Introduction
Anatomy
The elbow is a complex hinge-and-pivot joint formed by 3 articulations: the humeroulnar joint between the trochlea of the humerus and the ulnar notch, permitting flexion and extension; the humeroradial (radiocapitellar) joint between the capitellum of the humerus and the radial head, which allows both rotation and flexion-extension movements; and the proximal radioulnar joint between the proximal ulna and radius, enabling forearm pronation and supination. These 3 articulations are enclosed within a single synovial sheath (see Image. Medial and Volar Views of the Right Elbow).
Stability of the elbow is maintained despite its broad range of motion (ROM), which spans from 0° in full extension to 150° in full flexion, and approximately 80° in both supination and pronation. The radial head and the annular ligament contribute significantly to proximal forearm stability (see Image. Ligamentous Anatomy of the Right Elbow).
The coronoid process plays a critical role in elbow joint stability by preventing posterior translation of the ulna relative to the humerus. As an attachment site for the lateral ulnar collateral ligament and the anterior band of the medial collateral ligament, the coronoid contributes to resistance against varus and valgus stress.[1][2][3] Axial load is primarily transmitted through the radiocapitellar joint, particularly in extension. The olecranon limits anterior translation of the humerus.
The medial epicondyle serves as the common origin for the superficial forearm flexor-pronator group, including the flexor carpi radialis, flexor carpi ulnaris, palmaris longus, pronator teres, and flexor digitorum superficialis. The lateral epicondyle provides attachment for several extensor muscles and the supinator, including extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris.
The elbow consists of 3 bones: the distal humerus, which includes the condyles and the articular surfaces (trochlea and capitellum); the proximal ulna, composed of the olecranon and coronoid process; and the proximal radius, defined primarily by the radial head. Several common elbow fracture types involve these anatomic components, discussed below.
Supracondylar Fracture
Fractures of the distal humerus just above the elbow, known as supracondylar fractures, account for approximately 60% of all elbow fractures in children.[4] These injuries primarily affect the immature skeleton and occur most commonly in younger age groups. Based on the mechanism and direction of distal fragment displacement, supracondylar fractures are classified as either extension- or flexion-type.[5][6][7]
Extension-type fractures account for more than 95% of cases and result from a fall onto an outstretched hand (FOOSH) with the elbow in full extension. The transmitted force is directed toward the olecranon fossa, a structurally vulnerable site. Posterior displacement of the distal fragment is typical. Nondisplaced fractures may be radiographically subtle, with indirect signs such as a posterior fat pad, anterior sail sign, or disruption of the anterior humeral line.
The radiographic classification of extension-type fractures is as follows:
- Type I: Nondisplaced or minimally displaced
- Type II: Displaced, with intact posterior cortex
- Type III: Completely displaced, with disruption of both cortices
Flexion-type fractures occur in less than 5% of cases and result from direct anterior trauma to a flexed elbow, leading to anterior displacement of the distal fragment. These injuries frequently involve posterior periosteal disruption and are often open due to the direct force.[8][9][10][11]
Flexion-type fractures are classified as follows:
- Type I: Nondisplaced or minimally displaced
- Type II: Incomplete fracture with intact anterior cortex
- Type III: Completely displaced with proximal and anterior migration of the distal fragment
Neurovascular injury is a major complication, particularly involving the brachial artery and median nerve due to their proximity to the fracture site (see Image. Course of the Median Nerve in the Forearm). Prompt recognition and management are essential to prevent long-term morbidity.
Gartland classification
Supracondylar fractures are classified according to the degree of displacement, with extension-type fractures comprising the vast majority of cases. The Gartland classification categorizes extension-type fractures as follows:
- Type I: Nondisplaced or minimally displaced fracture. Radiographic visualization may be difficult, as the fracture is often occult. The anterior humeral line continues to intersect the anterior half of the capitellum. A positive fat pad sign may be the only radiologic clue (see Image. Posterior Fat Pad Sign in Supracondylar Fracture).
- Type II: Posteriorly displaced fracture with an intact posterior cortex.
- Type III: Completely displaced fracture with disruption of both cortices. Posteromedial displacement occurs in approximately 75% of cases, while posterolateral displacement is seen in 25%.
- Type IV: Involves complete circumferential periosteal disruption and results in multidirectional instability, with loss of stability in both flexion and extension. Although not part of the original Gartland classification, this type has important management implications, as closed reduction may be challenging and often requires surgical fixation with careful intraoperative assessment of stability.[12]
In flexion-type supracondylar fractures, the distal fragment is displaced anteriorly due to direct trauma to a flexed elbow. These fractures are less common than extension-type injuries and are often associated with high-energy trauma.
Lateral Condyle Fracture
Lateral condyle fractures are the 2nd most common type of elbow fracture in children, accounting for 15% to 20% of all cases. These injuries involve the lateral condyle of the distal humerus, the outer bony prominence of the elbow. The peak incidence occurs between the ages of 4 and 10 years. Most lateral condyle fractures are classified as Salter-Harris type IV, involving the metaphysis, physis, and epiphysis.
Two classification systems are commonly used to describe these fractures. The Milch classification describes lateral condyle fractures based on the location of the fracture line relative to the trochlear groove. In Milch type I, the fracture line lies lateral to the trochlear groove. In Milch type II, the fracture extends through the groove. Although Milch type II is more commonly observed, this classification alone does not reliably predict elbow instability.[13] Current management decisions are based more on the degree of displacement and the extent of articular and soft tissue involvement rather than the fracture line’s position within the trochlea.
The displacement classification categorizes fractures based on the degree of displacement. Type 1 fractures exhibit less than 2 mm of displacement. Type 2 fractures show displacement between 2 mm and 4 mm, with the fragment remaining near the humerus. Type 3 fractures are widely displaced with disruption of the articular surface.[14]
Medial Epicondyle Fracture
Medial epicondyle fractures are the 3rd most common type of elbow fracture in children. These extra-articular injuries involve the apophysis of the medial epicondyle, located on the posteromedial aspect of the elbow. The typical age of occurrence is between 9 and 14 years, with a higher incidence in boys. These fractures frequently result from athletic activities such as football, baseball, or gymnastics. Common mechanisms include posterior elbow dislocation or repetitive valgus stress, as seen in repeated overhead throwing. This overuse mechanism is often referred to as "Little League elbow." Clinical presentation includes medial elbow pain, tenderness over the medial epicondyle, and valgus instability.
