Anatomy, Abdomen and Pelvis: Falciform Ligament
Anatomy, Abdomen and Pelvis: Falciform Ligament
Introduction
The liver is an essential organ that occupies the right upper quadrant of the abdomen. This structure is supported by the hepatic veins, which open into the inferior vena cava, as well as by intraabdominal pressure and peritoneal ligaments. The liver is covered by visceral peritoneum, which reflects onto adjacent viscerae and the abdominal wall as peritoneal ligaments.
The falciform ligament is a bilayered, sickle-shaped fold of parietal peritoneum that extends from the anterior abdominal wall to the inferior border and anterior surface of the liver. This fibrous band serves as a crucial landmark during minimally invasive and laparoscopic abdominal procedures. This ligament may also be used as a patch or flap for reconstruction or repair of nearby structures.
During surgery, the falciform may be seen drooping from the liver hilum. The structure attaches to the liver between the right and left lobes and to the inferior diaphragmatic surface. The ligament's free, inferior border contains the paraumbilical veins and the round ligament of the liver (ligamentum teres hepatis), which runs along a fissure between the inferior surfaces of the right and left lobes. To avoid confusion, the shorthand “round ligament” here refers specifically to the round ligament of the liver, not the round ligament of the uterus.
The paraumbilical veins become more prominent and patent in portal hypertension, when the portal vein is engorged with blood that cannot fully enter the liver. If severe, these veins form a caput medusae—engorged vessels surrounding the umbilicus. Caput medusae is a hallmark of portal hypertension and advanced liver dysfunction, as seen in end-stage liver disease.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The falciform ligament forms a double-layered extension of the parietal peritoneum that arises from the anterior abdominal wall and divides the liver into asymmetric left and right lobes (see Image. Liver Segmental Anatomy and the Couinaud System).[1][2] This ligament consists of 2 margins, 2 surfaces, an apex, and a base.
Margins
The ventral (anterior) margin extends from the umbilicus to the inferior surface of the diaphragm, reflecting onto the anterosuperior surface of the liver.[3] This segment attaches marginally to the right side of the midline on the anterior abdominal wall.[4] The dorsal (posterior) margin, known as the free margin, hangs freely within the peritoneal cavity and contains the round ligament of the liver along with the paraumbilical vein.
The round ligament, a remnant of the left umbilical vein, extends from the umbilicus to the inferior border of the liver.[5][6] This ligament attaches at a notch on the inferior border of the liver and continues as the ligamentum venosum, the remnant of the ductus venosus, located on the posterior liver surface.[7] The groove for the ligamentum venosum extends to the groove for the inferior vena cava. The paraumbilical vein drains blood from the skin surrounding the umbilicus into the left portal vein within the falciform ligament.[8]
Layers
The falciform ligament remains freely movable as it hangs into the greater sac of the peritoneal cavity, suspended from the anterior abdominal wall (see Image. Axial Anatomy of the Upper Abdomen).[9] Both layers of the ligament form an incomplete partition within the greater sac.[10] The right and left layers converge at the free posterior margin, enclosing the ligamentum teres and paraumbilical veins.[11][12] Near the liver, both layers attach firmly to the anterior surface, constituting the base of the ligament.
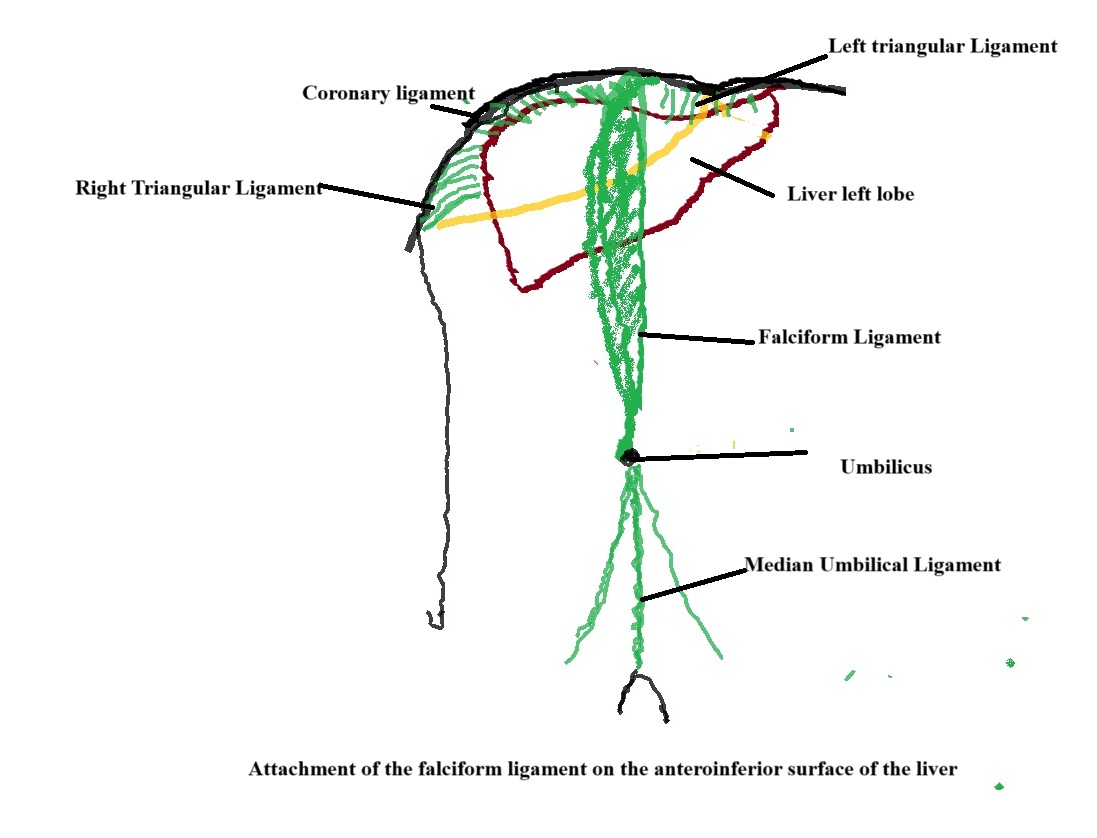
The right layer continues horizontally along the anterior margin as the peritoneal lining of the anterior abdominal wall.[13] This portion extends as parietal peritoneum along the right anterolateral abdominal wall and forms the right paracolic gutter before transitioning into the visceral peritoneum covering the ascending colon.[14] Approaching the liver, the right layer becomes the visceral peritoneum, which lines the anterosuperior surface of the liver.[15] This layer then forms the superior layer of the coronary ligament and reflects onto the diaphragm as the right triangular ligament.[16] The region between the superior and inferior layers of the coronary ligament lacks peritoneal attachment, creating the bare area of the liver (see Image. Falciform Ligament Attachment on the Anteroinferior Liver Surface).
