Introduction
Herniated nucleus pulposus (HNP) is a common cause of back pain resulting from the displacement of the nucleus pulposus from its normal position within the intervertebral space. Patients often experience pain and recall an event that triggered the condition. Unlike mechanical back pain, herniated disk–related pain is typically characterized by a burning or stinging sensation and may radiate into the extremities. In severe cases, the herniation is associated with weakness, sensory abnormalities, and bowel and bladder dysfunction. The nucleus pulposus supports the spine by acting as a shock-absorbing cushion. In some instances, a herniated disk can compress the nerve or the spinal cord, causing pain, symptoms of nerve compression, or spinal cord dysfunction, also known as myelopathy.
Unfortunately, effective conservative treatment options for HNP are limited. However, most cases of disk herniation resolve in a few weeks. Furthermore, a disk herniation may be asymptomatic and discovered incidentally on an MRI. Imaging studies are not indicated in a patient without red flag signs unless symptoms persist for 6 weeks, and MRI is the imaging modality of choice. Most herniated disks improve with conservative treatment, but refractory cases may require interventional or surgical repair. Epidural corticosteroid injections are effective for short-term pain management of a disk herniation. Surgical diskectomy is more effective than conservative management during the first year of symptoms; surgical intervention is less effective after 1 year.[1][2][3] Clinicians should monitor for severe or rapidly progressing neurological changes, as this would indicate urgent neurosurgical referral.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
HNP occurs when part or all of the nucleus pulposus protrudes through the annulus fibrosus. The most common cause of disk herniation is degeneration of the nucleus pulposus, which is associated with the progressive dehydration and instability of the disk that occur with age, eventually leading to symptoms. The second most common cause of disk herniation is trauma. Other causes include connective tissue disorders and congenital disorders such as short pedicles.
Disk herniation is most common in the lumbar spine, followed by the cervical spine, due to biomechanical stress in these more flexible areas. Factors associated with the development of lumbar disk herniation with radiculopathy include middle age (eg, 30–50 years), smoking, higher BMI, the presence of cardiovascular risk factors (in women), and a greater cumulative occupational lumbar load from forward bending postures and manual materials handling.[4] Conversely, the thoracic spine has a lower rate of disk herniation.[5][6]
Epidemiology
The incidence of HNP is 5 to 20 cases per 1000 adults annually, predominantly affecting individuals aged 30 to 50, and the ratio of men to women is approximately 2:1.[7] Patients with heriated lumbar disks represent 1% to 3% of the population, depending on age and sex. According to the Spine Patient Outcomes Research Trial, the average age of onset is 41, and it is more common in men. The most commonly affected disk levels are L4 to L5 and L5 to S1, accounting for approximately 95% of cases in adults between 25 and 55 years old.[8][9]
Risk factors include obesity, physical and high-stress occupations, as well as medical comorbidities like diabetes, hyperlipidemia, and a history of smoking [Seminars in Spine Surgery. The epidemiology and pathophysiology of lumbar disc herniation. 2016]. Despite the high prevalence of disk herniation, degenerative disk disease is the underlying cause in less than 5% of patients with back pain.[10] Furthermore, not all lumbar back pain results from disk disease; other etiologies include facet-mediated, myofascial, or visceral conditions; compression fractures; and Schmorl nodes.
Pathophysiology
The pathophysiology of disk herniations involves mechanical, degenerative, and biochemical processes. Degeneration of the intervertebral disks with age predisposes them to injuries. Alterations in capillaries, cell morphology, density within the nucleus pulposus (NP), and the formation of small clefts in the annulus fibrosus (AF) begin early in life. The outer layer of the AF, which prevents herniation, begins to degenerate later in life. Herniation occurs when the NP bulges through the AF, affecting portions of the AF and sometimes the cartilaginous endplate.[Semin in Spine Surg. The epidemiology and pathophysiology of lumbar disc herniation. 2016] The disk herniation may also cause Modic endplate changes, which are alterations in the bone marrow of the vertebral endplates, as seen on MRI. Modic changes are categorized as type 1 (associated with inflammation and edema in the vertebral endplate) or type 2 (characterized by changes indicative of fatty degeneration of the bone marrow). Both types contribute to low back pain.[11]
Most herniations occur posterolaterally at the weaker points of the AF, which lack structural support from the longitudinal ligaments. Herniations at this location increase the likelihood of nerve root compression. This mechanical compression and an inflammatory response involving chemokines such as tumor necrosis factor-α and interleukin-1 contribute to both pain and degeneration. Elevated levels of fibroblast growth factor and other cytokines attract macrophages that resorb the herniated disk material but also contribute to radicular symptoms by chemically irritating the nerve roots. Large herniations exhibit increased nerve irritation and inflammation-induced changes in the nerve roots (edema and myelin changes) due to higher levels of these cytokines, which promote inflammation and disk resorption.[12][13][14][15]
A healthy disk is typically 7 to 10 mm thick and 4 cm in diameter in the lumbar region, with approximately 20 layers of lamellae.[16] In cases of disk degeneration, this height is lost, and the lamellae degenerate, usually posterolaterally along the posterior longitudinal ligament. The outer third of the lamellae is most richly innervated, so herniation in this area causes more neurogenic symptoms. Another pathological factor is the pH of the disk. A healthy mammalian disk pH is usually 7.2; degenerative disks may have a pH as low as 5.2. Patients with abnormal disk pH may have symptoms due to chemical irritation and present with pain contralateral to the herniation.[17]