Radial Head and Neck Fracture
Radial head fractures are more common in adults and account for approximately 1/3 of all elbow fractures. In children, these fractures most often follow a Salter-Harris type II pattern, with the fracture line traversing the physis and extending into the metaphysis. Hemarthrosis is a frequent finding following this kind of injury due to the radial head’s rich vascular supply.
The Mason classification system describes radial head fractures based on displacement and associated injuries. Type I fractures are nondisplaced and involve less than or equal to 2 mm of displacement. Type II fractures are displaced by more than 2 mm. Type III fractures are comminuted. Type IV fractures are associated with elbow dislocation.
Olecranon Fracture
Olecranon fractures account for approximately 10% of elbow fractures (see Image. Occult Olecranon Fracture on Lateral Elbow Radiograph). The olecranon is the most proximal portion of the ulna, extending from its tip to the coronoid process. The olecranon curves around the distal humerus and articulates with the trochlea to form the posterior aspect of the elbow joint. All olecranon fractures are intra-articular and involve the point of insertion of the triceps tendon. These fractures are relatively uncommon in children and are frequently associated with concomitant injuries, particularly radial head or neck fractures. A transolecranon fracture-dislocation represents a complex injury involving both fracture and elbow joint dislocation.[15]
The fracture pattern depends on the mechanism of injury. Comminuted fractures typically result from a direct fall onto the elbow, whereas noncomminuted fractures often occur following a FOOSH. The degree of elbow flexion at the time of trauma influences both the location and morphology of the fracture.
Coronoid Fracture
The coronoid process, the anterior-most bony prominence of the proximal ulna, serves a critical stabilizing function by resisting posterior translation of the ulna. Fractures of the coronoid process occur in approximately 10% to 15% of elbow dislocations.
The Regan and Morrey classification describes coronoid fractures according to the extent of involvement. Type I fractures involve only the tip of the coronoid. These injuries often appear stable, but instability may occur in the setting of ligamentous disruption or terrible triad injuries. Type II fractures involve up to half of the coronoid process and may compromise ulnohumeral stability. Type III fractures affect more than half of the coronoid and are frequently associated with posterior elbow instability.
Monteggia Fracture
A Monteggia fracture involves a fracture of the proximal ulna with dislocation of the radial head at the elbow.[16] Although the radius appears intact on initial imaging, this injury demands a high index of suspicion for radial head dislocation in any patient with a proximal ulnar fracture. The most common mechanism is a FOOSH, resulting in hyperpronation. Alternative mechanisms include a direct posterior blow to the ulna or a fall on a flexed elbow.
Monteggia fractures are frequently missed, making them one of the most commonly overlooked serious elbow injuries. Delayed or missed diagnosis is not uncommon, often leading to poor functional outcomes. Careful assessment of the radiocapitellar alignment is essential in any case of ulnar fracture to avoid overlooking a radial head dislocation.
Capitellum Fracture
Capitellum fractures are uncommon, accounting for fewer than 1% of adult elbow fractures. These injuries usually result from high-energy trauma, such as a direct blow or fall. Capitellar fractures are often difficult to detect on plain radiographs and may require advanced imaging, such as computed tomography (CT), for definitive diagnosis.
Terrible Triad Injury
The terrible triad injury consists of a posterolateral elbow dislocation combined with fractures of the radial head and the anterolateral facet of the coronoid process (see Image. Terrible Triad Injury on Lateral Elbow Radiography).[17] This injury complex also includes disruption of the lateral ulnar collateral ligament and is associated with significant instability and an unpredictable clinical outcome.[18]
Fracture Classification by Joint Involvement
Elbow fractures may be classified based on joint involvement. Extra-articular fractures include supracondylar, epicondylar, condyle, and intercondylar fractures that do not involve the articular surface. Intra-articular fractures involve components of the joint surface, such as the trochlea, capitellum, radial head, and proximal ulna.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Fracture patterns vary with patient age and mechanism of injury. The most common cause is a FOOSH, although direct trauma to the elbow can also result in a fracture. Playground injuries, particularly those involving monkey bars, are frequent sources of pediatric elbow trauma.
Supracondylar fractures may present as either extension- or flexion-type injuries, depending on the direction of distal fragment displacement. Extension-type fractures typically result from a FOOSH injury, while flexion-type fractures commonly arise from a direct blow to the posterior olecranon. Radial head fractures commonly occur following a FOOSH injury with the forearm in pronation.[19]
Coronoid process fractures are often caused by axial compression transmitted through the trochlea. Transolecranon fracture-dislocation is a high-energy injury caused by direct trauma to the proximal dorsal forearm. This mechanism results in anterior displacement of the forearm relative to the distal humerus, typically with a comminuted olecranon fracture.[20]
Olecranon fracture types arise from different mechanisms. Comminuted fractures typically follow a direct fall onto the elbow, whereas noncomminuted fractures are associated with FOOSH injuries.
Epidemiology
Elbow fractures account for up to 5% of all fractures, with a higher incidence in children than in adults.[21] Supracondylar fractures are the most common type in children younger than 7 years, peaking between ages 5 and 7, and occur more frequently in boys. Fracture patterns vary by age and mechanism of injury. In children, the most common types are supracondylar fractures (50% to 70%), followed by lateral condylar (17% to 34%) and medial epicondylar fractures (10%).[22] In contrast, intra-articular fractures predominate in adults.
Pathophysiology
The elbow is a complex joint with 3-dimensional mobility, permitting flexion and extension between the distal humerus and the ulna. Stability is provided by the osseous architecture, joint capsules, and surrounding ligaments. The ulnohumeral joint provides the primary restraint to static elbow stability, particularly in flexion, while the radiocapitellar joint bears the majority of axial load during extension, with load distribution varying depending on elbow position.[23][24] Common clinical findings include limited elbow extension and pain during forearm supination and pronation.
