Introduction
Electrical injuries are a unique type of trauma that is distinct from mechanical trauma, such as blunt or penetrating injuries. These injuries result from the transfer of either low-voltage or high-voltage electricity to an individual's body and are often associated with significant morbidity and mortality. Most electrical injuries are accidental and typically preventable. When not immediately fatal, electrical injuries can cause dysfunction in multiple tissues or organs.[1][2][3][4]
Electrical injuries are categorized into 4 main types based on how electricity affects the body of an individual: flash, flame, lightning, and true injuries. Flash injuries, caused by an arc flash, typically result in cutaneous burns, as no electrical current passes through the body. Flame injuries occur when an arc flash ignites an individual's clothing, leading to thermal burns. Lightning injuries involve extremely short-duration, high-voltage electrical energy and are characterized by flash-over currents along the skin surface. Conduction through the body may vary. True electrical injuries occur when the individual becomes part of an electrical circuit, usually with identifiable contact points at the entrance and exit sites.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Electrical injuries are generally classified into 2 categories—low-voltage (<1000 volts) and high-voltage (≥1000 volts). In North America, household appliances typically operate at 110 to 120 volts (represented by the unit "V"), whereas a power of 220 to 240 volts is standard in many other parts of the world. Low-voltage injuries can occur at home through contact with small appliances, extension cords, or wall outlets, which may result in significant trauma or complications, particularly with prolonged exposure.
In children, low-voltage injuries often result from biting or chewing electrical cords and may occur without loss of consciousness or cardiac arrest. Despite the lower voltage, such injuries can still cause severe damage—similar to high-voltage injuries—depending on factors such as the duration of contact (eg, prolonged muscle tetany), the individual's size, and the cross-sectional area in contact with the electrical source.[5][6][7][8] Large overhead transmission power lines typically carry voltages ranging from 69 to 765 kilovolts (represented by the unit "kV"), whereas smaller distribution lines carry voltages ranging from 4 to 34.5 kV. In occupational settings, at least half of all electrocutions (fatalities resulting from electrical injuries) are caused by contact with power lines, and approximately one-quarter are due to electrical machinery or tools. Lightning strikes typically carry a voltage between 100 and 150 million volts (represented by the unit "MV").
Epidemiology
In the United States, electrical injuries cause approximately 1000 deaths annually. Of these, around 400 result from high-voltage electrical injuries, while lightning accounts for 50 to 300 deaths. Additionally, there are at least 30,000 nonfatal electrical shock incidents each year. Electrical injuries also account for about 5% of all burn unit admissions annually in the United States. Approximately 20% of all electrical injuries occur in children, with the highest incidence seen in toddlers and adolescents. In adults, these injuries most commonly occur in occupational settings and represent the fourth-leading cause of work-related traumatic death. In contrast, electrical injuries in children typically happen at home.[9]
Pathophysiology
Electricity is generated by the flow of electrons through a conductive material along a potential gradient, moving from areas of high to low electron concentration. Ohm’s law defines the relationship between current, voltage, and resistance, which states that current is directly proportional to voltage and inversely proportional to resistance.[10] The potential gradient, or the difference in electron concentrations between high and low areas, determines the voltage and varies depending on the electrical source. Electrical injuries are classified as low-voltage (<1000 V) or high-voltage (≥1000 V). In the United States, household electricity typically operates at 110 to 120 V, although some high-power appliances may use up to 240 V. In comparison, industrial and high-tension power lines can carry voltages exceeding 100,000 V.
Current (I) refers to the flow of electric charge (the volume of electrons) moving down a potential gradient and is measured in amperes (represented by the unit "A"). This represents the amount of electrical energy passing through an individual’s body during an electrical injury. The maximum current an individual can tolerate while still being able to release the electrical source, before muscle tetany sets in, varies from person to person.
Resistance (R) measures how much a material opposes the flow of electrical current and is expressed in ohms (Ω). In the body, resistance varies among tissues based on their water and electrolyte content levels. Tissues with high concentrations of water and electrolytes, such as blood vessels, neurons, and muscles, have low resistance and are excellent conductors of electricity. In contrast, bone, fat, and skin have high resistance and are poor conductors of electricity. Skin resistance increases with greater thickness, dryness, and keratinization. Moist mucous membranes or breaches in the skin (such as punctures, lacerations, or abrasions) exhibit lower resistance.
High skin resistance leads to greater energy dissipation at the skin surface, often resulting in cutaneous burns and reducing the amount of electrical energy that reaches internal tissues. In contrast, low skin resistance may cause minimal or no visible skin injury, while allowing more electrical energy to transfer to internal tissues. Therefore, the extent of external burns on the skin does not reliably indicate the severity of internal damage, and the absence of external burns does not rule out significant internal electrical injury. The resistance of internal tissues further determines the extent of injury sustained. An additional factor to consider is current density, which is determined by the cross-sectional area of a particular tissue. For example, as electrical energy travels down an arm, which is mainly composed of low-resistance tissues such as muscle, nerve, and blood vessels, the current density is relatively low and constant throughout. This holds true until the electrical energy reaches the joints (such as the elbow, wrist, and fingers), where a larger proportion of the cross-sectional area consists of high-resistance tissues such as bone and tendons, and fewer low-resistance tissues. As a result, the electrical energy becomes concentrated in the remaining low-resistance tissues, making them more susceptible to injury at the joints throughout the body.