Radicular features are present if a posterolateral herniation compromises the lateral foramen or directly compresses a spinal nerve. A disk herniation in the midline or a stenotic region could compress the cauda equina, resulting in myelopathy. A combination of HNP and ligamentum flavum thickening, a congenitally narrowed pedicle (short pedicle syndrome), or narrowing due to autoimmune diseases can compress the spinal cord above the cauda equina, causing myelopathy. If the narrowing is at the level of the conus medullaris, a classic conus medullaris syndrome with symptoms of saddle anesthesia may be present on physical examination. However, rare cases of pure conus medullaris syndrome without cauda equina involvement presenting with isolated bowel and bladder incontinence have been reported.[17]
Histopathology
The annulus fibrosus is a laminated fibrous ring composed of collagen and other proteins. The nucleus pulposus is a gelatinous substance rich in water and proteoglycans. Histologic changes to the cartilaginous endplate (CE) contribute to the degeneration and herniation of intervertebral disks. Microscopic changes include abnormal cellular clusters, empty lacunae, extensive neovascularization, and apoptotic, necrotic, and senescent cells. Loss of endplate thickness, avulsions, cracks, fissures, loss of normal matrix staining, fibrosis, and calcification are also observed on histologic examination of CEs in symptomatic individuals. Furthermore, pain scores were higher in patients with vascular mimicry, herniation into the CE, the presence of bone tissue in the CE, and traumatic nodes.[18]
In one study, cartilaginous endplates in herniated disks were evaluated and compared with clinical symptoms and postoperative outcomes. The cellular and tissue composition of herniated disks varied across different age groups and correlated with the severity of symptoms. CE abnormalities were observed with increasing age and were more frequently detected in patients with Modic changes on imaging studies (P < .001). A higher proportion of lumbar disk herniation with a 20% or greater occupancy rate (eg, CEs with a greater content of water and other substances) was found in patients younger than 50 (P = .009). These changes were associated with decreased motor strength preoperatively (P = .007). The postoperative visual analog scale score for low back pain was higher in patients with CE abnormalities than those without in patients older than 50 (P < .001). In multiple regression analysis, CE abnormalities were independently associated with residual low back pain at 1 year postoperatively in older patients (β= .46, P < .001). The study also stated that avulsion-type herniations in patients younger than 50 had a higher CE occupancy rate, which was a potential cause of preoperative motor weakness. Clinical outcomes following diskectomy improved regardless of the presence of CE abnormalities; however, cartilaginous herniation in patients aged 50 or older may affect residual low back pain at 1 year.[19]
Toxicokinetics
Although there is no specific toxin known to directly target intervertebral disks and cause herniation in isolation, nicotine, most heavy metals, and excessive alcohol intake are associated with advanced spinal disk degeneration.[20]
History and Physical
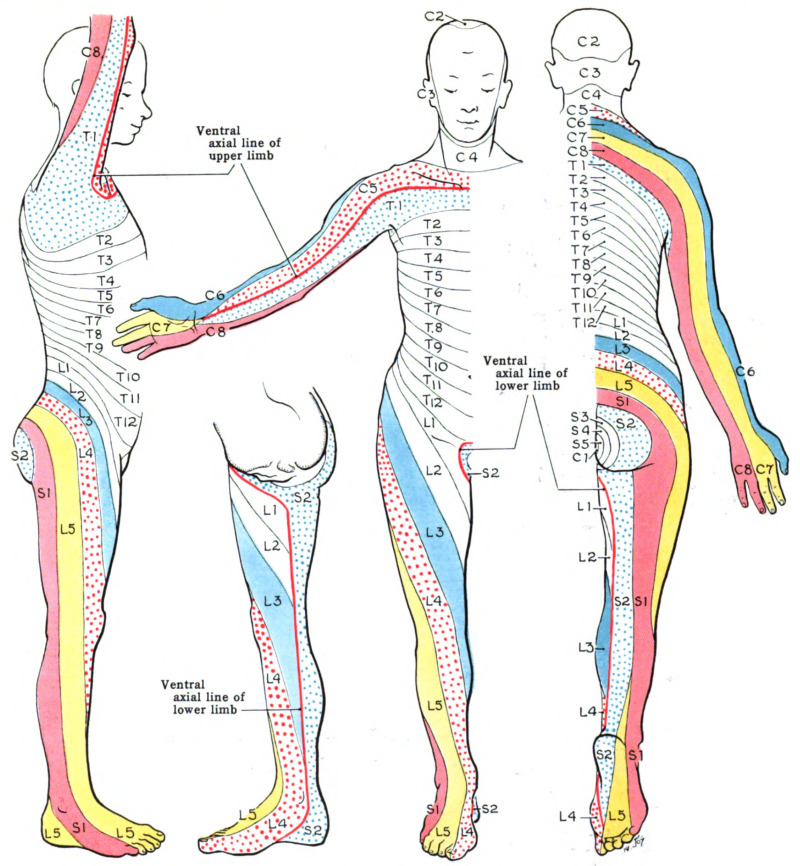
The history and physical examination should focus on screening for "red flag" signs and symptoms.[21] The patient will likely recall an inciting injury, often due to lifting or twisting. Pain is frequently described as sharp or burning, and usually radiates along the distribution of the compressed nerve root (see Image. Dermatomes). Numbness, tingling, and decreased sensation along the path of the nerve root may also occur; in more severe cases, weakness or instability may be present during ambulation.
Cervical Spine
- History
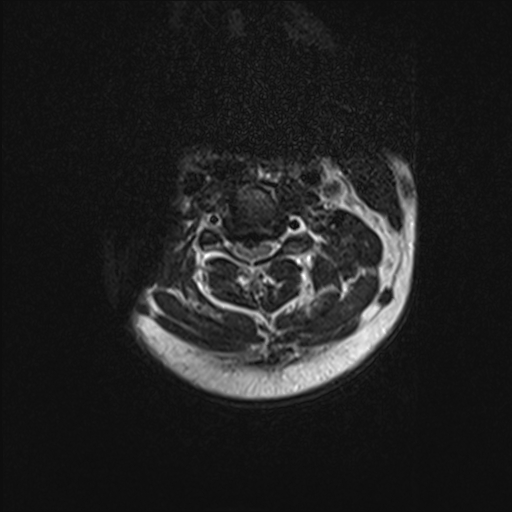
- The C6 to C7 level of the cervical spine is the most common site of a herniated disk causing radiculopathy (see Image. Cervical Spine, Magnetic Resonance Image). The history should include the chief concern, onset of symptoms, location, and radiating pattern of pain, and any past treatments.
- Physical examination
- On physical examination, particular attention should be given to areas of weakness, sensory abnormalities, and the corresponding myotome and dermatome distribution. Red flags or signs of spinal cord dysfunction should also be evaluated. Facet-loading maneuvers can help differentiate between disk pathology and facet pain.
Typical findings of a solitary nerve lesion due to compression by a herniated disk in the cervical spine:
- C5 nerve: Neck, shoulder, and scapular pain; lateral arm numbness; weakness of shoulder abduction, external rotation, elbow flexion, and forearm supination
- Abnormal biceps and brachioradialis reflexes
- C6 nerve: Neck, shoulder, scapular, lateral arm, forearm, and hand pain; lateral forearm, first and second digit numbness.
- Weakness of shoulder abduction, external rotation, elbow flexion, forearm supination, and pronation
- Abnormal biceps and brachioradialis reflexes
- C7 nerve: Neck, shoulder, and third digit pain, numbness of the second, third, fourth, and volar hand
- Weakness of the elbow and wrist extensors, forearm pronation, and wrist flexion
- Abnormal triceps reflex
- C8 nerve: Neck, shoulder, and medial forearm pain, numbness of the medial forearm and medial hand
- Weakness of digit extension, wrist (ulnar) extension, and distal digit flexion, extension, abduction, and adduction
- Reflexes: Typically not affected
- T1 nerve: Pain in the neck, medial arm, and forearm, with numbness of the anterior and medial forearm
- Weakness of the first digit abduction; distal finger flexion, abduction, and adduction
- Reflexes are not typically affected.