History and Physical
Elbow fractures commonly result from direct trauma or a FOOSH. Acute presentation includes sharp, localized pain in the elbow and forearm, with limited extension and discomfort during supination and pronation. Swelling and tenderness frequently obscure surface anatomy. Palpation of the radial neck, olecranon, medial and lateral epicondyles, and supracondylar region is essential to localize injury.
A systematic approach to physical examination should include inspection, palpation, assessment of ROM, and a focused neurovascular evaluation. Gross deformity may indicate significant displacement. In Monteggia fractures, the dislocated radial head may be subtle or easily missed, making the assessment of radiocapitellar alignment critical. Evaluation of the full 4-directional ROM—pronation, supination, flexion, and extension—should be performed. Preserved ROM lowers clinical suspicion for major fractures but does not exclude intra-articular injuries such as radial head or capitellum fractures.[25]
In adults, the elbow extension test may aid in ruling out a fracture. Full active extension significantly lowers, but does not eliminate, the likelihood of significant bony injury. Tenderness and swelling over the antecubital fossa may suggest a coronoid process fracture.
A comprehensive neurovascular examination is mandatory. Numbness in the forearm or hand suggests possible nerve involvement. Peripheral pulses must be palpated to assess vascular integrity.
The anterior interosseous nerve (AIN) is most frequently affected in supracondylar fractures. Assessment involves testing the flexor pollicis longus and flexor digitorum profundus by instructing the patient to form an “OK” sign. Inability to perform this maneuver indicates motor dysfunction of the AIN. Posterior interosseous nerve (PIN) integrity is evaluated through active finger extension. A warm, well-perfused hand does not rule out brachial artery injury, as distal perfusion may be maintained by collateral circulation despite complete arterial disruption. Serial neurovascular examinations should be performed to monitor for evolving compartment syndrome or delayed vascular compromise, particularly following reduction or splinting.
Regional assessment should extend beyond the elbow. Examination of the ipsilateral shoulder and wrist is necessary to exclude concurrent injuries. Coronoid fractures may coexist with complex injury patterns such as the terrible triad, which includes elbow dislocation, radial head fracture, and coronoid process involvement. Thorough clinical evaluation is essential to identify subtle or unstable fracture patterns.
In pediatric patients, growth plate injuries may be radiographically subtle, and nonverbal signs such as guarding or irritability should be carefully interpreted. Evaluation must account for open physes, cartilaginous structures, and age-specific fracture patterns.
Evaluation
Evaluation should begin with a primary survey, which includes a rapid assessment of vital signs, airway patency, adequate breathing, circulation, and control of external bleeding. This initial step aims to identify and address life-threatening conditions without delay. A focused neurovascular examination must follow, as injuries to nerves or blood vessels are common in elbow trauma.
Serial neurovascular examinations are critical throughout the course of treatment, particularly after reduction or immobilization, to detect evolving ischemia or compartment syndrome. The AIN is most frequently injured and may be evaluated by asking the patient to make an “OK” sign by flexing the thumb and index finger simultaneously to form a circle. The inability to perform this movement may indicate nerve damage. The PIN, a deep branch of the radial nerve, may be injured in Monteggia fractures. This nerve supplies the finger extensors and the supinator, and injury manifests as weakness or paralysis of thumb and finger extension. Vascular injury may involve the brachial artery, and a subset of cases may be complicated by compartment syndrome.
Initial imaging should include anteroposterior and lateral radiographs of the elbow. The anteroposterior view visualizes the medial and lateral epicondyles and their articular surfaces. The lateral view assesses the alignment of the distal humerus and proximal forearm, including the relationships of the anterior and posterior fat pads to the humerus. A systematic radiographic approach should include verification of radiocapitellar alignment on all views, as disruption may be the only indicator of a Monteggia fracture or subtle dislocation.
On lateral imaging, the anterior humeral line should intersect the middle 3rd of the capitellum, while the radiocapitellar line, drawn through the center of the radial neck, should also pass through the center of the capitellum. Disruption of these anatomic relationships suggests fracture. Although the anterior fat pad may be visible normally, elevation or displacement may indicate joint effusion or hemarthrosis. A visible posterior fat pad is always considered pathologic, particularly in the setting of a suspected supracondylar fracture.
An oblique radiographic view provides improved visualization of the radiocapitellar joint, medial epicondyle, radioulnar joint, and coronoid process. This view is especially useful for identifying subtle lateral condyle fractures and evaluating displacement. An anteroposterior view obtained with the elbow flexed to 40° may help disengage the olecranon from the olecranon fossa, improving visualization of the capitellum. The radial head should be aligned with the capitellum in all views to confirm normal radiocapitellar alignment.
A contralateral comparison radiograph may be considered in young children but is not routinely recommended. Interpreting pediatric elbow radiographs can be challenging due to the predominantly cartilaginous composition of the joint and the presence of open growth plates. Evaluation should account for the possibility of cartilaginous injuries not visible on plain radiographs. Nonverbal cues such as irritability or refusal to use the arm may be early signs of injury.
Six ossification centers surround the pediatric elbow. Familiarity with the sequence denoted by "CRITOE" is essential for identifying subtle elbow injuries in children.
- C: Capitellum
- R: Radial head
- I: Internal (medial) epicondyle
- T: Trochlea
- O: Olecranon
- E: External (lateral) epicondyle
The capitellum typically appears at approximately 1 year of age, with each successive ossification center emerging at roughly 2-year intervals, around 1, 3, 5, 7, 9, and 11 years, respectively.
CT may be necessary to determine the precise location of a fracture and assess for associated instability. Three-dimensional reconstructions enhance the evaluation of complex fracture patterns in select cases. Capitellum fractures are often difficult to detect on plain radiographs, necessitating CT for accurate visualization. Coronoid fracture fragments may appear small or poorly defined on lateral radiographs. Therefore, CT is recommended when such fractures are suspected. CT should also be considered for intra-articular fractures with questionable displacement or in cases of mechanical instability where radiographs are inconclusive. Magnetic resonance imaging can help identify occult fractures, chondral injuries, and soft tissue damage in pediatric or athletic populations.
Ultrasound has become an increasingly useful diagnostic tool for elbow fractures. Cortical disruption of bone, visible on sonography, serves as a direct indicator of fracture. A recent systematic review has demonstrated high sensitivity and specificity for ultrasound in both ruling out and confirming elbow fractures.[26] Arteriography is indicated when brachial artery injury is suspected but should not delay timely closed reduction of the fracture.