Other key determinants of electrical injury throughout the body include the source (the entry point) and ground (the exit point) of the current. The hand is the most common source, followed by the head, whereas the feet are usually the most common ground. However, it is often difficult to clinically distinguish entry from exit points; therefore, the term "contact points" is preferred, much like how gunshot wounds are described as penetrating injuries rather than entry and exit sites. Electrical injuries may also cause skip lesions, resulting in multiple contact points. Any current passing through the head can lead to damage to the central nervous system (CNS). When the current travels across the chest—such as from hand to leg or hand to hand—the heart is often affected, increasing the risk of potentially fatal arrhythmias. The degree of electrical injury experienced by an individual can be predicted using the Kouwenhoven factors, which include the type of current, current strength, duration of exposure, body resistance, the pathway the current takes through the body, and the electrical field strength.
The type of current refers to either alternating current (AC) or direct current (DC). AC is commonly used in household electrical outlets (generally 50-60 Hz, low frequency), and it changes direction rhythmically. In contrast, DC is found in most batteries and flows continuously in one direction. Most cardioverters and defibrillators also use DC. The higher the current and voltage—whether AC or DC—the greater the extent of electrical damage. High-voltage currents (≥1000 V) typically cause deep tissue injury, whereas low-voltage currents (<1000 V) are more likely to induce muscle tetany. Muscle tetany typically occurs in response to electrical stimulation at frequencies between 40 and 110 Hz, which is the frequency range of most household currents. When this contraction affects the hand, the flexor muscles may cause the individual to grasp the electrical source, prolonging contact.[10][11]
The perception threshold of electrical current through touch, typically experienced as a tingling sensation, occurs at approximately one milliampere (mA). The let-go current is the maximum current (amperage) an individual can tolerate while still being able to release the electrical source voluntarily, despite muscle contraction. This threshold varies depending on factors such as muscle mass and body weight. For example, an average 70 kg adult male has a let-go current of about 75 mA for DC and 15 mA for AC. Most children have a lower let-go threshold, typically ranging from 3 to 5 mA.
Electrical circuit breakers and fuses are designed to interrupt electrical flow when excessive current is detected, typically at thresholds between 15 and 20 A. in residential settings, the let-go current for both adults and children is several orders of magnitude lower than the current needed to trip a standard household breaker, as these breakers are designed to protect household wiring rather than individuals. In contrast, ground fault circuit interrupters (GFCIs) are specialized switches and breakers designed for areas such as kitchens and bathrooms to protect individuals from electrical injury by detecting current imbalances as low as 4 to 6 mA and tripping the circuit accordingly.
The frequency of AC primarily determines its effect on the body. Low-frequency AC tends to cause tetany, or prolonged muscle contraction, which can make it difficult for an individual to release the electrical source, thereby increasing the duration of exposure. For this reason, low-frequency AC is often more hazardous than high-frequency AC. Generally, AC is approximately 3 to 5 times more damaging than direct current DC at the same voltage and current. Additionally, DC typically causes a single muscle contraction or convulsion, often propelling the person away from the source of the electrical current.
Finally, current density must be considered when determining the level of tissue injury. The severity of the injury is determined by the surface area through which the current passes—the larger the contact area, the lower the current density. For example, a very high voltage spread over a large surface area may have a current density equal to or even less than that of a much lower voltage concentrated on a smaller surface area. Therefore, low-voltage injuries that focus on a small area can often cause as much damage as high-voltage injuries that are distributed over a larger area. An illustrative example is the use of monopolar electrocautery in the operating room, where the same amount of current passes from the tip of the pen to the grounding pad. As the tip has a smaller surface area, it produces a higher current density at the point of contact, resulting in localized tissue destruction.
Low electrical field strength is associated with an immediate, uncomfortable sensation (referred to as a “shock”) that will not result in any significant injury. In contrast, high electrical field strength can cause electrochemical or thermal damage to tissues, leading to protein coagulation, coagulation necrosis, hemolysis, thrombosis, tendon or muscle avulsion, and dehydration. Beyond the direct electrical injury, high electrical field strength can result in massive tissue edema, which may be caused by thrombosis, vascular congestion, and muscle swelling, potentially leading to compartment syndrome. This tissue edema can also cause dehydration, hypovolemia, and hypotension. Severe muscle injury may further lead to rhabdomyolysis, myoglobinuria, and electrolyte disturbances. Altogether, these sequelae place affected individuals at a very high risk of acute kidney injury.[12]
History and Physical
Electrical injuries are classified into 4 categories—flash, flame, lightning, and true, each with distinct presentations and different signs and symptoms. However, before evaluating an individual for an electrical injury, life-threatening conditions should be assessed first using an algorithmic approach.