Thoracic Spine
Intervertebral disk degeneration may cause diskogenic pain. Thoracic disk lesions most often occur in the lower thoracic spine. Approximately 75% occur below the level of T8, with T11 to T12 the most common.
- History
- Most thoracic disk herniations are asymptomatic and discovered incidentally on MRI. Unlike lumbar and cervical disk herniations, thoracic disk herniations often present with atypical symptoms and are frequently diagnosed by exclusion.
- Physical examination
- Patients may have sensory changes. Severe findings include gait disturbances, paralysis, and cardiovascular abnormalities.
Lumbar Spine
- History
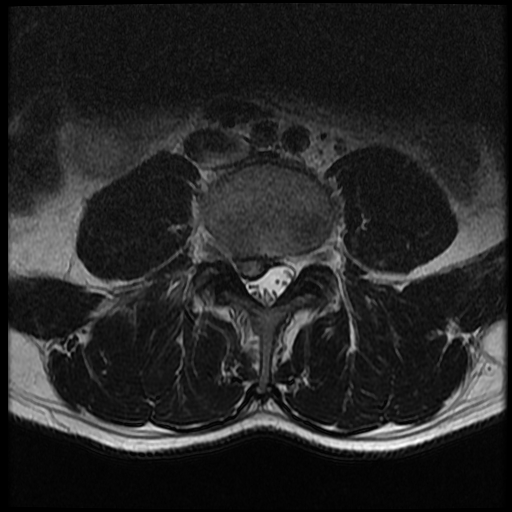
- A herniated lumbar disk typically presents with sensory and motor abnormalities localized to a specific myotome (see Image. Lumbar Spine Disk Herniation, Magnetic Resonance Image). The history should include the chief concern, the onset of symptoms, the location and radiating pattern of pain, and any past treatments.
- Physical examination
- A careful neurologic examination may localize the level of compression. The sensory loss, weakness, pain location, and reflex changes associated with the corresponding levels are described below. Facet-loading maneuvers can help differentiate disk herniation from facet joint–mediated pain.
Typical findings of a solitary nerve lesion due to compression by a herniated disk in the lumbar spine
- L1 nerve: Pain and sensory loss in the inguinal region
- Hip flexion weakness is rare, and the stretch reflex is typically abnormal
- L2-L4 nerves: Back pain radiating to the anterior thigh and medial lower leg; sensory loss of the anterior thigh and sometimes medial lower leg; hip flexion and adduction weakness; knee extension weakness; and decreased patellar reflex
- L5 nerve: Back pain radiating to the buttock, lateral thigh, lateral leg, dorsum of the foot, and hallux; sensory deficit of the lateral lower leg, dorsum of the foot, webspace of first and second digits of the foot; weakness of hip abduction, knee flexion, ankle dorsiflexion, digit of the foot extension and flexion, foot inversion and eversion; decreased semitendinosus/semimembranosus reflex
- S1 nerve: Back pain radiating to the buttock, lateral or posterior thigh, posterior leg, and lateral or plantar foot
- Sensory deficit of the posterior leg and the lateral or plantar aspect of the foot
- Weakness of hip extension, knee flexion, plantar flexion, and ankle plantar flexion of the foot
- Decreased Achilles reflex; severe cases may have weakness of the medial buttock, perineal, and perianal region
- Urinary and fecal incontinence, sexual dysfunction (may be present)
- S2-S4 nerves: Sacral or buttock pain radiating to the posterior aspect of the leg or the perineum; sensory deficit of the medial buttock, perineal, and perianal region; absent bulbocavernosus and anal wink reflexes
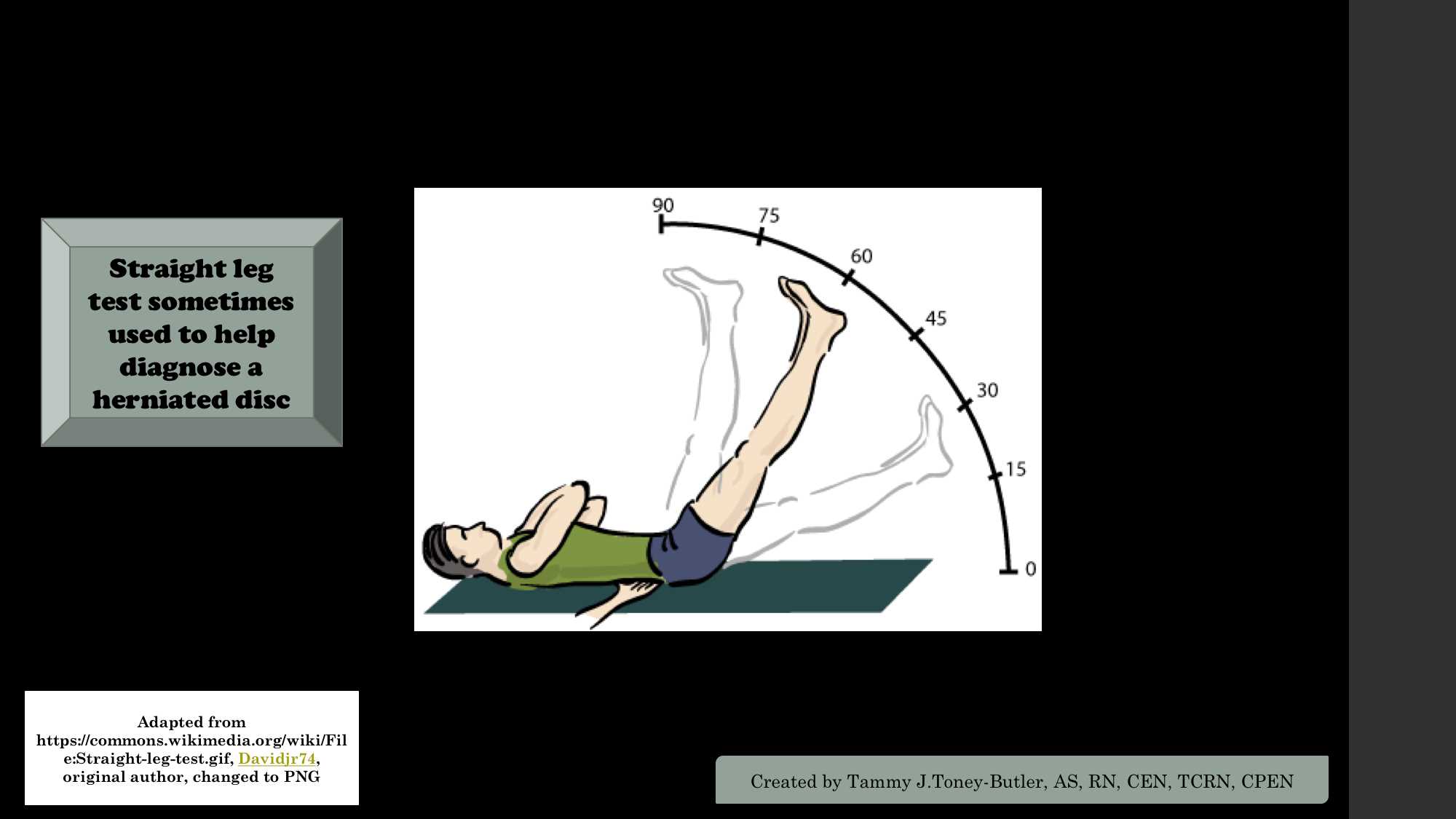
The straight-leg raise test: With the patient lying supine, the clinician slowly elevates the patient's leg with the knee extended. The test result is positive if it reproduces pain and paresthesia in the extended leg (See Image. Straight Leg Test).[22]
The contralateral (crossed) straight-leg raise test: The clinician elevates the asymptomatic leg with the patient in the supine position. The test result is positive if the maneuver reproduces pain and paresthesia in the extended leg. The test has a specificity of more than 90%. The distribution of radiating pain is usually a diagnostically valuable indicator. However, this finding does not reliably differentiate between L5 and S1 radiculopathy.[23] Notably, disk herniation can affect any level distal to the lesion, and far lateral herniations irritate the nerve root at that level. For example, a disk herniation at L2 to L3 can result in an isolated L5 radiculopathy.[24]
Evaluation
Over 85% of symptoms of acute herniated disks will resolve within 8 to 12 weeks with conservative management. However, patients who have an abnormal neurologic examination or do not improve with conservative therapy will need further evaluation and treatment.[25][26][27]
Imaging Studies
- Radiography: This imaging technique can identify structural instability with flexion-extension views and diagnose anterolisthesis, characterized by a loss of disk height. Radiographs can also provide insight into fractures and endplate changes, although they do not differentiate between Modic types 1 and 2. However, x-rays cannot provide information on nerve compression or disk herniation. A computed tomography or MRI scan is warranted if radiographs show an acute fracture.