Treatment / Management
The goals of treatment are to immobilize the fracture and restore proper alignment in an acceptable anatomic position. Early identification and treatment of neurovascular injuries are essential to reduce the risk of complications. Management is guided by fracture stability and the degree of neurovascular compromise. Immediate application of forearm traction is warranted when neurovascular involvement is present, as this maneuver may restore distal pulses. Adequate analgesia must be administered without delay.
Initial management should include prompt immobilization using a posterior long-arm splint, elevation of the limb, and frequent neurovascular assessments to monitor for evolving ischemia or compartment syndrome. Serial examinations are particularly important after reduction or splint application.
Interventions for Supracondylar Fractures
Nondisplaced supracondylar fractures do not require operative intervention. Initial treatment consists of immobilization using a long-arm posterior splint. The elbow must be flexed at 90° while the forearm is positioned neutrally. The splint is later replaced by a cast once the swelling has subsided. A follow-up radiograph after 1 week is necessary to confirm appropriate alignment and monitor healing. Cast removal typically occurs after 3 to 4 weeks.
Displaced supracondylar fractures require surgical intervention. Angulation exceeding 20° warrants orthopedic evaluation and fracture reduction under sedation and analgesia. Neurovascular status must be continuously monitored.
Closed reduction with percutaneous pinning is a standard technique in managing displaced fractures. Bone fragments are realigned through closed reduction and stabilized with 2 lateral metal pins. Three pins may be required in the presence of severe displacement or a floating distal segment. The fixation is reinforced with a splint or cast, and both the pins and immobilization device are removed once adequate healing is observed in the ensuing weeks.
Open reduction with internal fixation (ORIF) is indicated in unstable supracondylar fractures. A 2-pin lateral-entry configuration is frequently employed as the primary method of percutaneous stabilization.[27] Indications for open reduction include failure of closed reduction, vascular insufficiency suggesting possible entrapment of the brachial artery, and the presence of an open fracture. Hospital admission may be necessary to monitor neurovascular function, particularly in cases of displaced fractures or extensive soft tissue swelling.(B2)
Ongoing follow-up should assess for complications such as malunion, nerve injury, and restricted ROM. Delayed or missed diagnoses may increase the risk of permanent dysfunction.
Lateral Condyle Fracture Management
Management of lateral condyle fractures is similar to that of supracondylar fractures but typically requires a longer duration of immobilization, often up to 6 weeks. Close radiographic monitoring is essential due to the high risk of secondary displacement during healing. Monitoring should include repeat imaging within the first 7 to 10 days, as even initially nondisplaced fractures may undergo progressive displacement over time.
Medial Epicondyle Fracture Treatment
Treatment follows principles similar to those for supracondylar fractures but involves a slightly different fixation approach. Instead of percutaneous pinning, small screws are used to secure the bone fragments. Consequently, the recovery period is shorter, and immobilization with a splint or cast is generally required for only 1 to 2 weeks (see Image. Rose and Welch Splints).
Interventions for Radial Head and Neck Fractures
The extent of fracture displacement determines the treatment strategy. When radial head displacement is less than 30°, immobilization with a collar is sufficient, and closed reduction is not necessary. If displacement exceeds 30°, closed reduction is required, and percutaneous pinning using a Kirschner wire is performed if reduction is unsuccessful. Excessive manipulation should be avoided in pediatric cases to reduce the risk of growth plate disturbance.
Therapeutic Approaches for Olecranon Fractures
Nondisplaced olecranon fractures may be treated conservatively using orthotic immobilization with the elbow flexed at 90°. Displaced fractures warrant ORIF to restore articular congruity. Care must be taken due to the proximity of the ulnar nerve, which lies just medial to the olecranon and is at risk of injury.
Coronoid Fracture Management
Type I coronoid fractures may be managed conservatively without surgery. In contrast, types II and III typically require operative intervention with ORIF to restore elbow stability and prevent recurrent dislocation.
Transolecranon Fracture-Dislocation Treatment
This injury may present in 1 of 2 forms: simple (type I) or comminuted (type II). Both require surgical stabilization due to the disruption of the ulnohumeral articulation.
Interventions for Monteggia Fractures
Treatment of Monteggia fractures is influenced by patient age and fracture severity. In pediatric patients, conservative treatment using a long-arm cast in supination is often sufficient following acceptable closed reduction. Urgent ORIF is typically recommended in adults due to the higher risk of persistent instability and malalignment. Radiocapitellar alignment must be confirmed postreduction, as persistent dislocation or subluxation of the radial head can lead to long-term dysfunction.
Differential Diagnosis
The differential diagnosis for elbow pain includes several nonfracture conditions. Avulsion injuries may present with localized tenderness and limited motion. Olecranon bursitis causes swelling and pain, especially with pressure. Elbow dislocation can resemble a fracture and requires prompt recognition. Ligamentous sprains and tendinopathies, such as epicondylitis, should also be considered. Accurate diagnosis depends on clinical assessment and imaging. In young children, clinicians should also consider nonaccidental trauma when the history is inconsistent, even in the absence of fractures.
Prognosis
The prognosis for most patients with supracondylar fractures is generally favorable. However, outcomes tend to worsen with increasing fracture severity. Traumatic nerve injuries are typically transient and often resolve spontaneously.[28]
Complications
The 2 broad categories of complications most commonly associated with supracondylar humerus fractures are malunion and neurovascular injury. Several nerves and vascular structures lie in close proximity to the elbow, increasing the risk of compromise. The brachial artery bifurcates at the level of the radial neck into the radial and ulnar arteries, with the median nerve running closely adjacent. The ulnar nerve is particularly vulnerable at the medial epicondyle, while the PIN encircles the lateral neck of the radial head.