True Electrical Injury
An individual who has experienced a "true" electrical injury may present with a wide range of complaints or issues, including cardiac arrhythmia or arrest, respiratory arrest, coma, blunt trauma, or various types of burns. Some patients may complain of occasional unpleasant sensations without visible physical damage, whereas others may exhibit significant pain and overt tissue damage. Regardless of the patient’s presentation, it is crucial to gather detailed information about the electrical source (eg, high versus low voltage, AC versus DC), duration of contact, and any associated trauma that may have occurred.
Patients who have experienced a low-voltage AC injury may present with only superficial burns or, conversely, with severe injuries if contact is prolonged or muscle tetany occurs. Low-voltage AC injuries can potentially lead to cardiac or respiratory arrest, arrhythmias (such as ventricular fibrillation), or unwitnessed seizures. Therefore, electrical injury should be considered as a differential diagnosis in any patient presenting with, or recently having experienced, cardiac or respiratory arrest. Additionally, gathering detailed information about the electrical injury from witnesses or emergency medical personnel is also crucial to guide appropriate treatment.
High-voltage AC injuries are more likely to cause severe thermal burns, and individuals often experience loss of consciousness or cardiac arrest. In these cases, providers should make every effort to gather detailed information about the injury from witnesses or medical personnel. Although the exact voltage is often unknown, identifying the setting of the injury—such as residential, commercial, or power line exposure—can help estimate the voltage involved.
Regardless of presenting complaints or the apparent severity of the electrical injury, all patients should undergo a comprehensive physical examination to evaluate the full extent of tissue damage. High-voltage injuries are associated with greater morbidity, including higher rates of compartment syndrome, rhabdomyolysis, renal failure, and limb amputation.[13][14] Mortality rates for high-voltage injuries range from 5% to 30%, whereas low-voltage injuries have a significantly lower mortality rate of less than 1% to 3%.[6][13]
Ventricular fibrillation, for example, can occur with exposure to currents as low as 50 to 120 mA—levels lower than the highest accessible current in most households. Beyond arrhythmias and other electrical disturbances, electrical injuries can also directly damage cardiac myocytes. As a result, patients may develop delayed arrhythmias such as sinus tachycardia or premature ventricular contractions. However, long-term cardiac complications from electrical injuries are rare. If the electrical current pathway crosses the thorax, there is a risk of paralysis of the chest wall muscles, which can lead to respiratory arrest. Unlike cardiac muscle, lung tissue is a poor conductor of electricity and therefore rarely sustains direct electrical injury.
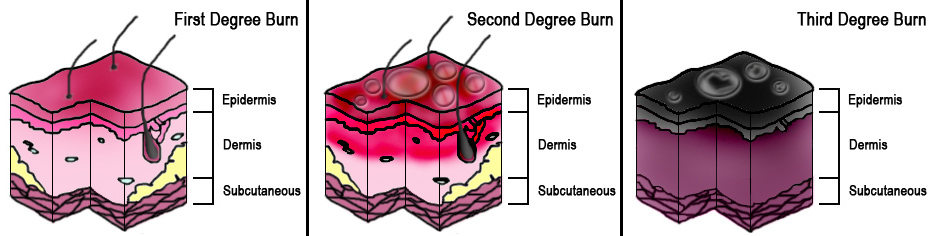
Skin damage from a true electrical injury can often be severe, yet cutaneous burns may appear minor despite significant internal damage. Burns are typically most severe at contact points, with the extent of injury depending mainly on the intensity and duration of contact with the electrical source. Smaller contact points often indicate higher current density and greater electrical field strength compared to larger ones. However, the actual risk of requiring surgical intervention (eg, amputation or fasciotomy) depends on the full clinical history and other presenting signs and symptoms (see Image. Degrees of Burn).
When electrical injuries affect the extremities, a high suspicion of compartment syndrome is essential. Extensive muscle necrosis from electroporation leads to significant edema, resulting in swelling that raises compartment pressures within the confines of the muscular fascia. This condition is similar to—but distinct from—eschar syndrome, which results from circumferential full-thickness burns; in eschar syndrome, the constricting eschar, rather than the fascia, must be released to relieve pressure. In both syndromes, clinicians should assess "he “" Ps”: pain out of proportion to the examination, paresthesias, paralysis, pallor, poikilothermia, and pulselessness.