- Computed tomography: This imaging is the preferred study for visualizing bony structures in the spine. CT scans can also show calcified herniated disks. Compared to radiography, CT is less accessible in outpatient settings but more readily available than MRIs. Furthermore, CT myelography is a diagnostic alternative for herniated disks in patients with implanted devices incompatible with MRI.
- Magnetic resonance imaging: MRI is the preferred and most sensitive study for visualizing herniated disks. MRI findings can help surgeons and other clinicians plan procedures and evaluate for malignancy, infection, abscess, and Modic endplate changes.
Treatment / Management
Conservative Treatments
Acute cervical and lumbar radiculopathies due to a herniated disk are primarily managed with nonsurgical treatments. Nonsteroidal anti-inflammatory drugs and physical therapy are first-line therapies. However, physical therapy is not recommended at the initial onset of symptoms. Most cases of disk herniation resolve within a few weeks; thus, it is not recommended to start physical therapy until symptoms persist for at least 3 weeks. Patients who do not improve with conservative treatment or have neurologic deficits require timely surgical referral.[28][29][30][31]
There is limited evidence to support the use of muscle relaxants, such as cyclobenzaprine, or oral corticosteroids.[32] For cases of severe pain unresponsive to over-the-counter pain medication, opioid analgesics may be considered. However, the adverse effects, risks, and benefits of opioids should be discussed with the patient, and they should only be used for a short duration. Moreover, translaminar epidural injections and selective nerve root blocks are second-line modalities after conservative management, and are indicated for patients who have had symptoms for at least 4 to 6 weeks. There is limited evidence on the efficacy of epidural injections beyond 3 months; however, repeat injections may be considered.[33][34](A1)
Interventional Pain Management
Interventional pain management consists of a spectrum of treatments that overlap with minimally invasive spinal procedures. Trigger point injections are initially performed to treat the soft tissue component of pain and avoid the systemic effects of exogenous corticosteroids. More advanced methods, such as epidural corticosteroid injections, are performed via an interlaminar, transforminal (severe unilateral radiculopathy), or caudal approach with or without a caudal-based catheter. These procedures can be performed concurrently with epidural lysis of adhesions (more common in postlaminectomy cases) or on separate occasions, depending on whether the pain is axial or radicular in origin. The decision is also based on physical examination findings and, in some cases, electromyography.
More advanced procedures, such as the Intracept procedure, treat the sinuvertebral nerves and denervate the vertebral endplates, particularly in patients with Modic endplate changes. A less standard procedure, intradiscal electrothermal annuloplasty, has essentially fallen out of favor. However, this procedure involved placing a radiofrequency ablation catheter into the NP using a lateral discogram approach, allowing it to wrap around the posterior annulus, and performing a thermal denervation. Some clinicians use the same radiofrequency lesion generator for facet medial branch block and radiofrequency ablation, directing the catheter to the lateral vertebral body and ablating the sinuvertebral nerves. Radiofrequency ablation is typically performed after a successful diagnostic block, whether of the facet joint, sinuvertebral nerve, or more peripheral areas.
Several brands of minimally invasive disk decompression devices, such as the Wolfe endoscopic system. This device features a variety of 1- to 3-mm tools, including a channel for a working tool, light, and water flow. Another device, the DeKompressor, is a handheld, self-contained device powered by a 9-V battery and a simple motor that spins a fixed 1 mm Auger inside a 14-gauge needle in the disk. This device operates on the Archimedes screw principle, removing disk material into a clear reservoir. Using a classic diskogram approach, both devices enter the disk unilaterally, but may also be performed bilaterally.[35]
Medication Management
Medication management encompasses a spectrum of options ranging from anti-inflammatory drugs to narcotic analgesics. Nonsteroidal anti-inflammatory drugs may be helpful initially, but they have several complications (such as renal failure). Muscle relaxants may be beneficial, especially at night, for helping to restore the sleep-wake cycle. Membrane stabilizers (such as anticonvulsants and antidepressants) are often helpful for severe pain radiating down the limb, leg, or other dermatome. Membrane stabilizers can also overlap with other membrane stabilizers and help with sleep. Opioid medications can be helpful for severe pain, but are controversial. There are regional, geographic, administrative, legal, regulatory, and opinion differences as to whether opioids should be used for acute low back pain.