The left layer extends horizontally in the lower abdomen as the parietal peritoneum lining the left anterior abdominal wall, left anterolateral abdominal wall, and left paracolic gutter. In the upper abdomen, this section transitions into the visceral peritoneum, which covers the anterior surface of the left lobe of the liver.[17] The left layer then continues over the superior surface of the liver and reflects onto the diaphragm to form the left triangular ligament.[18][19]
The falciform ligament forms an apex at the umbilical level on the anterior abdominal wall. The ligament attaches superiorly as a base to the anterosuperior surface of the liver.[20]
Embryology
The falciform ligament derives from the ventral mesentery attached to the ventral border of the foregut.[21][22] The primitive gut develops from the endoderm following lateral folding of the embryo, which remains surrounded by the splanchnopleuric mesoderm.[23][24] The primitive gut divides into foregut, midgut, and hindgut segments based on blood supply and the structures formed from each region.[25] The liver arises from the caudal portion of the foregut.
The intraembryonic mesoderm, located between the ventral wall of the embryo and the ventral border of the primitive gut, is designated as the ventral mesogastrium. In contrast, the mesoderm between the dorsal border of the primitive gut and the dorsal wall of the embryo forms the dorsal mesogastrium. The development of the liver at the ventral border of the foregut splits the ventral mesogastrium into 2 parts. The portion between the ventral abdominal wall and the liver develops into the falciform ligament, whereas the area between the liver and the ventral border of the foregut forms the lesser omentum, including the hepatogastric and hepatoduodenal parts.[26] Enlargement of the liver and rotation of the foregut during development stretch the ventral mesogastrium.[27][28]
During embryological development, the umbilical vein forms from the placenta to the sinus venosus through the umbilical cord.[29] The umbilical vein courses through the ventral mesogastrium to reach the developing inferior vena cava.[30] The right umbilical vein begins degenerating by the 4th week and completes degeneration by the 7th week of embryological life.[31][32] The left umbilical vein persists throughout embryological life, carrying oxygenated blood from the placenta to the inferior vena cava.[33] Postnatally, this vein degenerates and remains as the round ligament of the liver, also known as the ligamentum teres.
Blood Supply and Lymphatics
Blood Supply
The blood supply of the falciform ligament may be divided into 2 groups: superior and inferior. The superior group consists of vessels originating from the median part of the diaphragm, supplying the liver lobules covered by the falciform ligament. The inferior group is composed of vessels associated with the umbilical and paraumbilical veins, which supply and drain the lower portion of the falciform ligament and adjacent anterior abdominal wall.
Superior group
Arterial contributions to the superior group include the superior thoracic artery, the inferior phrenic artery, and branches of the internal thoracic artery. Specifically, the superior falciform artery and the xiphoid branch, both branches of the internal thoracic artery, provide vascular supply to this region. These arteries run along the falciform ligament’s attachment to the liver, where they anastomose with the inferior falciform artery.[34][35]
Venous drainage of the superior portion involves the internal thoracic and inferior phrenic veins. The superior falciform ligament veins drain the liver lobules beneath the ligament, passing through the median diaphragm and emptying into the internal thoracic vein. A peripheral branch of the left portal vein also extends into the superior falciform ligament after piercing the superior liver surface, eventually draining into the internal thoracic vein. These veins enlarge significantly in cases of portal hypertension or portal vein obstruction.[36][37]
Inferior group
The inferior portion of the falciform ligament receives venous blood primarily from the umbilical and paraumbilical veins. The paraumbilical vein drains the skin surrounding the umbilicus and the anterior abdominal wall, traveling alongside the umbilical vein through the inferior segment of the falciform ligament. At their origin, these veins connect with the epigastric and abdominal cutaneous veins, while the paraumbilical vein also communicates with the intrahepatic left portal vein at the ligament’s attachment.[38]
During embryological development, the umbilical vein carries oxygenated blood from the placenta to the fetal circulation via the ductus venosus and hepatic sinusoids. Postnatally, remnants of the umbilical vein persist within the falciform ligament as the ligamentum teres. In cases of portal hypertension, both the umbilical and paraumbilical veins recanalize and become engorged.[39][40]
Arterial supply to the inferior falciform ligament arises from a branch of the middle, left hepatic artery, or both, coursing along the ligament’s anterior margin toward the umbilicus. This artery also provides blood to the skin around the umbilicus and forms anastomoses with branches of the internal thoracic and superior thoracic arteries. The xiphoid artery, a middle terminal branch of the internal thoracic artery, anastomoses with the falciform ligament artery and penetrates the properitoneal fat. Some researchers refer to this artery as the "ensiform artery."[41]
Lymphatic Supply
The superficial lymphatics of the liver drain lymph from the falciform ligament. The close anatomical association with the liver enables infections and malignancies to spread to the falciform ligament via its blood supply or lymphatic pathways.[42] The porta hepatis, located in a fissure on the inferior aspect of the far left side of the right lobe, carries the neurovascular bundle, including the common hepatic duct, proper hepatic artery, hepatic portal vein, and autonomic axons into the liver. Due to its proximity to the round ligament of the liver, infections or carcinomas originating in the porta hepatis may extend to the falciform ligament. Moreover, the superficial lymphatics of the liver may transport infections or malignant cells from adjacent structures, facilitating seeding of the falciform ligament.