Posterior shoulder dislocations are rare injuries that can result from electrical injuries or seizures. Unlike the more common anterior dislocations, posterior dislocations occur when the stronger internal rotator muscles overpower the external rotators, forcing the humeral head out of the glenoid fossa. Individuals at highest risk include those who experience high-voltage or tetanic low-voltage injuries. Affected individuals typically present with the arm adducted and internally rotated.[15]
Flash Electrical Injury
A flash burn occurs when the intense heat generated by an electrical discharge, such as an electrical arc, causes injury. These arcs can reach temperatures of approximately 19,000 °C. As current travels between 2 electrodes, it ionizes surrounding gases and creates plasma—the fourth state of matter. This phenomenon occurs when current passes through a typically nonconductive medium, forming localized areas of high current density, often accompanied by visible light.
Large electric arcs in nature occur in the form of lightning, which is a distinct category of electrical injury. In contrast, electrical arcs are used in processes such as welding and plasma cutting in industrial settings. Undesired arcs may occur due to improperly installed circuit breakers, switches, or electrical contact points. Flash burns resemble thermal burns more than true electrical injuries, as the electrical current typically does not pass through the body of an individual. These burns cause cutaneous injuries without the usual contact points, and the lesions vary in depth, ranging from hyperemic tissue in superficial burns to dry, leathery skin in full-thickness burns.
Pediatric patients may present with oral burns after biting or sucking on an electrical wire or appliance. An electric arc often forms between the external and internal aspects of the mouth, potentially involving the orbicularis oris muscle or causing lip deformity if the burn crosses the oral commissure (corners of the mouth). Significant edema and eschar formation typically develop within 2 to 3 days. If the eschar involves the labial artery, severe bleeding may occur when the eschar sloughs off, usually after 2 to 3 weeks. These patients should be closely monitored and receive appropriate follow-up with burn specialists and oral or plastic surgeons. Parents should be instructed to control bleeding by applying local pressure—pinching the lips—while transporting the child to specialized care.
Flame Electrical Injury
Flame burns occur from exposure to radiating heat without direct physical contact. In electrical flame burns, the electrical current ignites clothing or nearby materials, resulting in cutaneous burns. When clothing catches fire, contact burns may also develop. Additionally, synthetic fabrics (such as polyester or nylon) can melt and adhere to the skin, causing deeper burns.
Lightning Electrical Injury
Affected individuals are typically outdoors and become the path of least resistance for electricity traveling from the clouds to the ground. The clinical presentation can range from minimal cutaneous burns to severe injuries resembling those seen in high-voltage commercial electrical exposures. Although not always present, the appearance of a fern-like pattern on the skin, known as "Lichtenberg figures," is highly suggestive of a lightning strike. Additional findings may include ruptured tympanic membranes, ophthalmic injuries, and neurological complications such as seizures, paralysis, and paresthesias. A unique manifestation, known as keraunoparalysis (also referred to as Charcot paralysis), involves transient tetraplegia and loss of proprioception, which can last from hours to several weeks.[16]
Evaluation
Affected individuals of electrical injuries should be addressed as both trauma and cardiac patients. All adult patients who have experienced an electrical injury should undergo an electrocardiogram (ECG) and cardiac monitoring. Prolonged monitoring is warranted for patients presenting with chest pain, ECG abnormalities, a known transthoracic pathway of electrical injury, cardiac arrest, loss of consciousness, or preexisting cardiac history. Most patients without significant injury or cardiac abnormalities on initial assessment are unlikely to develop any cardiac abnormalities after 24 to 48 hours.[17][18][19][20]
In general, patients with a normal ECG who have sustained a low-voltage electrical injury, without any cardiac symptoms or a history of cardiac issues, may be safely discharged from the hospital after a thorough physical examination. Similarly, children exposed to low-voltage, household current electrical exposure without any significant injury or preexisting cardiac history may be discharged following a comprehensive physical examination.
Laboratory studies to be considered for any patient who has experienced an electrical injury include a complete blood count (CBC), a comprehensive metabolic panel with evaluation of electrolytes and creatinine levels, and a urinalysis. If myoglobinuria is detected on urinalysis, serum myoglobin should be assessed. An arterial blood gas analysis may be warranted in patients with rhabdomyolysis or those requiring respiratory support. Creatine kinase (CK) levels should be evaluated, particularly if rhabdomyolysis is suspected. If the electrical current is suspected to have passed through the chest, or if the patient reports chest pain or has ECG abnormalities (eg, arrhythmia or ischemia), cardiac biomarkers such as CK-MB and troponin should also be measured.
Imaging studies may be considered based on the type of injury and associated symptoms. A chest radiograph is indicated for patients presenting with cardiac or respiratory arrest, chest pain, shortness of breath, hypoxia, a history of fall or blunt trauma, or those who require cardiopulmonary resuscitation (CPR). A head computed tomography (CT) scan is warranted for patients with altered mental status, known head trauma, loss of consciousness, seizures, or focal neurological deficits. In addition to a head CT scan, cervical spine immobilization is recommended for these patients, and cervical spine imaging may also be considered. However, it may not be necessary in patients without focal neurological deficits, changes in mental status, or significant injury.