Osteopathic Manipulation
Osteopathic manipulation has been studied extensively for over a century, and is typically performed by specialized osteopathic clinicians. Osteopathic manipulation can reduce the size of the disk herniation, increase function, and decrease pain.[36] (B3)
Surgical Treatments
Surgical treatment is the last resort when managing a disk herniation. Depending on the clinical presentation, surgical procedures for a herniated disk include laminectomies or discectomies. For cervical spine herniations, anterior cervical decompression and fusion may be required. An artificial disk replacement can also be considered. Surgical procedures for the lumbar spine include a lateral or anterior approach for diskectomy and fusion. The benefits of surgical intervention are moderate and tend to decrease over time.[37] (A1)
Differential Diagnosis
The differential diagnoses for a herniated disk include:
- Cardiac angina
- Cauda equina syndrome
- Compression fracture
- Degenerative spinal stenosis
- Diabetic amyotrophy
- Diskal cyst
- Epidural abscess
- Epidural hematoma
- Infectious diskitis=
- Mechanical back pain
- Metastatic disease
- Neurinoma
- Noncardiac angina
- Osteophytes
- Parsonage-Turner syndrome (brachial neuritis)
- Peripheral nerve entrapment
- Posterior annular tear
- Severe length–dependent peripheral neuropathy
- Synovial cyst
- Thoracic outlet syndrome
Many of these conditions can be excluded with MRI and clinical assessment.
Pertinent Studies and Ongoing Trials
Antagonism or Reduction of Local Inflammatory Mediators
Sustained inflammation is the pathophysiological basis for intervertebral disk degeneration. Effective antagonism or reduction of local inflammatory mediators may help regulate the microenvironment and reshape the extracellular matrix of the disk. One novel therapy is an immunomodulatory hydrogel microsphere system, combining cell membrane–coated mimic technology and surface chemical modification methods by grafting neutrophil membrane–coated polylactic-glycolic acid copolymer nanoparticles loaded with transforming growth factor-β1 onto the surface of methacrylic acid gelatin anhydride microspheres via amide bonds. The nanoparticle-microsphere complex, exhibiting excellent cell-like functions, effectively bound to proinflammatory cytokines and enhanced the release of transforming growth factor-β1. The nanoparticle-microsphere complex significantly inhibited lipopolysaccharide-induced inflammation in nucleus pulposus cells in vitro.[38]
Protein-Rich Plasma
Platelet-rich plasma in the lumbar spine has a low incidence of adverse events compared to similar spinal injection techniques, with well-documented safety profiles. A systematic review on the use of platelet-rich plasma in lower back pain found the level of supporting evidence to be level II. However, this study did not specifically address disk herniation in isolation.[39]
T-box Transcription Factor T Antagonism
One study investigated the role of T-box transcription factor T (Tbxt) in disk degeneration. Knockdown of Tbxt exacerbates H2O2-induced senescence and apoptosis in nucleus pulposus cells, whereas upregulation of Tbxt significantly protects against intervertebral disk diseases in both in vivo and in vitro settings. Mechanistically, Tbxt enhances the transcription of ATG7 in the NP. This upregulation of ATG7 promotes autophagy, ultimately improving intervertebral disk disease. However, the precise mechanism underlying this senescence and apoptosis remains unclear, and further studies are warranted to clarify this understanding.[40]
Toxicity and Adverse Effect Management
The toxicity and adverse effects of HNP management vary significantly depending on the procedure or intervention. Possible interventions include physical therapy, osteopathic manipulation, trigger point injections, subarachnoid pain pumps, and surgery, each carrying its own risk profile. Few adverse effects occur with basic lumbar exercises and physical therapy. However, many patients have concomitant medical conditions, such as neuropathy, and are at high risk of falls. The risk can be mitigated by an astute therapist using a gait belt to assist the patient with ambulation.
Furthermore, patients require appropriate education and training on using adaptive equipment, such as standard and fold-down seat walkers, to ensure safety. Other issues can occur during therapy, such as cardiac events or pulmonary embolism, which are unlikely to be related to the treatment itself. Still, they can be precipitated by physical stress. Therefore, most physical therapists are certified in basic life support, and automated external defibrillators are nearly ubiquitous in medical settings.
Interventional procedures or oral corticosteroids can contribute to secondary hyperglycemia. Patients with type 1 diabetes may require sliding scale insulin coverage in addition to their basal insulin regimen; patients with type 2 diabetes usually do not require added insulin therapy if they remain adequately hydrated (hyperglycemia can cause polyuria and dehydration). In addition, edema of the peripheral extremities can occur using oral or injected corticosteroids. There is also a risk of infection associated with interventional procedures, and although rare, complications such as epidural abscess, meningitis, and soft tissue cellulitis can occur.[41][42] Muscle relaxants and opioids can be sedating and precipitate falls, especially in older adults. All patients receiving an opioid should also be prescribed naloxone and receive education on its proper use. Another designated individual should be aware of the location and indications of naloxone. Furthermore, polypharmacy is common in chronic pain management. Clinical trials have not evaluated the safety or efficacy of more than 2 concurrent medications.
Other potential adverse effects can occur during the ablation of the sinuvertebral nerves or intradiscal thermal radiofrequency ablation of the posterior annulus. Although unlikely, significant vascular or neurologic injury can occur. Additionally, interventional procedures in patients with cardiac pacemakers are generally safe. However, the pacemaker may misinterpret the radiofrequency signal as a nonperfusing, shockable rhythm. To prevent the shock, the defibrillation mode can be disabled during the radiofrequency procedure. If a nonperfusing rhythm occurs, the clinician should stop the radiofrequency ablation and commence resuscitation. Clinicians performing interlaminar injections should be familiar with the management of inadvertent spinal block and capable of placing or referring for epidural blood patches. Interventional procedures such as epidural steroid injections, radiofrequency ablations, and spinal cord stimulator placements should be performed in settings equipped to manage emergencies, including access to lipid rescue protocols for bupivacaine or other high-risk local anesthetics. Bupivacaine is avoided in most spinal and disk procedures because of its toxicity and risk, and lidocaine is used more frequently. Please refer to StatPearls' companion resource, "Lipid Emulsion Therapy," for additional information on this local anesthetic systemic toxicity treatment.
The likelihood of adverse effects depends on the medication(s) and the patient's comorbid conditions. Nonsteroidal anti-inflammatory drugs are generally safe, but can cause renal failure. Muscle relaxants and opioids can increase the risk of falls and sedation. Opioids can also cause respiratory depression, and naloxone should be available for prevention. Membrane stabilizers and benzodiazepines should not be stopped abruptly to avoid withdrawal, and they carry risks of sedation and potential falls. Several of these medications can be addictive, and patients can develop tolerance over time. Before initiating treatment with opioid medications, patients should undergo careful screening for substance use and mental health disorders. Self-medication is an additional concern, as patients may supplement prescribed treatments with alcohol, other medications, or illicit substances.
Prognosis
The prognosis of herniated disks is variable, but most cases respond to conservative management. Approximately 30% of patients continue to have back pain after one year.[43] Many herniated disks are asymptomatic and are detected incidentally on advanced imaging studies. Of symptomatic cases, 90% resolve after 6 weeks of conservative management. Surgery may lead to a more rapid recovery of the symptomatic herniated disk, but results are similar to conservative management after 1 year.[44][45]
Complications
Herniated disks can lead to chronic back pain. Furthermore, untreated herniation may result in prolonged nerve damage when severe nerve root compression is present. Most surgical repairs and diskectomies are successful, but some cases require repeat intervention. Economically, symptomatic herniated disks can lead to significant lost productivity and disability. Severe complications of surgery or interventional procedures are paralysis and death, although rare.