Neuropraxia, a temporary nerve injury, is the most frequent neurologic complication and typically resolves within 6 to 12 weeks. Nerve injury occurs in approximately 11% of supracondylar fractures, with the AIN most frequently affected, followed by the radial, median, and ulnar nerves.[29][30]
The anterior interosseous branch of the median nerve may be injured in extension-type fractures, often due to entrapment in surrounding muscle or fibrous tissue following anterior displacement of a proximal humeral fragment. This deficit may be assessed by testing flexion at the distal interphalangeal joint of the index finger. Posteromedial displacement may involve the radial nerve, while posterolateral displacement may affect the median nerve.
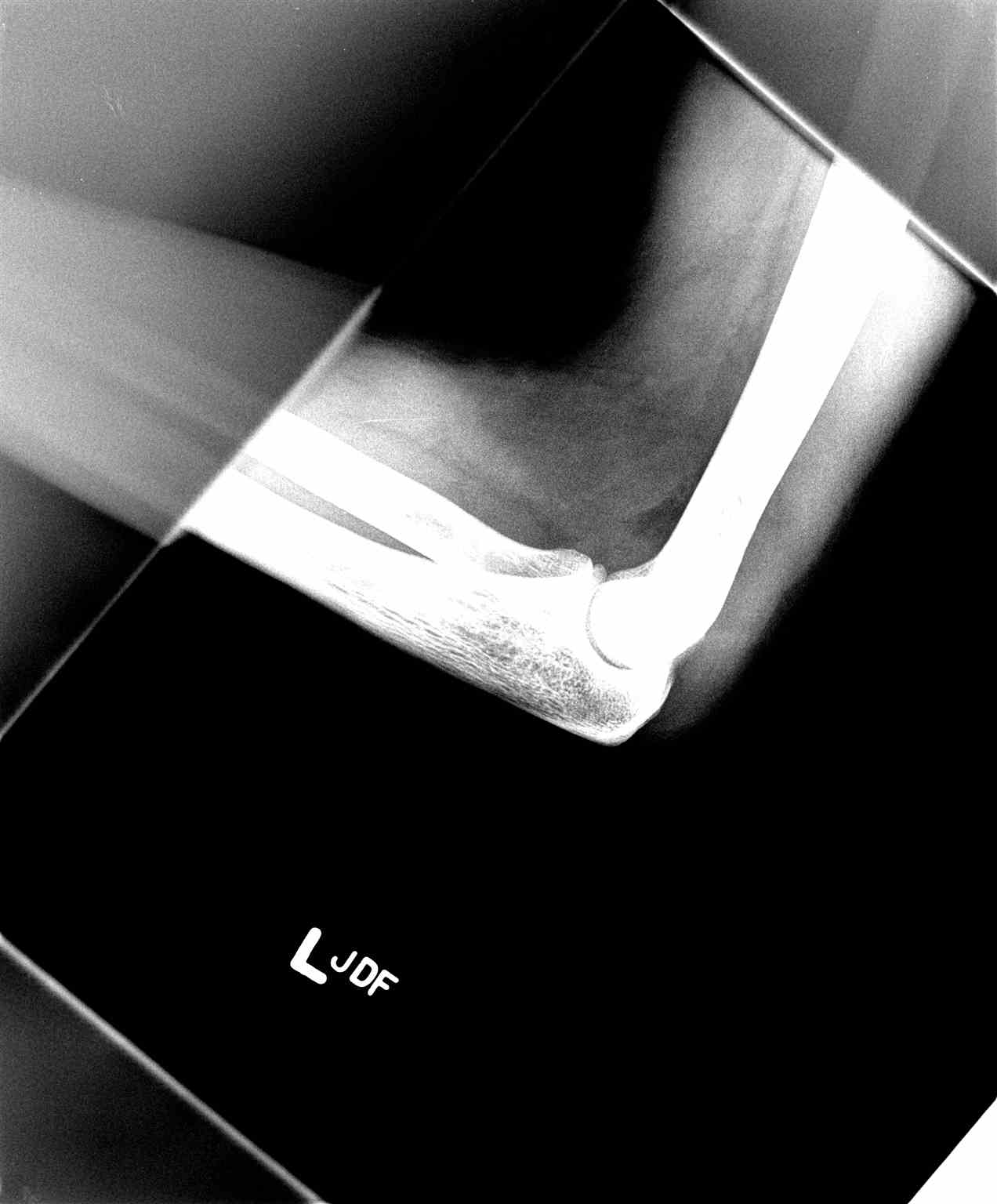
Flexion-type supracondylar fractures may involve the ulnar nerve, usually at the level of the medial epicondyle, due to posterior displacement of the proximal fragment (see Image. Elbow Fracture on Lateral Radiography). Motor testing reliably identifies AIN injury through the inability to form an “OK” sign using the thumb and index finger, indicating impairment of flexion at their distal interphalangeal joints. The PIN is at risk due to its anatomical course around the lateral radial neck.[31]
Vascular injury is another significant concern. Displacement of a supracondylar fracture may damage the brachial artery.[32] Even when the hand appears pink and well-perfused, vascular injury should still be suspected in the absence of a palpable radial pulse. Partial transection of the vessel may explain this phenomenon.
Compartment syndrome is a potential complication and must be identified early. An absent radial pulse warrants urgent evaluation. A Volkmann contracture may develop due to ischemic injury of the forearm resulting from brachial artery compromise. This ischemic injury may present with an inability to open the hand in children, pain with passive extension of the fingers, forearm tenderness, and absence of a radial pulse. Prompt recognition through careful neurovascular assessment is essential to prevent irreversible damage.
Malunion frequently complicates supracondylar fractures and can result in deformities such as cubitus valgus or cubitus varus. Loss of the carrying angle may lead to cubitus varus, also referred to as a “gunstock” deformity. Nonunion is more commonly associated with lateral condylar fractures, which often require revision surgery. Monteggia fracture-dislocation also carries an elevated risk of ulnar nonunion.[33]
Fractures around the elbow are also well known for resulting in joint stiffness. Early initiation of physical therapy is critical to preserving the ROM and optimizing functional recovery.
Postoperative and Rehabilitation Care
Careful evaluation of neurovascular status is essential following fracture reduction. Hospital admission may be required for continued monitoring. Follow-up with orthopedic and trauma surgery services should be arranged to guide ongoing care.