Nerves
Postsynaptic sympathetic nerve fibers from the hepatic plexus reach the falciform ligament via the vascular structures despite the absence of direct nerves associated with the ligament.[43] This indirect innervation allows the falciform ligament to participate in autonomic regulation related to hepatic blood flow and function.
Muscles
The falciform ligament contains no skeletal or smooth muscle fibres. However, associations with surrounding skeletal musculature occur, as the ligament connects to the inferior surface of the thoracic diaphragm and runs along the posterior sheath of the right rectus abdominis muscle, extending caudally as far as the umbilicus.
Physiologic Variants
Physiological variants of the falciform ligament are very rare. A few case reports describe obliteration of the falciform ligament, resulting in the absence of the fissure that the ligament typically creates in the liver. Anatomic variants also involve structures contained within the falciform ligament, such as paraumbilical veins. Most variants lack clinical significance and are typically incidental findings during surgery or imaging performed for unrelated diagnoses.[44][45][46]
Surgical Considerations
The falciform ligament serves as a key anatomical landmark during abdominal surgeries, including minimally invasive techniques. The hepatic veins, which drain into the inferior vena cava and remain hidden on the liver’s bare surface, lie immediately inferior to the falciform ligament. The round ligament, located in the falciform ligament’s free margin, extends to the umbilicus and serves as a vital landmark for the inner anterior abdominal wall. This ligament also provides an important reference point during gallbladder surgeries.
Falciform Ligament Use in Reconstructive Surgery
The falciform ligament has been utilized as a flap for reconstructing or repairing adjacent structures due to several advantages. Harvesting this fibrous structure requires no separate incision, reducing donor site morbidity. The ligament’s availability and mobility facilitate surgical manipulation. In emergencies or complications, the falciform ligament offers a convenient repair option for damaged viscera. This technique proves more cost-effective compared to synthetic graft materials.
Falciform Ligament Flap in Liver Resection
Following liver resection, the falciform ligament serves as a surgical flap in minimal access surgery, both laparoscopic and robotic, for various pathologies, including hepatocellular carcinoma. This method demonstrates superiority over conventional techniques lacking the flap. The ligament effectively seals the resection surface and provides a cost-efficient alternative to artificial or commercially available hemostatic agents.[47][48]
Use in Inferior Vena Cava Reconstruction
Malignant tumours of abdominal viscera, such as renal cell carcinoma, may invade the inferior vena cava, necessitating resection of the vessel and its tributaries. The falciform ligament can serve as an autologous graft to repair or reconstruct the inferior vena cava and its associated veins, including the hepatic vein.[49][50]
Repair of Duodenal Perforation
The falciform ligament presents a favorable alternative to the omentum for repairing perforated duodenal ulcers. This approach is associated with fewer intraoperative and postoperative complications than the alternative.[51][52][53]
Management of Hiatal and Esophageal Hernias
The falciform ligament flap has been used as an anchoring sleeve within the abdomen in treating hiatal and esophageal hernias. This method has yielded acceptable results without compromising the blood supply.[54][55][56][57]
Control of Postpancreatectomy Hemorrhage
The falciform ligament flap has been used effectively to control bleeding in postpancreatectomy hemorrhage. Surgical outcomes have been comparable to those achieved with conventional methods.[58][59]
Clinical Significance