Notably, the severity of an electrical injury does not correlate with the extent of external burns on an individual's body; the absence of visible burns does not rule out internal tissue damage. Therefore, some patients may require additional imaging, such as CT or ultrasound, depending on the suspected path of the electrical current through the body. The choice of imaging modality should be guided by the specific tissues being evaluated.
Finally, high-voltage exposure or prolonged contact with low-voltage current may cause significant tissue damage that warrants surgical intervention, such as fasciotomy. In such cases, early surgical consultation is essential, as prompt fasciotomy may help prevent serious complications, including limb amputation.
Treatment / Management
Upon arrival in the emergency department, patients with electrical injuries should be promptly stabilized and provided with respiratory and circulatory support as needed, following Advanced Cardiovascular Life Support (ACLS) and Advanced Trauma Life Support (ATLS) protocols. Cardiac monitoring should be initiated in all patients who have sustained more than a minor low-voltage electrical burn.
Any patient presenting with facial or oral burns, hypoxia, respiratory distress, loss of consciousness, or any condition that compromises airway protection or patency should receive supplemental oxygen and appropriate airway management, such as ventilation, intubation, or cricothyrotomy.
Depending on the type of trauma or injury sustained, the patient may require cervical spine or full spinal immobilization. A primary assessment to evaluate for traumatic injuries (eg, pneumothorax or fractures) should be performed promptly. Following this, any patient with significant burns or suspected rhabdomyolysis (evidenced by myoglobinuria) should receive fluid resuscitation, with a target urine output of 1 to 2 mL/kg/h. The use of an osmotic diuretic (eg, mannitol), a loop diuretic (eg, furosemide), or urine alkalinization (via sodium bicarbonate titration) may be considered. However, such interventions are generally discouraged in patients with cutaneous burns involving more than 20% of the total body surface area or those with concomitant trauma, as these individuals may be hypovolemic and at risk for hemodynamic instability.
Intravenous (IV) access should be established in all adult patients who have experienced an electrical injury. If IV access proves difficult, intraosseous (IO) access should be considered. In cases of significant trauma, cardiac or respiratory arrest, or loss of consciousness, central IV access may be necessary. Whenever possible, IVs, IOs, and central lines should not be placed through burned tissue, as this increases the risk of infection. However, if no alternative access sites are available, these lines may be used temporarily, as prompt resuscitation takes priority.
Proper burn care should be initiated, including administering a tetanus vaccination if needed, along with appropriate splinting and bandaging after a thorough neurovascular assessment.
Any patient who has experienced cardiac or respiratory arrest, loss of consciousness, chest pain, hypoxia, arrhythmia, significant trauma or burns, or shows abnormalities on ECG should be admitted for further inpatient care. This may also be followed by transfer to a burn care unit or a rehabilitation center as necessary. Finally, early consultations with trauma or critical care specialists, surgical teams, and orthopedic specialists should be initiated to help prevent complications and minimize the risk of irreversible damage.
Before discharge, patients should receive education on potential sources of electrical exposure at home and in the workplace, along with information about the possible long-term effects of electrical injuries, including neurological, psychological, or physical complications. Appropriate follow-up appointments should also be scheduled based on the severity and nature of the injury.
Emerging Therapies
Recent research has investigated the potential of Poloxamer-188 (P-188) as a treatment for electrical injuries. This surfactant, composed of both hydrophilic and hydrophobic segments, has demonstrated the ability to repair damaged cell membranes and reduce muscle and nerve injury associated with electrical trauma. Studies suggest that P-188 stabilizes injured cell membranes, reduces inflammation, and prevents further tissue degradation. While it has been primarily investigated in conditions such as sickle cell disease and ischemia-reperfusion injury, its potential use in treating electrical burns and deep tissue damage is also being explored. Ongoing clinical trials are assessing its safety and efficacy in humans, which may support its inclusion in future treatment guidelines.[21][22]
In addition, advancements in regenerative medicine have led to the exploration of stem cell therapy as a potential treatment for electrical injuries, focusing on reducing tissue damage, enhancing wound healing, and promoting nerve regeneration. Mesenchymal stem cells, derived from sources such as bone marrow, adipose tissue, and umbilical cord blood, have demonstrated the ability to mitigate inflammation, reduce fibrosis, and stimulate tissue repair.