Early mobilization is critical to prevent joint stiffness, particularly after immobilization exceeding 2 weeks. Once clinical and radiographic evidence of healing is confirmed, a structured rehabilitation program should begin, focusing on ROM exercises and progressive strengthening. Rehabilitation should emphasize restoration of elbow extensor strength and joint mobility, as even minor deficits or posttraumatic stiffness can impair functional use. Referral to physical therapy is often indicated, especially in older children and adults, to optimize recovery and reduce the risk of long-term impairment.
Consultations
Immediate surgical or orthopedic consultation is indicated in cases of complex fractures, including Gartland types II to IV supracondylar fractures, unstable elbow joints, neurovascular compromise, and open fractures. Displaced fractures also require urgent evaluation, such as olecranon fractures with more than 2 mm of displacement, displaced coronoid fractures, or those involving more than 50% of the coronoid process. Vascular surgical consultation should be obtained promptly in the presence of vascular compromise. Surgical input is also necessary when compartment syndrome is suspected. Consultation with a radiologist may aid in interpretation, as pediatric elbow radiographs are often difficult to evaluate. Orthopedic evaluation is also essential in cases of Monteggia fracture-dislocation.
Deterrence and Patient Education
Protective measures should be emphasized to reduce the risk of elbow injuries, particularly in young children engaged in playground or sports activities. Proper supervision, use of age-appropriate equipment, and promotion of safe falling techniques can help prevent high-impact trauma. Early education on injury risks and safety practices is essential in reducing the incidence of fractures.
Families should be counseled about the potential for ROM loss following elbow fractures. Structured physical therapy is important to restore function and prevent long-term stiffness. Return to activity should be gradual and carried out under the supervision of orthopedic specialists to ensure safe and complete recovery.
Pearls and Other Issues
Pediatric elbow fractures present unique diagnostic and management challenges due to evolving anatomy and subtle radiographic findings. The following pearls highlight critical considerations to aid in accurate diagnosis and timely intervention:
- Arterial injury should always be suspected in supracondylar fractures, even if initial perfusion appears adequate. Both the brachial artery and median nerve should be evaluated, as these structures are in close proximity.
- Capitellum and radial head fractures may occur simultaneously. Both sites should be assessed in high-energy trauma.
- The posterior fat pad is always pathologic and may be the only radiographic clue to an occult fracture.
- Fat pads and alignment lines (eg, anterior humeral and radiocapitellar) should be assessed to improve detection of subtle injuries.
- Nondisplaced radial head fractures may be missed on initial radiographs. Clinical suspicion should be maintained, and advanced imaging should be considered if symptoms persist.
- The sequence and timing of ossification center appearance (CRITOE) should be understood to enhance recognition of subtle fractures.
- Compartment syndrome must be identified promptly. Early signs include agitation, anxiety, and increased analgesia requirements.
- Caution should be exercised when reducing type III supracondylar fractures to avoid tearing the intact periosteal hinge and creating a type IV injury.
- Loss of neurologic function after fracture reduction should prompt suspicion of nerve entrapment and should be addressed with urgent open exploration.
- Decreased limb perfusion in the setting of a fracture should be treated as a surgical emergency and evaluated immediately.
- Radiographs should be carefully assessed in suspected Monteggia injuries, as radial head dislocation may be subtle. Early recognition and treatment with ORIF should be performed in adults.
Mastery of these clinical insights helps reduce missed injuries, guide prompt interventions, and support safe recovery. Optimizing care for pediatric elbow fractures requires both systematic evaluation and high clinical suspicion.
Enhancing Healthcare Team Outcomes
Elbow fractures are managed by an interprofessional team comprising emergency physicians, orthopedic surgeons, nurses, radiologists, and physical therapists. Neurovascular complications frequently accompany these injuries and must be identified early. Nondisplaced fractures are typically treated conservatively, while all displaced fractures require surgical intervention. Extensive rehabilitation is often necessary to restore strength and ROM. A subset of patients may continue to experience restricted mobility and persistent pain despite complete recovery.[34] Timely recognition of unstable fracture patterns helps prevent chronic instability and reduces the likelihood of future corrective procedures.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
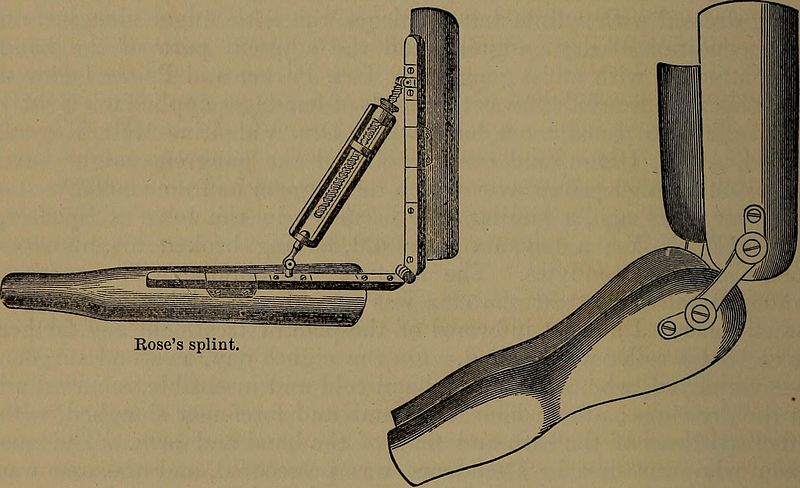
Rose and Welch Splints. The Rose splint is shown on the left, while the Welch splints are illustrated on the right. These devices were historically used to immobilize elbow fractures and may be applied in select stable injuries, such as nondisplaced medial epicondyle fractures, but are not suitable for supracondylar fractures.
Contributed by Wikimedia Commons, (Public Domain)
(Click Image to Enlarge)

Posterior Fat Pad Sign in Supracondylar Fracture. A posteriorly displaced distal humeral fragment is visible, consistent with a supracondylar fracture. The posterior fat pad is elevated and radiolucent, indicating an intra-articular effusion that often accompanies occult or subtle fractures.
Contributed by Wajeeha Saeed, MD
(Click Image to Enlarge)

Elbow Fracture on Lateral Radiography. A posterior dislocation of the elbow joint is visualized, with misalignment between the distal humerus and proximal forearm bones. This injury typically results from high-energy trauma and may be associated with fractures of the radial head, coronoid process, or olecranon.