In patients with portal hypertension, the falciform ligament undergoes vascular recanalisation. Venous congestion caused by increased portal pressure directs blood toward the anterior abdominal wall. As blood accumulates within the falciform ligament, periumbilical bruising becomes evident. Progressive portal hypertension results in the development of caput medusae, characterized by engorged and distended superficial epigastric and periumbilical veins on the anterior abdominal surface. Visualisation of this clinical feature should raise suspicion for portal hypertension.[60][61][62]
Several rare pathologies involving the falciform ligament have been documented, including cyst formation, infarction, internal herniation, torsion, and malignancy such as clear cell carcinoma. In some cases, the falciform ligament has served as a conduit for the drainage of pus or abscesses originating from the liver.[63][64][65][66][67][68]
Other Issues
The falciform ligament can be a cause of acute abdomen in select patients under specific circumstances.[69] Case reports have described falciform ligament necrosis as a rare but significant cause.[70] Documented pathologies also include hematomas, abscesses, and lipomas.[71][72][73][74] The most frequently encountered conditions affecting the falciform ligament are cysts, tumors, and vascular engorgement resulting from portal hypertension secondary to cirrhosis, Budd-Chiari syndrome, or malignancy. Congenital anomalies arising during embryological development may also predispose individuals to internal hernias involving the falciform ligament.[75]
Media
(Click Image to Enlarge)
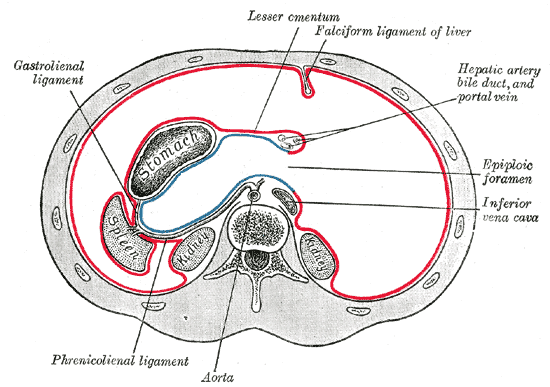
Axial Anatomy of the Upper Abdomen. Illustrated cross-sectional view showing the falciform ligament, lesser omentum, gastrolienal ligament, phrenicolienal ligament, epiploic foramen, hepatic artery, bile duct, portal vein, aorta, and inferior vena cava.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
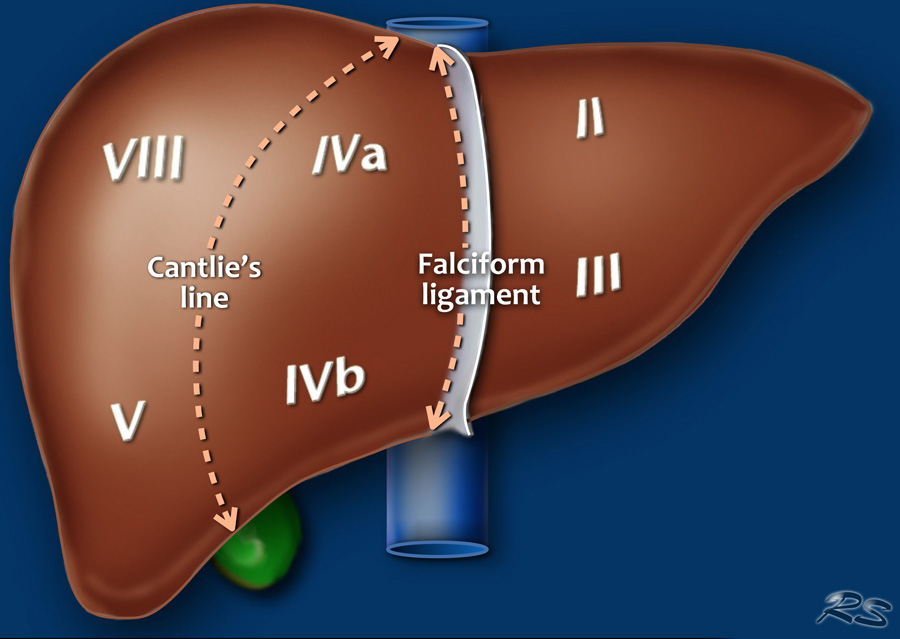
Liver Segmental Anatomy and the Couinaud System. Frontal illustration of the liver showing segmental divisions according to the Couinaud classification. Segments VI and VII are not visible due to their posterior position. The Cantlie line and the falciform ligament are labeled as key anatomical landmarks.
Contribution by Robin Smithuis and the Radiology Assistant
(Click Image to Enlarge)
References
Meyers MA. Dynamic radiology of the retroperitoneum. Normal and pathologic anatomy. Acta gastro-enterologica Belgica. 1983 Jul-Aug:46(7-8):273-88 [PubMed PMID: 6670453]
Vernon H, Wehrle CJ, Alia VSK, Kasi A. Anatomy, Abdomen and Pelvis: Liver. StatPearls. 2025 Jan:(): [PubMed PMID: 29763190]
Ibukuro K, Fukuda H, Tobe K, Akita K, Takeguchi T. The vascular anatomy of the ligaments of the liver: gross anatomy, imaging and clinical applications. The British journal of radiology. 2016 Aug:89(1064):20150925. doi: 10.1259/bjr.20150925. Epub 2016 May 10 [PubMed PMID: 27163944]
Warren LR, Chandrasegaram MD, Madigan DJ, Dolan PM, Neo EL, Worthley CS. Falciform ligament abscess from left sided portal pyaemia following malignant obstructive cholangitis. World journal of surgical oncology. 2012 Dec 22:10():278. doi: 10.1186/1477-7819-10-278. Epub 2012 Dec 22 [PubMed PMID: 23259725]
Level 3 (low-level) evidenceKozadinos A, Mylonakis A, Bekos F, Kydonakis N, Korovesis G, Kastanaki P, Despotidis M, Chrysikos D, Troupis T. The Development of the Umbilical Vein and Its Anatomical and Clinical Significance. Cureus. 2025 Feb:17(2):e79712. doi: 10.7759/cureus.79712. Epub 2025 Feb 26 [PubMed PMID: 40161047]
Meyers MA. Distribution of intra-abdominal malignant seeding: dependency on dynamics of flow of ascitic fluid. The American journal of roentgenology, radium therapy, and nuclear medicine. 1973 Sep:119(1):198-206 [PubMed PMID: 4744725]
Sidhu PS, Lui F. Embryology, Ductus Venosus. StatPearls. 2025 Jan:(): [PubMed PMID: 31613539]
Joseph A, Scharbach S, Samant H. Anatomy, Anterolateral Abdominal Wall Veins. StatPearls. 2024 Jan:(): [PubMed PMID: 29939686]
Solomon A, Rubinstein Z. Importance of the falciform ligament, ligamentum teres and splenic hilus in the spread of malignancy as demonstrated by computed tomography. Gastrointestinal radiology. 1984:9(1):53-6 [PubMed PMID: 6724241]