Postoperative and Rehabilitation Care
Discharge and postoperative instructions vary depending on the procedure and the clinicians' preferences. Surgeons use different protocols depending on whether they perform a laminectomy, fusion, or a diskectomy. Postoperative wound care is usually accomplished with an occlusive Aquacel or Silvercel dressing similar to that used in total knee arthroplasty. Sutures or staples are commonly removed after 14 days, unless dissolvable sutures are placed. Postoperative pain management is usually accomplished with short courses of outpatient oral medication. A bowel program to avoid constipation should be implemented, particularly after a laminectomy due to the increased risk of dural tear during Valsalva maneuvers. Furthermore, general anesthesia also contributes to constipation. Postoperative antibiotic protocols vary among surgeons. Patients should be instructed to apply ice to the surgical site, monitor their blood glucose levels, and contact their clinician if they develop a headache or fever. General rehabilitative care is a lifelong program of isometric exercises and abdominal core strengthening, even when axial spine pain is absent.
Following the placement of a temporary or permanent spinal cord stimulator, patients are typically advised to avoid overhead reaching for 6 weeks. Sutures or staples are usually removed after 14 days, with wound care tailored to the specific procedure, the patient's health status (eg, diabetes and immunosuppression), and the surgeon's discretion. Consensus is lacking regarding the use of prophylactic antibiotics for implantable devices; however, a 5-day course of a second-generation cephalosporin is commonly prescribed. Incisional pain tends to be more significant following pain pump insertion than after spinal cord stimulator placement, although procedures involving paddle lead stimulators with microlaminectomy may produce similar pain levels. Short-term opioid therapy (3–7 days) is often recommended for postoperative pain, particularly in cases with paddle leads.
Postoperative infections can occur with any procedure; however, spinal cord stimulators penetrate the epidural space, potentially causing epidural abscesses. While epidural abscesses are serious, meningitis presents an even greater risk. Because pain pumps are placed in the subarachnoid space, clinicians should monitor for signs of meningitis and have a low threshold for performing a lumbar puncture and consulting infectious disease specialists. Temporary and permanent pain pump insertions typically require an overnight hospital stay. However, some clinicians may use a single short-acting opioid spinal injection to assess pain response, allowing discharge after 6 to 8 hours. While this approach is more straightforward and cost-effective, it does not provide the advantage of evaluating how the device affects daily functioning and quality of life over an extended period. Postimplant spinal headaches may occur due to accidental dural puncture during spinal cord stimulator placement or intentional subarachnoid catheter placement. A blood patch is often an effective treatment option for this complication. Although no formal guidelines exist, early intervention, such as placing a temporary patch the following day, may help. For permanent pain pump implants, placement of a purse-string suture around the catheter may reduce the risk of postprocedural headaches.
Consultations
Disk herniation management may require either conservative treatment or a multidisciplinary approach. Different healthcare professionals may be involved, and the extent of their participation may be tailored to the patient’s specific needs, neurologic status, comorbidities, and treatment goals.
- Primary care clinicians are often the first to evaluate patients, perform comprehensive history and physical examinations, identify potential red flag signs, order necessary imaging tests, and prescribe appropriate therapies.
- Physical and occupational therapy are typically the first course of action in the absence of red flag signs. These therapists provide therapeutic exercise and training in the use of adaptive equipment. Physical therapists may also conduct trials with transcutaneous electrical nerve stimulation units and educate patients on their use.
- Interventional pain management clinicians can perform regional nerve blocks or procedural interventions, and insert spinal cord stimulators or intrathecal pumps.
- Psychiatry and psychology clinicians can address depression, anxiety, and adjustment disorders. Consultation may be indicated in cases progressing towards chronic pain syndrome. Please see StatPearls' companion reference, "Chronic Pain," for more information.
- Animal therapy has shown wide-ranging benefits across multiple areas of care. Hypoallergenic, nonshedding dogs are commonly used to provide comfort, ease anxiety, and serve as a source of distraction during procedures. These therapy animals can also enhance patient experiences by reducing perceived wait times in clinical settings.
- Pastoral care professionals support the spiritual needs of patients and their families. This service may overlap with psychiatric care and is usually tailored to reflect the patient’s religious beliefs and preferences.
- Prosthetics and orthotic clinicians provide braces and adaptive equipment to improve mobility and function.
- Orthopedic surgery clinicians can evaluate for other joint pathologies, such as those involving the hip or sacroiliac joint. They may also perform permanent stimulator implantations.
- Physical medicine and rehabilitation clinicians perform initial evaluations and coordinate care. They typically perform most interventional pain management procedures. Clinicians in this field may also manage prosthetic and brace assessments.
- Neurosurgery clinicians perform spinal surgeries and assist with implantable technologies.
- Addiction medicine clinicians should be consulted anytime a patient is placed on a controlled substance.
- The manufacturer's technical representative plays a crucial role in device programming, particularly during the first 12 weeks after implantation, as the leads settle and scar tissue forms. Seasonal changes, new injuries, and central sensitization often require reprogramming.
Deterrence and Patient Education
Patients should be educated to monitor for painless weakness, loss of bowel and bladder control, and involuntary movements, which may be signs of myelopathy. Patients also need education about the systemic signs of fever, chills, and night sweats. Patients also require instruction on the following points:
- Patients may experience burning pain, numbness, tingling, changes in sensation, or weakness.
- Most cases resolve with conservative management; however, a long-term program for core strengthening may be indicated to prevent further pain episodes.
- Patients with cervical and lumbar spine herniations are initially treated conservatively with over-the-counter pain medications, home exercises, heat, ice, and activity as tolerated.
- The recovery time depends on the injury mechanism and the severity of the disk herniation. On average, most cases of disk herniation resolve within 1 to 12 weeks after the injury.
- Because most cases start to improve 2 to 3 weeks after onset, physical therapy is not recommended until 3 weeks after the onset of symptoms.
- An MRI is not recommended unless symptoms persist for at least 6 weeks, severe radiculopathy develops, or neurologic deficits rapidly worsen.
- Progressive symptoms that do not improve with conservative treatment may require interventional pain management procedures.
Pearls and Other Issues
Pearls and other important information on disk herniation include the following:
- Clinicians should screen for red flag signs encompassing history and physical examination findings.
- Low back pain is a nearly universal human experience that affects almost all individuals during their lifetime.
- Disk herniations occur more often at the L4 to L5 and L5 to S1 intervertebral spaces. However, lumbar disk herniation tends to be more cranially located with increasing age. Any disk herniation can affect levels distal to it.