Contributed by W Saeed, MD
(Click Image to Enlarge)
(Click Image to Enlarge)
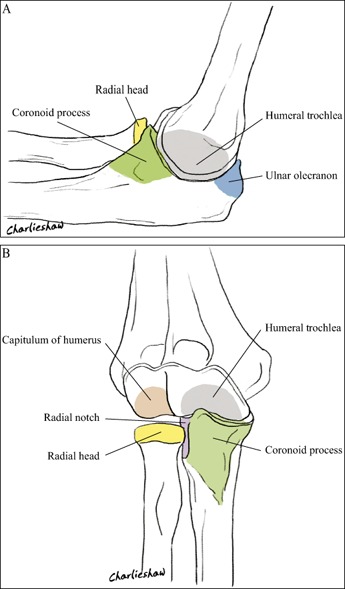
Medial and Volar Views of the Right Elbow. Image A shows a medial view of the proximal ulna and radius in relation to the humeral trochlea and radial head, highlighting the coronoid process, olecranon, and trochlea. Image B presents a volar (anterior) view of the right elbow joint, depicting the capitulum and trochlea of the humerus, radial head, coronoid process, and radial notch.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6583215/
(Click Image to Enlarge)
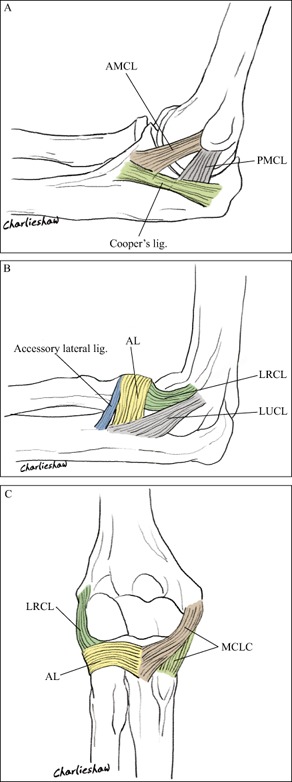
Ligamentous Anatomy of the Right Elbow. This illustration displays the ligamentous structures of the right elbow in 3 views. Image A highlights the anterior and posterior bundles of the medial collateral ligament (AMCL, PMCL) and the Cooper ligament. Image B demonstrates the lateral radial collateral ligament (LRCL), lateral ulnar collateral ligament (LUCL), accessory lateral ligament, and annular ligament (AL). Image C presents a composite view, with the medial collateral ligament complex (MCLC) on the right and the LRCL and annular ligament on the left.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6583215/
(Click Image to Enlarge)
References
Manidakis N, Sperelakis I, Hackney R, Kontakis G. Fractures of the ulnar coronoid process. Injury. 2012 Jul:43(7):989-98. doi: 10.1016/j.injury.2011.08.030. Epub 2011 Sep 29 [PubMed PMID: 21963158]
Morrey BF, An KN. Stability of the elbow: osseous constraints. Journal of shoulder and elbow surgery. 2005 Jan-Feb:14(1 Suppl S):174S-178S [PubMed PMID: 15726078]
Schneeberger AG, Sadowski MM, Jacob HA. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. The Journal of bone and joint surgery. American volume. 2004 May:86(5):975-82 [PubMed PMID: 15118040]
Landin LA,Danielsson LG, Elbow fractures in children. An epidemiological analysis of 589 cases. Acta orthopaedica Scandinavica. 1986 Aug [PubMed PMID: 3788491]
Level 2 (mid-level) evidenceLenz R, Bonacker J, Mittelmeier W, Ellenrieder M, Tischer T. [What do orthopedic and trauma surgeons expect from radiologists when interpreting imaging of the elbow?]. Der Radiologe. 2018 Nov:58(11):968-975. doi: 10.1007/s00117-018-0456-7. Epub [PubMed PMID: 30225771]
Gierer P, Rocher S, Wichelhaus A, Rotter R. [Typical fractures and dislocations of the elbow joint and their treatment]. Der Radiologe. 2018 Nov:58(11):976-984. doi: 10.1007/s00117-018-0449-6. Epub [PubMed PMID: 30194639]
Stromberg JD. Care of Water Polo Players. Current sports medicine reports. 2017 Sep/Oct:16(5):363-369. doi: 10.1249/JSR.0000000000000409. Epub [PubMed PMID: 28902761]
Carità E, Donadelli A, Cugola L, Perazzini P. Radial head prosthesis: results overview. Musculoskeletal surgery. 2017 Dec:101(Suppl 2):197-204. doi: 10.1007/s12306-017-0492-x. Epub 2017 Aug 14 [PubMed PMID: 28808982]
Level 3 (low-level) evidenceHo CA. Cubitus Varus-It's More Than Just a Crooked Arm! Journal of pediatric orthopedics. 2017 Sep:37 Suppl 2():S37-S41. doi: 10.1097/BPO.0000000000001025. Epub [PubMed PMID: 28799993]
Zwingmann J, Neumann MV, Hammer TO, Reising K, Südkamp NP. Comminuted Fracture of Elbow - Ostheosynthesis vs. Total Joint Replacement. Acta chirurgiae orthopaedicae et traumatologiae Cechoslovaca. 2016:83(4):231-237 [PubMed PMID: 28026723]
Kodde IF, Kaas L, Flipsen M, van den Bekerom MP, Eygendaal D. Current concepts in the management of radial head fractures. World journal of orthopedics. 2015 Dec 18:6(11):954-60. doi: 10.5312/wjo.v6.i11.954. Epub 2015 Dec 18 [PubMed PMID: 26716091]
Surd A, Muresan R, Ciongradi CI, Sur LM, Ardelean LR, Usatiuc LO, Snakovszki K, Munteanu C, Sârbu I. Modern Treatment of Supracondylar Humeral Fractures in Children. Children (Basel, Switzerland). 2025 Apr 25:12(5):. doi: 10.3390/children12050556. Epub 2025 Apr 25 [PubMed PMID: 40426735]
Saris TFF, Eygendaal D, The B, Colaris JW, van Bergen CJA. Lateral Humeral Condyle Fractures in Pediatric Patients. Children (Basel, Switzerland). 2023 Jun 8:10(6):. doi: 10.3390/children10061033. Epub 2023 Jun 8 [PubMed PMID: 37371265]
Burkhart RJ, Kolin DA, Fabricant PD, Liu RW, Mistovich RJ. Less common than expected: late displacement after minimally displaced pediatric lateral condyle fractures of the elbow. Journal of pediatric orthopedics. Part B. 2024 Mar 1:33(2):130-135. doi: 10.1097/BPB.0000000000001085. Epub 2023 Apr 11 [PubMed PMID: 37040657]