Given the extensive muscle, nerve, and vascular damage caused by high-voltage injuries, this novel therapy offers a promising approach by enhancing cell survival and promoting functional recovery. Preclinical studies suggest that mesenchymal stem cells can improve outcomes in burn-related injuries by reducing oxidative stress and promoting angiogenesis, a process essential for wound healing. Ongoing research aims to clarify the role of this therapy in preventing delayed neuropathy, a common and significant complication of electrical injuries. Although still in experimental stages, stem cell–based treatments have the potential to revolutionize electrical burn management by providing a regenerative solution to reduce long-term disability.[23][24]
Hyperbaric oxygen therapy may be considered for patients with severe electrical injuries, especially those with extensive burns. By delivering pure oxygen in a pressurized environment, this therapy enhances tissue oxygenation, reduces inflammation, and stimulates angiogenesis, thereby supporting the body’s natural healing processes and helping to prevent infection. In addition, this therapy is particularly beneficial for patients with severe tissue damage and limited oxygen supply, as it promotes tissue regeneration and improves the viability of skin grafts.[25]
Differential Diagnosis
The differential diagnoses of electrical burns include, but are not limited to, the following conditions:
- Chemical burns
- Thermal burns
- Intracranial haemorrhage
- Ocular burns and chemical injuries
- Respiratory arrest
- Rhabdomyolysis
- Seizures
- Syncope
- Status epilepticus
- Ventricular fibrillation
Prognosis
The outcome and prognosis of electrical injuries depend on the location and extent of the injury, the development of complications, and the patient's functional recovery. High-voltage electrical injuries are associated with poorer outcomes compared to low-voltage injuries. However, recent advancements in intensive care units (ICUs), resuscitation, nutritional support, surgical techniques, and the use of novel skin substitutes have significantly improved overall outcomes.
Complications
High electrical field strength often causes electrochemical or thermal damage to affected tissues, increasing the risk of protein coagulation, coagulation necrosis, hemolysis, thrombosis, muscle or tendon avulsion, and dehydration. Beyond the direct electrical injury, it can also lead to massive tissue edema, resulting from thrombosis, vascular congestion, and muscle swelling, which may progress to compartment syndrome. This tissue edema can cause dehydration, accompanied by hypovolemia and hypotension. Severe muscle injury may trigger rhabdomyolysis, myoglobinuria, and electrolyte imbalances. Collectively, these complications place patients at a very high risk for acute kidney injury.
Potential Long-Term Sequelae of Electrical Injuries: [26]
- Neurological complications that may persist after an electrical injury include:
- Neuropathy
- Seizures
- Syncope
- Tinnitus
- Paresthesias
- Weakness
- Loss of balance, poor coordination, or gait ataxia
- Psychological complications that may persist after an electrical injury include:
- Memory or attention difficulties
- Irritability
- Depression
- Posttraumatic stress
- Ocular complications that may persist after an electrical injury include:
- Cataracts
- Physical complications that may persist after an electrical injury include:
- Pain
- Fatigue
- Contractures
- Muscle spasms
- Pruritus
- Headaches
- Fever or night sweats
- Reduced range of motion or stiffness in the joints
Consultations
Managing electrical injuries requires a multidisciplinary team of healthcare professionals. The following specialists are typically involved in patient care:
- General or Burn surgeon
- Orthopedic surgeon
- Critical Care or Trauma specialist
- Neurosurgeon
- Neurologist
- Cardiologist
- Psychiatrist
- Physiotherapist
Deterrence and Patient Education
Proper precautions should always be undertaken when working with electricity. To prevent electrical burns at home, the following safety measures should be considered:
- Use child-safety covers on all electrical outlets.
- Keep electrical cords out of children's reach.
- Follow all manufacturer instructions when using electrical appliances.
- Replace devices with damaged electrical cords.
- Avoid using electrical appliances in the shower or bath.
- Always turn off the circuit breaker and verify the absence of live wires using a noncontact electricity tester before working on any electrical system.
Before discharge, patients should be educated about potential sources of electrical exposure at home and work, the associated risks, and any possible long-term effects of their electrical injuries (eg, neurological, psychological, or physical). Appropriate follow-up appointments should be scheduled as needed.
Enhancing Healthcare Team Outcomes
Diagnosing and managing electrical injuries is most effective with an interprofessional team, including emergency department providers, radiologists, surgeons, trauma specialists, anesthesiologists, and burn specialists. Depending on the injury’s severity, following the advanced trauma life support protocol may be necessary. Cardiac monitoring should be initiated for all patients who have sustained a low-voltage burn, regardless of its severity.
Implementing structured treatment algorithms within healthcare institutions has been shown to improve the management of electrical injuries. A study demonstrated that such protocols can reduce unnecessary testing and hospital admissions while effectively identifying patients at risk for complications.[27]
Any patient presenting with facial or oral burns, hypoxia, respiratory distress, loss of consciousness, or difficulty protecting or maintaining a patent airway should receive oxygen and airway protection measures (eg, ventilation, intubation, or cricothyrotomy). All patients who experience respiratory or cardiac arrest require ICU admission. Early consultation with trauma or critical care specialists, surgical specialists, and orthopedists is recommended to prevent complications or irreversible damage.[28]
Before discharge, patients should be educated about potential sources of electrical exposure at home and work, the associated risks, and any possible long-term effects of their electrical injuries (eg, neurological, psychological, or physical). Appropriate follow-up should be scheduled as needed.