- Not all disk herniations are symptomatic, and not all low back pain results from a disk herniation.
- The differential diagnosis includes visceral, autoimmune, vascular, and infectious etiologies.
- Patients should be educated on home exercises, such as isometric abdominal strengthening, strategies to avoid lumbar hyperextension, maintaining a healthy weight and proper nutrition, preserving bone density, smoking cessation, and adopting healthy lifestyle practices.
Enhancing Healthcare Team Outcomes
Disk herniation is a common problem clinicians encounter in primary, emergency, urgent care, or internal medicine. Managing disk herniation is commonly suboptimal; therefore, an interprofessional team approach is recommended. Initial treatment should be conservative unless a patient has severe neurological compromise. The patient's pain is often managed with acetaminophen or nonsteroidal anti-inflammatory drugs, a home exercise program, and time. However, some cases require opioids, muscle relaxants, or membrane-stabilizing analgesics. Clear communication is essential, and no aspect of disk herniation care functions independently. Therapeutic interventions often involve collaboration among different members of the interprofessional team.
The physical therapist may need to contact the surgeon or prescribing clinician if the patient cannot tolerate specific therapy components. Secondary musculoskeletal issues, such as trochanteric bursitis, spinal enthesitis, or Baastrup disease, may emerge and interfere with progress. Additional modalities, such as therapeutic ultrasound, heat or cold application, or iontophoresis, may be necessary to support a comprehensive treatment plan and improve therapy tolerance. Clinicians should consider reassessment after a brief therapy course to address these complicating factors. A separate prescription is required for corticosteroids, typically dexamethasone, for iontophoresis or phonophoresis, and must be requested by the physical therapist. Pharmacists often notice patterns and notify prescribers, such as in the case of polysourcing, which is usually prevented through online monitoring systems. These systems allow clinicians to monitor prescriptions for controlled and selected noncontrolled substances. Surgery is usually a last resort, but may be a first-line treatment, such as in foot drop, cauda equina syndrome, or myelopathy. Surgical outcomes vary, and patients may have residual pain or neurologic deficits. An MRI of the affected spinal segment should be obtained if weakness or refractory axial spine pain is present or red flag signs are identified.
Furthermore, cases unresponsive to conservative management may require either the expertise of a pain medicine specialist in stable cases or a neurosurgeon in unstable instances. Back pain can be a significant cause of morbidity and is often associated with mental health conditions. Chronic back pain is also associated with depression and should be managed accordingly by the primary care or mental health clinician. The outcomes depend on many factors; however, individuals who exercise regularly and maintain a healthy body weight tend to achieve better results than those who remain sedentary.[1][7][46][47]
If the disk herniation results in post-laminectomy syndrome, chronic pain syndrome, or nonoperative status, a team approach similar to other chronic pain syndromes is indicated. Pain pumps require "interrogation" with a handheld device used for programming and reprogramming.[48] Patients in rural areas may be several hours away from their pain management specialist. In such cases, a local clinician can assist with adjustments to the pump. A manufacturer's technical representative can perform programming based on the pain specialist's orders. In contrast, the technical representative can typically perform spinal stimulator programming independently.[49] All pumps have an alarm usually set for 2 mL remaining, and any interdisciplinary team member should immediately bring this to the attention of the managing clinician.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
References
Sharma SB, Kim JS. A Review of Minimally Invasive Surgical Techniques for the Management of Thoracic Disc Herniations. Neurospine. 2019 Mar:16(1):24-33. doi: 10.14245/ns.1938014.007. Epub 2019 Mar 31 [PubMed PMID: 30943704]
Huang R, Meng Z, Cao Y, Yu J, Wang S, Luo C, Yu L, Xu Y, Sun Y, Jiang L. Nonsurgical medical treatment in the management of pain due to lumbar disc prolapse: A network meta-analysis. Seminars in arthritis and rheumatism. 2019 Oct:49(2):303-313. doi: 10.1016/j.semarthrit.2019.02.012. Epub 2019 Mar 4 [PubMed PMID: 30940466]
Level 1 (high-level) evidenceTang C, Moser FG, Reveille J, Bruckel J, Weisman MH. Cauda Equina Syndrome in Ankylosing Spondylitis: Challenges in Diagnosis, Management, and Pathogenesis. The Journal of rheumatology. 2019 Dec:46(12):1582-1588. doi: 10.3899/jrheum.181259. Epub 2019 Apr 1 [PubMed PMID: 30936280]
Hincapié CA, Kroismayr D, Hofstetter L, Kurmann A, Cancelliere C, Raja Rampersaud Y, Boyle E, Tomlinson GA, Jadad AR, Hartvigsen J, Côté P, Cassidy JD. Incidence of and risk factors for lumbar disc herniation with radiculopathy in adults: a systematic review. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2025 Jan:34(1):263-294. doi: 10.1007/s00586-024-08528-8. Epub 2024 Oct 25 [PubMed PMID: 39453541]
Level 1 (high-level) evidencePark CH, Park ES, Lee SH, Lee KK, Kwon YK, Kang MS, Lee SY, Shin YH. Risk Factors for Early Recurrence After Transforaminal Endoscopic Lumbar Disc Decompression. Pain physician. 2019 Mar:22(2):E133-E138 [PubMed PMID: 30921991]
Huang JS, Fan BK, Liu JM. [Overview of risk factors for failed percutaneous transforaminal endoscopic discectomy in lumbar disc herniation]. Zhongguo gu shang = China journal of orthopaedics and traumatology. 2019 Feb 25:32(2):186-189. doi: 10.3969/j.issn.1003-0034.2019.02.019. Epub [PubMed PMID: 30884940]