Rasool MN. Dislocations of the elbow in children. The Journal of bone and joint surgery. British volume. 2004 Sep:86(7):1050-8 [PubMed PMID: 15446537]
Ramponi DR. Monteggia Fracture-Dislocation. Advanced emergency nursing journal. 2022 Jan-Mar 01:44(1):29-33. doi: 10.1097/TME.0000000000000389. Epub [PubMed PMID: 35089278]
Al-Ani Z, Tham JL, Ooi MWX, Wright A, Ricks M, Watts AC. The radiological findings in complex elbow fracture-dislocation injuries. Skeletal radiology. 2022 May:51(5):891-904. doi: 10.1007/s00256-021-03900-x. Epub 2021 Sep 4 [PubMed PMID: 34480618]
Dailiana ZH, Papatheodorou LK, Michalitsis SG, Varitimidis SE. Pediatric terrible triad elbow fracture dislocations: report of 2 cases. The Journal of hand surgery. 2013 Sep:38(9):1774-8. doi: 10.1016/j.jhsa.2013.05.030. Epub 2013 Jul 23 [PubMed PMID: 23890394]
Level 3 (low-level) evidenceGoldflam K. Evaluation and treatment of the elbow and forearm injuries in the emergency department. Emergency medicine clinics of North America. 2015 May:33(2):409-21. doi: 10.1016/j.emc.2014.12.010. Epub [PubMed PMID: 25892729]
Ring D, Jupiter JB. Fracture-dislocation of the elbow. The Journal of bone and joint surgery. American volume. 1998 Apr:80(4):566-80 [PubMed PMID: 9563387]
Duckworth AD, Clement ND, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of fractures of the proximal ulna. Injury. 2012 Mar:43(3):343-6. doi: 10.1016/j.injury.2011.10.017. Epub 2011 Nov 9 [PubMed PMID: 22077988]
Emery KH, Zingula SN, Anton CG, Salisbury SR, Tamai J. Pediatric elbow fractures: a new angle on an old topic. Pediatric radiology. 2016 Jan:46(1):61-6. doi: 10.1007/s00247-015-3439-0. Epub 2015 Jul 28 [PubMed PMID: 26216157]
Bryce CD, Armstrong AD. Anatomy and biomechanics of the elbow. The Orthopedic clinics of North America. 2008 Apr:39(2):141-54, v. doi: 10.1016/j.ocl.2007.12.001. Epub [PubMed PMID: 18374805]
Morrey BF. Current concepts in the management of complex elbow trauma. The surgeon : journal of the Royal Colleges of Surgeons of Edinburgh and Ireland. 2009 Jun:7(3):151-61 [PubMed PMID: 19580179]
Vinson DR, Kann GS, Gaona SD, Panacek EA. Performance of the 4-way range of motion test for radiographic injuries after blunt elbow trauma. The American journal of emergency medicine. 2016 Feb:34(2):235-9. doi: 10.1016/j.ajem.2015.10.031. Epub 2015 Oct 24 [PubMed PMID: 26597495]
Ashoobi MA, Homaie Rad E, Rahimi R. The diagnostic value of sonographic findings in pediatric elbow fractures: A systematic review and meta-analysis. The American journal of emergency medicine. 2024 Mar:77():121-131. doi: 10.1016/j.ajem.2023.12.021. Epub 2023 Dec 20 [PubMed PMID: 38142484]
Level 1 (high-level) evidenceSkaggs DL, Cluck MW, Mostofi A, Flynn JM, Kay RM. Lateral-entry pin fixation in the management of supracondylar fractures in children. The Journal of bone and joint surgery. American volume. 2004 Apr:86(4):702-7 [PubMed PMID: 15069133]
Level 2 (mid-level) evidenceRamachandran M, Birch R, Eastwood DM. Clinical outcome of nerve injuries associated with supracondylar fractures of the humerus in children: the experience of a specialist referral centre. The Journal of bone and joint surgery. British volume. 2006 Jan:88(1):90-4 [PubMed PMID: 16365127]
Level 2 (mid-level) evidenceGómez JE. Upper extremity injuries in youth sports. Pediatric clinics of North America. 2002 Jun:49(3):593-626, vi-vii [PubMed PMID: 12119867]
Peters P. Orthopedic problems in sport climbing. Wilderness & environmental medicine. 2001 Summer:12(2):100-10 [PubMed PMID: 11434485]
Kokkalis ZT, Ballas EG, Mavrogenis AF, Soucacos PN. Distal biceps and triceps ruptures. Injury. 2013 Mar:44(3):318-22. doi: 10.1016/j.injury.2013.01.003. Epub 2013 Jan 23 [PubMed PMID: 23352149]
Baratz M, Micucci C, Sangimino M. Pediatric supracondylar humerus fractures. Hand clinics. 2006 Feb:22(1):69-75 [PubMed PMID: 16504779]
Gonzalez LJ, Shields CN, Leucht P, Konda SR, Egol KA. Fracture-Dislocations of the Elbow: A Comparison of Monteggia and Terrible Triad Fracture Patterns. Orthopedics. 2023 May:46(3):158-163. doi: 10.3928/01477447-20221129-07. Epub 2022 Dec 2 [PubMed PMID: 36476213]
Swensen SJ, Tyagi V, Uquillas C, Shakked RJ, Yoon RS, Liporace FA. Maximizing outcomes in the treatment of radial head fractures. Journal of orthopaedics and traumatology : official journal of the Italian Society of Orthopaedics and Traumatology. 2019 Mar 23:20(1):15. doi: 10.1186/s10195-019-0523-5. Epub 2019 Mar 23 [PubMed PMID: 30904970]