Ambrosetti MC, Bariani M, Zamboni GA, Valletta R, Bonatti M. The Many Faces of the Angry Peritoneum. Diagnostics (Basel, Switzerland). 2025 May 3:15(9):. doi: 10.3390/diagnostics15091163. Epub 2025 May 3 [PubMed PMID: 40361981]
Jelinek LA, Marietta M, Jones MW. Surgical Access Incisions. StatPearls. 2025 Jan:(): [PubMed PMID: 31082062]
Sharma M, Rai P, Rameshbabu CS, Senadhipan B. Imaging of peritoneal ligaments by endoscopic ultrasound (with videos). Endoscopic ultrasound. 2015 Jan-Mar:4(1):15-27. doi: 10.4103/2303-9027.151317. Epub [PubMed PMID: 25789280]
Cosentino F, Rossitto C, Turco LC, Gueli Alletti S, Vascone C, Di Meglio L, Scambia G, Malzoni M. Laparoscopic Management of Abdominal Pregnancy. Journal of minimally invasive gynecology. 2017 Jul-Aug:24(5):724-725. doi: 10.1016/j.jmig.2017.01.023. Epub 2017 Feb 4 [PubMed PMID: 28179200]
Omole AE, Mandiga P, Kahai P, Lobo S. Anatomy, Abdomen and Pelvis: Large Intestine. StatPearls. 2025 Jan:(): [PubMed PMID: 29261962]
Lowe MC, D'Angelica MI. Anatomy of Hepatic Resectional Surgery. The Surgical clinics of North America. 2016 Apr:96(2):183-95. doi: 10.1016/j.suc.2015.11.003. Epub 2016 Feb 16 [PubMed PMID: 27017858]
Mirilas P, Skandalakis JE. Benign anatomical mistakes: right and left coronary ligaments. The American surgeon. 2002 Sep:68(9):832-5 [PubMed PMID: 12356161]
Le O. Patterns of peritoneal spread of tumor in the abdomen and pelvis. World journal of radiology. 2013 Mar 28:5(3):106-12. doi: 10.4329/wjr.v5.i3.106. Epub [PubMed PMID: 23671747]
Kogure K, Kojima I, Kuwano H, Matsuzaki T, Yorifuji H, Takata K, Makuuchi M. Reconfirmation of the anatomy of the left triangular ligament and the appendix fibrosa hepatis in human livers, and its implication in abdominal surgery. Journal of hepato-biliary-pancreatic sciences. 2014 Dec:21(12):856-63. doi: 10.1002/jhbp.144. Epub 2014 Aug 20 [PubMed PMID: 25139445]
Agarwal S, Munyal R, Aravinthan A, Clarke C. Left triangular ligament lesions are likely hepatic in origin: a systematic review. The British journal of radiology. 2023 Nov:96(1152):20230231. doi: 10.1259/bjr.20230231. Epub 2023 Oct 3 [PubMed PMID: 37747273]
Level 1 (high-level) evidenceKostov S, Selçuk I, Watrowski R, Dineva S, Kornovski Y, Slavchev S, Ivanova Y, Dzhenkov D, Yordanov A. Surgical Anatomy of the Liver-Significance in Ovarian Cancer Surgery. Diagnostics (Basel, Switzerland). 2023 Jul 14:13(14):. doi: 10.3390/diagnostics13142371. Epub 2023 Jul 14 [PubMed PMID: 37510115]
O'Connor A, Sabri S, Solkar M, Ramzan A, Solkar M. Falciform ligament torsion as a rare aetiology of the acute abdomen. Journal of surgical case reports. 2022 Jan:2022(1):rjab150. doi: 10.1093/jscr/rjab150. Epub 2022 Jan 17 [PubMed PMID: 35047164]
Level 3 (low-level) evidenceChinese Society of Colorectal Surgeons, Chinese Society of Colorectal Surgery, National Health Commission Capacity Building and Continuing Education Center Colorectal Surgery Committee, Chinese Society of Colorectal and Anal Functional Surgery. [Chinese expert consensus on definition and terminology of colon and rectum: mesentery, fascia, and space (2023 edition)]. Zhonghua wei chang wai ke za zhi = Chinese journal of gastrointestinal surgery. 2023 Jun 25:26(6):529-535. doi: 10.3760/cma.j.cn441530-20230604-00192. Epub [PubMed PMID: 37583006]
Level 3 (low-level) evidenceBhatia A, Shatanof RA, Bordoni B. Embryology, Gastrointestinal. StatPearls. 2025 Jan:(): [PubMed PMID: 30725857]
McLin VA, Henning SJ, Jamrich M. The role of the visceral mesoderm in the development of the gastrointestinal tract. Gastroenterology. 2009 Jun:136(7):2074-91. doi: 10.1053/j.gastro.2009.03.001. Epub 2009 Mar 17 [PubMed PMID: 19303014]
Indrio F, Neu J, Pettoello-Mantovani M, Marchese F, Martini S, Salatto A, Aceti A. Development of the Gastrointestinal Tract in Newborns as a Challenge for an Appropriate Nutrition: A Narrative Review. Nutrients. 2022 Mar 28:14(7):. doi: 10.3390/nu14071405. Epub 2022 Mar 28 [PubMed PMID: 35406018]
Level 3 (low-level) evidenceMontgomery RK, Mulberg AE, Grand RJ. Development of the human gastrointestinal tract: twenty years of progress. Gastroenterology. 1999 Mar:116(3):702-31 [PubMed PMID: 10029630]