Media
(Click Image to Enlarge)
References
Burnham T, Hilgenhurst G, McCormick ZL. Second-degree Skin Burn from a Radiofrequency Grounding Pad: A Case Report and Review of Risk-Mitigation Strategies. PM & R : the journal of injury, function, and rehabilitation. 2019 Oct:11(10):1139-1142. doi: 10.1002/pmrj.12143. Epub 2019 Apr 29 [PubMed PMID: 30746904]
Level 3 (low-level) evidenceKim MS, Lee SG, Kim JY, Kang MY. Maculopathy from an accidental exposure to welding arc. BMJ case reports. 2019 Feb 3:12(2):. doi: 10.1136/bcr-2018-227677. Epub 2019 Feb 3 [PubMed PMID: 30718265]
Level 3 (low-level) evidenceCarrano FM, Iezzi L, Melis M, Quaresima S, Gaspari AL, Di Lorenzo N. A Surgical Instrument Cover for the Prevention of Thermal Injuries During Laparoscopic Operations. Journal of laparoendoscopic & advanced surgical techniques. Part A. 2019 Jan 30:():. doi: 10.1089/lap.2018.0742. Epub 2019 Jan 30 [PubMed PMID: 30698493]
Lovaglio AC, Socolovsky M, Di Masi G, Bonilla G. Treatment of neuropathic pain after peripheral nerve and brachial plexus traumatic injury. Neurology India. 2019 Jan-Feb:67(Supplement):S32-S37. doi: 10.4103/0028-3886.250699. Epub [PubMed PMID: 30688230]
Trivedi TK, Liu C, Antonio ALM, Wheaton N, Kreger V, Yap A, Schriger D, Elmore JG. Injuries Associated With Standing Electric Scooter Use. JAMA network open. 2019 Jan 4:2(1):e187381. doi: 10.1001/jamanetworkopen.2018.7381. Epub 2019 Jan 4 [PubMed PMID: 30681711]
Daskal Y, Beicker A, Dudkiewicz M, Kessel B. [HIGH VOLTAGE ELECTRIC INJURY: MECHANISM OF INJURY, CLINICAL FEATURES AND INITIAL EVALUATION.]. Harefuah. 2019 Jan:158(1):65-69 [PubMed PMID: 30663297]
Bailey ME, Sagiraju HKR, Mashreky SR, Alamgir H. Epidemiology and outcomes of burn injuries at a tertiary burn care center in Bangladesh. Burns : journal of the International Society for Burn Injuries. 2019 Jun:45(4):957-963. doi: 10.1016/j.burns.2018.12.011. Epub 2019 Jan 3 [PubMed PMID: 30612889]
Von Caues S, Herbst CI, Wadee SA. A retrospective review of fatal electrocution cases at Tygerberg Forensic Pathology Services, Cape Town, South Africa, over the 5-year period 1 January 2008 - 31 December 2012. South African medical journal = Suid-Afrikaanse tydskrif vir geneeskunde. 2018 Nov 26:108(12):1042-1045. doi: 10.7196/SAMJ.2018.v108i12.13131. Epub 2018 Nov 26 [PubMed PMID: 30606289]
Level 2 (mid-level) evidenceKarray R, Chakroun-Walha O, Mechri F, Salem I, Drira H, Nasri A, Damak A, Rekik N. Outcomes of electrical injuries in the emergency department: epidemiology, severity predictors, and chronic sequelae. European journal of trauma and emergency surgery : official publication of the European Trauma Society. 2025 Jan 27:51(1):85. doi: 10.1007/s00068-025-02766-1. Epub 2025 Jan 27 [PubMed PMID: 39869174]
Culnan DM, Farner K, Bitz GH, Capek KD, Tu Y, Jimenez C, Lineaweaver WC. Volume Resuscitation in Patients With High-Voltage Electrical Injuries. Annals of plastic surgery. 2018 Mar:80(3 Suppl 2):S113-S118. doi: 10.1097/SAP.0000000000001374. Epub [PubMed PMID: 29461290]
Esses SI, Peters WJ. Electrical burns; pathophysiology and complications. Canadian journal of surgery. Journal canadien de chirurgie. 1981 Jan:24(1):11-4 [PubMed PMID: 7459729]
Rouse RG, Dimick AR. The treatment of electrical injury compared to burn injury: a review of pathophysiology and comparison of patient management protocols. The Journal of trauma. 1978 Jan:18(1):43-7 [PubMed PMID: 340708]
Shih JG, Shahrokhi S, Jeschke MG. Review of Adult Electrical Burn Injury Outcomes Worldwide: An Analysis of Low-Voltage vs High-Voltage Electrical Injury. Journal of burn care & research : official publication of the American Burn Association. 2017 Jan/Feb:38(1):e293-e298. doi: 10.1097/BCR.0000000000000373. Epub [PubMed PMID: 27359191]
