiro M. Stepladder Dislocation of the Finger. The New England journal of medicine. 2024 Jan 4:390(1):e2. doi: 10.1056/NEJMicm2302974. Epub 2023 Dec 30 [PubMed PMID: 38165086]
Gaston RG, Chadderdon C. Phalangeal fractures: displaced/nondisplaced. Hand clinics. 2012 Aug:28(3):395-401, x. doi: 10.1016/j.hcl.2012.05.032. Epub 2012 Jun 26 [PubMed PMID: 22883890]
Xu J, Han L, Zhang B, Cao S, Zhu D, Yin Z, Gong K, Zhan H. The Application of Sesamoid Position in Diagnosing Thumb Metacarpophalangeal Joint Dorsal Dislocation: A Retrospective Study. Orthopaedic surgery. 2024 Apr:16(4):984-988. doi: 10.1111/os.14001. Epub 2024 Feb 4 [PubMed PMID: 38311800]
Level 2 (mid-level) evidenceTayal VS, Antoniazzi J, Pariyadath M, Norton HJ. Prospective use of ultrasound imaging to detect bony hand injuries in adults. Journal of ultrasound in medicine : official journal of the American Institute of Ultrasound in Medicine. 2007 Sep:26(9):1143-8 [PubMed PMID: 17715307]
Stannard JT, Stannard JP. Fractures and Dislocations on the Playing Field: Which Are Emergent and What to Do? Clinics in sports medicine. 2023 Jul:42(3):515-524. doi: 10.1016/j.csm.2023.02.012. Epub [PubMed PMID: 37208062]
Hunt TJ, Powlan FJ, Renfro KN, Polmear M, Macias RA, Dunn JC, Wells ME. Common Finger Injuries: Treatment Guidelines for Emergency and Primary Care Providers. Military medicine. 2024 May 18:189(5-6):988-994. doi: 10.1093/milmed/usad022. Epub [PubMed PMID: 36734106]
Yin ZG, Zhang JB, Kan SL, Wang P. A comparison of traditional digital blocks and single subcutaneous palmar injection blocks at the base of the finger and a meta-analysis of the digital block trials. Journal of hand surgery (Edinburgh, Scotland). 2006 Oct:31(5):547-55 [PubMed PMID: 16930788]
Level 1 (high-level) evidenceCalfee RP, Sommerkamp TG. Fracture-dislocation about the finger joints. The Journal of hand surgery. 2009 Jul-Aug:34(6):1140-7. doi: 10.1016/j.jhsa.2009.04.023. Epub [PubMed PMID: 19643295]
Mahajan NP, Patil TC, Sangma S. Management of Complex Kaplan's dislocation by Open Dorsal Approach - A Case Report. Journal of orthopaedic case reports. 2021 Nov:11(11):84-87. doi: 10.13107/jocr.2021.v11.i11.2526. Epub [PubMed PMID: 35415108]
Level 3 (low-level) evidenceKAPLAN EB. Dorsal dislocation of the metacarpophalangeal joint of the index finger. The Journal of bone and joint surgery. American volume. 1957 Oct:39-A(5):1081-6 [PubMed PMID: 13475407]
Dinh P, Franklin A, Hutchinson B, Schnall SB, Fassola I. Metacarpophalangeal joint dislocation. The Journal of the American Academy of Orthopaedic Surgeons. 2009 May:17(5):318-24 [PubMed PMID: 19411643]
Barry K, McGee H, Curtin J. Complex dislocation of the metacarpo-phalangeal joint of the index finger: a comparison of the surgical approaches. Journal of hand surgery (Edinburgh, Scotland). 1988 Nov:13(4):466-8 [PubMed PMID: 3249153]
Level 3 (low-level) evidencePaschos NK, Abuhemoud K, Gantsos A, Mitsionis GI, Georgoulis AD. Management of proximal interphalangeal joint hyperextension injuries: a randomized controlled trial. The Journal of hand surgery. 2014 Mar:39(3):449-54. doi: 10.1016/j.jhsa.2013.11.038. Epub 2014 Feb 4 [PubMed PMID: 24503231]
Level 1 (high-level) evidenceKolovich GP, Heifner JJ. Proximal interphalangeal joint dislocations and fracture-dislocations. The Journal of hand surgery, European volume. 2023 Sep:48(2_suppl):27S-34S. doi: 10.1177/17531934231183259. Epub [PubMed PMID: 37704028]
Cheah AE, Yao J. Surgical Approaches to the Proximal Interphalangeal Joint. The Journal of hand surgery. 2016 Feb:41(2):294-305. doi: 10.1016/j.jhsa.2015.11.013. Epub 2015 Dec 18 [PubMed PMID: 26708513]
Swanson AB, Maupin BK, Gajjar NV, Swanson GD. Flexible implant arthroplasty in the proximal interphalangeal joint of the hand. The Journal of hand surgery. 1985 Nov:10(6 Pt 1):796-805 [PubMed PMID: 4078262]
Chamay A. A distally based dorsal and triangular tendinous flap for direct access to the proximal interphalangeal joint. Annales de chirurgie de la main : organe officiel des societes de chirurgie de la main. 1988:7(2):179-83 [PubMed PMID: 3190311]
Lin HH, Wyrick JD, Stern PJ. Proximal interphalangeal joint silicone replacement arthroplasty: clinical results using an anterior approach. The Journal of hand surgery. 1995 Jan:20(1):123-32 [PubMed PMID: 7722251]
Level 2 (mid-level) evidenceGreen SM, Posner MA, Garay A. Silicone rubber arthroplasty of the proximal interphalangeal joint: dorsal and lateral approaches. Seminars in arthroplasty. 1991 Apr:2(2):130-8 [PubMed PMID: 10149611]
DeDeugd CM, Rizzo M. Surgical Exposure of the Proximal Interphalangeal Joint. Hand clinics. 2018 May:34(2):127-138. doi: 10.1016/j.hcl.2017.12.003. Epub [PubMed PMID: 29625633]