Roberts DJ. Molecular mechanisms of development of the gastrointestinal tract. Developmental dynamics : an official publication of the American Association of Anatomists. 2000 Oct:219(2):109-20 [PubMed PMID: 11002332]
Rubarth LB, Van Woudenberg CD. Development of the Gastrointestinal System: An Embryonic and Fetal Review. Neonatal network : NN. 2016:35(3):156-8. doi: 10.1891/0730-0832.35.3.156. Epub [PubMed PMID: 27194610]
Heil JR, Bordoni B. Embryology, Umbilical Cord. StatPearls. 2025 Jan:(): [PubMed PMID: 32491422]
Basta M, Lipsett BJ. Anatomy, Abdomen and Pelvis: Umbilical Cord. StatPearls. 2025 Jan:(): [PubMed PMID: 32491321]
Spurway J, Logan P, Pak S. The development, structure and blood flow within the umbilical cord with particular reference to the venous system. Australasian journal of ultrasound in medicine. 2012 Aug:15(3):97-102. doi: 10.1002/j.2205-0140.2012.tb00013.x. Epub 2015 Dec 31 [PubMed PMID: 28191152]
Pinette MG, Tropepe M. Umbilical Cord Abnormalities. Clinical obstetrics and gynecology. 2025 Mar 1:68(1):111-118. doi: 10.1097/GRF.0000000000000915. Epub 2024 Dec 19 [PubMed PMID: 39696752]
Dubetskyi BI, Makarchuk OM, Zhurakivska OY, Rymarchuk MI, Andriets OA, Lenchuk TL, Delva KM, Piron-Dumitrascu M, Bakun OV. Pregnancy and umbilical cord pathology: structural and functional parameters of the umbilical cord. Journal of medicine and life. 2023 Aug:16(8):1282-1291. doi: 10.25122/jml-2023-0025. Epub [PubMed PMID: 38024812]
Feldberg MA, van Leeuwen MS. The properitoneal fat pad associated with the falciform ligament. Imaging of extent and clinical relevance. Surgical and radiologic anatomy : SRA. 1990:12(3):193-202 [PubMed PMID: 2149617]
Gray S, Ganti L. Significance of the Hepatic Falciform Artery. Cureus. 2021 Jul:13(7):e16440. doi: 10.7759/cureus.16440. Epub 2021 Jul 17 [PubMed PMID: 34466300]
Buffoli B, Verzeletti V, Gabusi V, Giugno L, Hirtler L, Faini G. Anatomical basis of retrograde thoracic veins flow and its implications in complex thoracic wall reconstructive surgery. Surgical and radiologic anatomy : SRA. 2022 Oct:44(10):1319-1328. doi: 10.1007/s00276-022-03015-5. Epub 2022 Sep 21 [PubMed PMID: 36129523]
White HJ, Soos MP. Anatomy, Thorax, Superior Vena Cava. StatPearls. 2025 Jan:(): [PubMed PMID: 31424839]
Martin BF, Tudor RG. The umbilical and paraumbilical veins of man. Journal of anatomy. 1980 Mar:130(Pt 2):305-22 [PubMed PMID: 7400038]
Foster RJ, Cowell GW. Acute paraumbilical vein recanalization: an unusual complication of acute pancreatitis. BJR case reports. 2015:1(1):20150021. doi: 10.1259/bjrcr.20150021. Epub 2015 Apr 20 [PubMed PMID: 30363191]
Level 3 (low-level) evidenceTucker WD, Shrestha R, Burns B. Anatomy, Abdomen and Pelvis: Inferior Vena Cava. StatPearls. 2025 Jan:(): [PubMed PMID: 29493975]
Baba Y, Hokotate H, Nakajo M. Visualization of the internal mammary artery via the hepatic falciform artery in a patient with hepatocellular carcinoma. Acta radiologica (Stockholm, Sweden : 1987). 2004 Nov:45(7):716-7 [PubMed PMID: 15624512]
Kumar PM, Kotaiah MT, Keerthi G, Reddy V. Falciform Ligament Abscess Causing Acute Abdomen: Unveiling the Enigma with Review of Literature. Journal of Indian Association of Pediatric Surgeons. 2025 Jan-Feb:30(1):41-45. doi: 10.4103/jiaps.jiaps_135_24. Epub 2025 Jan 2 [PubMed PMID: 39968264]
Luo Q, Liu P, Dong Y, Qin T. The role of the hepatic autonomic nervous system. Clinical and molecular hepatology. 2023 Oct:29(4):1052-1055. doi: 10.3350/cmh.2023.0244. Epub 2023 Jul 25 [PubMed PMID: 37489022]
Level 2 (mid-level) evidenceHan SY. Variation in falciform ligament with pheumoperitoneum. Journal of the Canadian Association of Radiologists. 1980 Sep:31(3):171-3 [PubMed PMID: 7419542]
Cho KC, Baker SR. Visualization of the extrahepatic segment of the ligamentum teres: a sign of free air on plain radiographs. Radiology. 1997 Mar:202(3):651-4 [PubMed PMID: 9051011]
Altafulla JJ, Iwanaga J, Kikuta S, Prickett J, Ishak B, Uz A, Dumont AS, Tubbs RS. The falciform ligament: Anatomical study with microsurgical implications. Clinical neurology and neurosurgery. 2020 Aug:195():106049. doi: 10.1016/j.clineuro.2020.106049. Epub 2020 Jun 29 [PubMed PMID: 32652394]