Schweizer R, Pedrazzi N, Klein HJ, Gentzsch T, Kim BS, Giovanoli P, Plock JA. Risk Factors for Mortality and Prolonged Hospitalization in Electric Burn Injuries. Journal of burn care & research : official publication of the American Burn Association. 2021 May 7:42(3):505-512. doi: 10.1093/jbcr/iraa192. Epub [PubMed PMID: 33137191]
Ketenci IE, Duymus TM, Ulusoy A, Yanik HS, Mutlu S, Durakbasa MO. Bilateral posterior shoulder dislocation after electrical shock: A case report. Annals of medicine and surgery (2012). 2015 Dec:4(4):417-21. doi: 10.1016/j.amsu.2015.10.010. Epub 2015 Nov 4 [PubMed PMID: 26904192]
Level 3 (low-level) evidenceJacob NE, M R. Keraunoparalysis: Fleeting Paralysis Following a Lightning Flash. Cureus. 2024 Oct:16(10):e70773. doi: 10.7759/cureus.70773. Epub 2024 Oct 3 [PubMed PMID: 39493204]
Pawlik AM, Lampart A, Stephan FP, Bingisser R, Ummenhofer W, Nickel CH. Outcomes of electrical injuries in the emergency department: a 10-year retrospective study. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2016 Dec:23(6):448-454 [PubMed PMID: 25969345]
Level 2 (mid-level) evidenceDavis C, Engeln A, Johnson EL, McIntosh SE, Zafren K, Islas AA, McStay C, Smith WR, Cushing T, Wilderness Medical Society. Wilderness Medical Society practice guidelines for the prevention and treatment of lightning injuries: 2014 update. Wilderness & environmental medicine. 2014 Dec:25(4 Suppl):S86-95. doi: 10.1016/j.wem.2014.08.011. Epub [PubMed PMID: 25498265]
Level 1 (high-level) evidenceGentges J, Schieche C. Electrical injuries in the emergency department: an evidence-based review. Emergency medicine practice. 2018 Nov:20(11):1-20 [PubMed PMID: 30358379]
Lee DH, Desai MJ, Gauger EM. Electrical Injuries of the Hand and Upper Extremity. The Journal of the American Academy of Orthopaedic Surgeons. 2019 Jan 1:27(1):e1-e8. doi: 10.5435/JAAOS-D-17-00833. Epub [PubMed PMID: 30278017]
Wong SW, Yao Y, Hong Y, Ma Z, Kok SH, Sun S, Cho M, Lee KK, Mak AF. Preventive Effects of Poloxamer 188 on Muscle Cell Damage Mechanics Under Oxidative Stress. Annals of biomedical engineering. 2017 Apr:45(4):1083-1092. doi: 10.1007/s10439-016-1733-0. Epub 2016 Sep 20 [PubMed PMID: 27650939]
Moloughney JG, Weisleder N. Poloxamer 188 (p188) as a membrane resealing reagent in biomedical applications. Recent patents on biotechnology. 2012 Dec:6(3):200-11 [PubMed PMID: 23092436]
Surowiecka A, Chrapusta A, Klimeczek-Chrapusta M, Korzeniowski T, Drukała J, Strużyna J. Mesenchymal Stem Cells in Burn Wound Management. International journal of molecular sciences. 2022 Dec 5:23(23):. doi: 10.3390/ijms232315339. Epub 2022 Dec 5 [PubMed PMID: 36499664]
Wang M, Xu X, Lei X, Tan J, Xie H. Mesenchymal stem cell-based therapy for burn wound healing. Burns & trauma. 2021:9():tkab002. doi: 10.1093/burnst/tkab002. Epub 2021 May 1 [PubMed PMID: 34212055]
Murias R, Court Y, Merbilhaá O, Fariña G, Pace EL, Biglia A, Igoillo MC, Echezuri J, Garone A, Crocenzi A, Portas M. Therapeutic approach to electric burn with platelet rich plasma, grafts and hyperbaric oxygenation. Medicina. 2021:81(2):297-300 [PubMed PMID: 33906152]
Wesner ML, Hickie J. Long-term sequelae of electrical injury. Canadian family physician Medecin de famille canadien. 2013 Sep:59(9):935-9 [PubMed PMID: 24029506]
Nisar S, Keyloun JW, Kolachana S, McLawhorn MM, Moffatt LT, Travis TE, Shupp JW, Johnson LS. Institutional Experience Using a Treatment Algorithm for Electrical Injury. Journal of burn care & research : official publication of the American Burn Association. 2021 May 7:42(3):351-356. doi: 10.1093/jbcr/irab020. Epub [PubMed PMID: 33530107]
Gille J, Schmidt T, Dragu A, Emich D, Hilbert-Carius P, Kremer T, Raff T, Reichelt B, Siafliakis A, Siemers F, Steen M, Struck MF. Electrical injury - a dual center analysis of patient characteristics, therapeutic specifics and outcome predictors. Scandinavian journal of trauma, resuscitation and emergency medicine. 2018 May 31:26(1):43. doi: 10.1186/s13049-018-0513-2. Epub 2018 May 31 [PubMed PMID: 29855384]