Rahimli M, Perrakis A, Schellerer V, Andric M, Stockheim J, Lorenz E, Franz M, Arend J, Croner RS. A falciform ligament flap surface sealing technique for laparoscopic and robotic-assisted liver surgery. Scientific reports. 2020 Jul 22:10(1):12143. doi: 10.1038/s41598-020-69211-8. Epub 2020 Jul 22 [PubMed PMID: 32699283]
Reggiani P, Antonelli B, Rossi G. Robotic surgery of the liver: Italian experience and review of the literature. Ecancermedicalscience. 2013 Sep 26:7():358. doi: 10.3332/ecancer.2013.358. Epub 2013 Sep 26 [PubMed PMID: 24174991]
Goto H, Hashimoto M, Akamatsu D, Shimizu T, Miyama N, Tsuchida K, Tajima Y, Ohuchi N. Surgical resection and inferior vena cava reconstruction for treatment of the malignant tumor: technical success and outcomes. Annals of vascular diseases. 2014:7(2):120-6. doi: 10.3400/avd.oa.13-00125. Epub 2014 Mar 15 [PubMed PMID: 24995055]
Kaneko J, Hayashi Y, Kazami Y, Nishioka Y, Miyata A, Ichida A, Kawaguchi Y, Akamatsu N, Hasegawa K. Resection and reconstruction of the largest abdominal vein system (the inferior vena cava, hepatic, and portal vein): a narrative review. Translational gastroenterology and hepatology. 2024:9():23. doi: 10.21037/tgh-23-90. Epub 2024 Mar 21 [PubMed PMID: 38716218]
Level 3 (low-level) evidenceElgazar A, Awad AK, Elseidy SA. Falciform ligament use in perforated duodenal ulcer repair: a case report and literature review. Journal of surgical case reports. 2020 Nov:2020(11):rjaa243. doi: 10.1093/jscr/rjaa243. Epub 2020 Nov 12 [PubMed PMID: 33214862]
Level 3 (low-level) evidenceReddy GPS, Mecheri Antony A, Venkateswaran R. Laparoscopic Repair of Duodenal Perforation Using the Falciform Ligament: A Cross-Sectional Study. Cureus. 2024 Nov:16(11):e73576. doi: 10.7759/cureus.73576. Epub 2024 Nov 13 [PubMed PMID: 39677075]
Level 2 (mid-level) evidencePaudel P, Agrawal S, Khatiwada B, Rai P, Karki S. Pedicled falciform ligament flap use as an alternative surgical technique in peptic ulcer perforation repair: a case report and review of literature. Journal of surgical case reports. 2024 Aug:2024(8):rjae502. doi: 10.1093/jscr/rjae502. Epub 2024 Aug 15 [PubMed PMID: 39149529]
Level 3 (low-level) evidenceKashyap SS, Abbas KA, Herron R, Abbas FA, Chudnovets A, Abbas G. Use of a mobilized, perfused, falciform ligament patch for repair of paraconduit herniation after robotic-assisted Ivor Lewis esophagectomy. JTCVS techniques. 2024 Jun:25():204-207. doi: 10.1016/j.xjtc.2024.02.023. Epub 2024 Mar 11 [PubMed PMID: 38899100]
Park AE, Hoogerboord CM, Sutton E. Use of the falciform ligament flap for closure of the esophageal hiatus in giant paraesophageal hernia. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2012 Jul:16(7):1417-21. doi: 10.1007/s11605-012-1888-4. Epub 2012 May 1 [PubMed PMID: 22547347]
Koussayer B, Nehila T, Awshah S, Sujka JA, DuCoin CG. A Case Report of a Rare Hernia: Incarcerated Falciform Ligament Hernia. Cureus. 2023 Apr:15(4):e37386. doi: 10.7759/cureus.37386. Epub 2023 Apr 10 [PubMed PMID: 37182046]
Level 3 (low-level) evidenceRunkel M, Kuvendjiska J, Marjanovic G, Fichtner-Feigl S, Diener MK. Ligamentum teres augmentation (LTA) for hiatal hernia repair after minimally invasive esophageal resection: a new use for an old structure. Langenbeck's archives of surgery. 2021 Nov:406(7):2521-2525. doi: 10.1007/s00423-021-02284-9. Epub 2021 Oct 6 [PubMed PMID: 34611750]
Abe N, Sugiyama M, Suzuki Y, Yanagida O, Masaki T, Mori T, Atomi Y. Falciform ligament in pancreatoduodenectomy for protection of skeletonized and divided vessels. Journal of hepato-biliary-pancreatic surgery. 2009:16(2):184-8. doi: 10.1007/s00534-008-0036-8. Epub 2009 Jan 24 [PubMed PMID: 19169616]
Andreasi V, Partelli S, Crippa S, Balzano G, Tamburrino D, Muffatti F, Belfiori G, Cirocchi R, Falconi M. A systematic review and meta-analysis on the role of omental or falciform ligament wrapping during pancreaticoduodenectomy. HPB : the official journal of the International Hepato Pancreato Biliary Association. 2020 Sep:22(9):1227-1239. doi: 10.1016/j.hpb.2020.05.003. Epub 2020 Jul 4 [PubMed PMID: 32631806]
Level 1 (high-level) evidenceOliver TI, Sharma B, John S. Portal Hypertension. StatPearls. 2025 Jan:(): [PubMed PMID: 29939540]
Al-Busafi SA, McNabb-Baltar J, Farag A, Hilzenrat N. Clinical manifestations of portal hypertension. International journal of hepatology. 2012:2012():203794 [PubMed PMID: 23024865]
Dajti E, Ravaioli F, Zykus R, Rautou PE, Elkrief L, Grgurevic I, Stefanescu H, Hirooka M, Fraquelli M, Rosselli M, Chang PEJ, Piscaglia F, Reiberger T, Llop E, Mueller S, Marasco G, Berzigotti A, Colli A, Festi D, Colecchia A, Spleen Stiffness—IPD-MA Study Group. Accuracy of spleen stiffness measurement for the diagnosis of clinically significant portal hypertension in patients with compensated advanced chronic liver disease: a systematic review and individual patient data meta-analysis. The lancet. Gastroenterology & hepatology. 2023 Sep:8(9):816-828. doi: 10.1016/S2468-1253(23)00150-4. Epub 2023 Jul 18 [PubMed PMID: 37478880]
Level 1 (high-level) evidenceHill M, Bechet JJ, d'Albis A. Disuccinimidyl esters as bifunctional crosslinking reagents for proteins: assays with myosin. FEBS letters. 1979 Jun 15:102(2):282-6 [PubMed PMID: 456607]
Level 3 (low-level) evidenceFolpe AL, Goodman ZD, Ishak KG, Paulino AF, Taboada EM, Meehan SA, Weiss SW. Clear cell myomelanocytic tumor of the falciform ligament/ligamentum teres: a novel member of the perivascular epithelioid clear cell family of tumors with a predilection for children and young adults. The American journal of surgical pathology. 2000 Sep:24(9):1239-46 [PubMed PMID: 10976698]
Egle J, Gupta A, Mittal V, Orfanou P, Silapaswan S. Internal hernias through the falciform ligament: a case series and comprehensive literature review of an increasingly common pathology. Hernia : the journal of hernias and abdominal wall surgery. 2013 Feb:17(1):95-100. doi: 10.1007/s10029-012-0990-6. Epub 2012 Oct 6 [PubMed PMID: 23053747]
Level 2 (mid-level) evidenceBrock JS, Pachter HL, Schreiber J, Hofstetter SR. Surgical diseases of the falciform ligament. The American journal of gastroenterology. 1992 Jun:87(6):757-8 [PubMed PMID: 1590315]
Ozkececı ZT, Ozsoy M, Celep B, Bal A, Polat C. A rare cause of acute abdomen: an isolated falciform ligament necrosis. Case reports in emergency medicine. 2014:2014():570751. doi: 10.1155/2014/570751. Epub 2014 Jun 17 [PubMed PMID: 25045547]
Level 3 (low-level) evidenceHamal D, Fernandes A, Sagma J, Rufino M, Hamal P, DiBenedetto G. Falciform Ligament Infarction: A Case Report and Review of the Literature. Cureus. 2023 Nov:15(11):e48361. doi: 10.7759/cureus.48361. Epub 2023 Nov 6 [PubMed PMID: 37937182]
Level 3 (low-level) evidencePriola AM, Priola SM, Cataldi A, Marci V, Fava C. Acute abdomen as an unusual presentation of hepatic PEComa. A case report. Tumori. 2009 Jan-Feb:95(1):123-8 [PubMed PMID: 19366072]
Level 3 (low-level) evidenceSørensen J, Møller AM, Håkansson T. [Acute abdomen caused by necrosis of the falciform ligament of the liver]. Ugeskrift for laeger. 1983 Feb 21:145(8):583 [PubMed PMID: 6857822]
Level 3 (low-level) evidenceHonda H, Watanabe K, Mihara K, Hoshi H, Sakihama M. Lipoma of the hepatic falciform ligament. Journal of computer assisted tomography. 1983 Feb:7(1):170 [PubMed PMID: 6826846]
Level 3 (low-level) evidenceMoon SB, Lee HW, Park KW, Jung SE. Falciform ligament abscess after omphalitis: report of a case. Journal of Korean medical science. 2010 Jul:25(7):1090-2. doi: 10.3346/jkms.2010.25.7.1090. Epub 2010 Jun 16 [PubMed PMID: 20592906]
Level 3 (low-level) evidenceKakitsubata Y, Nakamura R, Shiba T, Sugimura H, Suzuki Y, Kakitsubata S, Watanabe K, Kawana T, Iwamura T. Lipoma of the falciform ligament: US, CT, and MRI appearances. Clinical imaging. 1993 Jan-Mar:17(1):27-9 [PubMed PMID: 8439840]
Level 3 (low-level) evidenceSari S, Ersöz F, Güneş ME, Paşaoğlu E, Arikan S. Hematoma of the falciform ligament: a rare cause of acute abdomen. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology. 2011:22(2):213-5 [PubMed PMID: 21796563]
Level 3 (low-level) evidenceSourtzis S, Canizares C, Thibeau JF, Philippart P, Damry N. An unusual case of herniation of small bowel through an iatrogenic defect of the falciform ligament. European radiology. 2002 Mar:12(3):531-3 [PubMed PMID: 11870465]
Level 3 (low-level) evidence