Level 3 (low-level) evidenceFjeld OR, Grøvle L, Helgeland J, Småstuen MC, Solberg TK, Zwart JA, Grotle M. Complications, reoperations, readmissions, and length of hospital stay in 34 639 surgical cases of lumbar disc herniation. The bone & joint journal. 2019 Apr:101-B(4):470-477. doi: 10.1302/0301-620X.101B4.BJJ-2018-1184.R1. Epub [PubMed PMID: 30929479]
Level 3 (low-level) evidenceJordan J, Konstantinou K, O'Dowd J. Herniated lumbar disc. BMJ clinical evidence. 2009 Mar 26:2009():. pii: 1118. Epub 2009 Mar 26 [PubMed PMID: 19445754]
Level 1 (high-level) evidenceCummins J, Lurie JD, Tosteson TD, Hanscom B, Abdu WA, Birkmeyer NJ, Herkowitz H, Weinstein J. Descriptive epidemiology and prior healthcare utilization of patients in the Spine Patient Outcomes Research Trial's (SPORT) three observational cohorts: disc herniation, spinal stenosis, and degenerative spondylolisthesis. Spine. 2006 Apr 1:31(7):806-14 [PubMed PMID: 16582855]
Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine. 1995 Sep 1:20(17):1878-83 [PubMed PMID: 8560335]
Level 2 (mid-level) evidenceZhu W, Yang Z, Zhou S, Zhang J, Xu Z, Xiong W, Liu P. Modic changes: From potential molecular mechanisms to future research directions (Review). Molecular medicine reports. 2025 Apr:31(4):. pii: 90. doi: 10.3892/mmr.2025.13455. Epub 2025 Feb 7 [PubMed PMID: 39918002]
Roberts S, Evans H, Menage J, Urban JP, Bayliss MT, Eisenstein SM, Rugg MS, Milner CM, Griffin S, Day AJ. TNFalpha-stimulated gene product (TSG-6) and its binding protein, IalphaI, in the human intervertebral disc: new molecules for the disc. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2005 Feb:14(1):36-42 [PubMed PMID: 15549486]
Andrade P, Visser-Vandewalle V, Philippens M, Daemen MA, Steinbusch HWM, Buurman WA, Hoogland G. Tumor necrosis factor-α levels correlate with postoperative pain severity in lumbar disc hernia patients: opposite clinical effects between tumor necrosis factor receptor 1 and 2. Pain. 2011 Nov:152(11):2645-2652. doi: 10.1016/j.pain.2011.08.012. Epub 2011 Sep 14 [PubMed PMID: 21920667]
Igarashi T, Kikuchi S, Shubayev V, Myers RR. 2000 Volvo Award winner in basic science studies: Exogenous tumor necrosis factor-alpha mimics nucleus pulposus-induced neuropathology. Molecular, histologic, and behavioral comparisons in rats. Spine. 2000 Dec 1:25(23):2975-80 [PubMed PMID: 11145807]
Olmarker K, Rydevik B. Selective inhibition of tumor necrosis factor-alpha prevents nucleus pulposus-induced thrombus formation, intraneural edema, and reduction of nerve conduction velocity: possible implications for future pharmacologic treatment strategies of sciatica. Spine. 2001 Apr 15:26(8):863-9 [PubMed PMID: 11317106]
Urban JP, Roberts S. Degeneration of the intervertebral disc. Arthritis research & therapy. 2003:5(3):120-30 [PubMed PMID: 12723977]
Level 3 (low-level) evidenceFu J, Yu W, Jiang D. Acidic pH promotes nucleus pulposus cell senescence through activating the p38 MAPK pathway. Bioscience reports. 2018 Dec 21:38(6):. pii: BSR20181451. doi: 10.1042/BSR20181451. Epub 2018 Nov 13 [PubMed PMID: 30291218]
Crump KB, Alminnawi A, Bermudez-Lekerika P, Compte R, Gualdi F, McSweeney T, Muñoz-Moya E, Nüesch A, Geris L, Dudli S, Karppinen J, Noailly J, Le Maitre C, Gantenbein B. Cartilaginous endplates: A comprehensive review on a neglected structure in intervertebral disc research. JOR spine. 2023 Dec:6(4):e1294. doi: 10.1002/jsp2.1294. Epub 2023 Oct 21 [PubMed PMID: 38156054]
Kawaguchi K, Saiwai H, Kobayakawa K, Tarukado K, Yokota K, Matsumoto Y, Harimaya K, Kato G, Nakashima Y. Association Between Histological Composition and Clinical Symptoms in Lumbar Disk Herniation in Different Age Groups. Spine. 2025 Aug 15:50(16):1153-1160. doi: 10.1097/BRS.0000000000005178. Epub 2024 Oct 8 [PubMed PMID: 39451128]
Rajesh N, Moudgil-Joshi J, Kaliaperumal C. Smoking and degenerative spinal disease: A systematic review. Brain & spine. 2022:2():100916. doi: 10.1016/j.bas.2022.100916. Epub 2022 Aug 7 [PubMed PMID: 36248118]
Level 1 (high-level) evidenceMaharty DC, Hines SC, Brown RB. Chronic Low Back Pain in Adults: Evaluation and Management. American family physician. 2024 Mar:109(3):233-244 [PubMed PMID: 38574213]
Das JM, Dua A, Nadi M. Straight Leg Raise Test (Lasegue sign). StatPearls. 2025 Jan:(): [PubMed PMID: 31424883]
Kaito T, Yamato Y. The Essence of Clinical Practice Guidelines for Lumbar Disc Herniation, 2021: 3. Diagnosis. Spine surgery and related research. 2022:6(4):325-328. doi: 10.22603/ssrr.2022-0044. Epub 2022 Jul 27 [PubMed PMID: 36051681]
Level 1 (high-level) evidenceChu EC, Yau KH, Bellin DL. An L2/3 Disc Herniation-Related L5 Radiculopathy. Current health sciences journal. 2023 Jan-Mar:49(1):129-133. doi: 10.12865/CHSJ.49.01.129. Epub 2023 Mar 31 [PubMed PMID: 37780195]
Carlson BB, Albert TJ. Lumbar disc herniation: what has the Spine Patient Outcomes Research Trial taught us? International orthopaedics. 2019 Apr:43(4):853-859. doi: 10.1007/s00264-019-04309-x. Epub 2019 Feb 15 [PubMed PMID: 30767043]
Hassan KZ, Sherman AL. Epidural Steroids. StatPearls. 2025 Jan:(): [PubMed PMID: 30726005]
Johnson SM, Shah LM. Imaging of Acute Low Back Pain. Radiologic clinics of North America. 2019 Mar:57(2):397-413. doi: 10.1016/j.rcl.2018.10.001. Epub 2018 Dec 5 [PubMed PMID: 30709477]
Brazilian Medical Association, Silvinato A, Simões RS, Buzzini RF, Bernardo WM. Lumbar herniated disc treatment with percutaneous hydrodiscectomy. Revista da Associacao Medica Brasileira (1992). 2018 Sep:64(9):778-782. doi: 10.1590/1806-9282.64.09.778. Epub [PubMed PMID: 30672996]
Harper R, Klineberg E. The evidence-based approach for surgical complications in the treatment of lumbar disc herniation. International orthopaedics. 2019 Apr:43(4):975-980. doi: 10.1007/s00264-018-4255-6. Epub 2018 Dec 12 [PubMed PMID: 30543041]
Lavi ES, Pal A, Bleicher D, Kang K, Sidani C. MR Imaging of the Spine: Urgent and Emergent Indications. Seminars in ultrasound, CT, and MR. 2018 Dec:39(6):551-569. doi: 10.1053/j.sult.2018.10.006. Epub 2018 Oct 19 [PubMed PMID: 30527521]
Alvin MD, Lubelski D, Alam R, Williams SK, Obuchowski NA, Steinmetz MP, Wang JC, Melillo AJ, Pahwa A, Benzel EC, Modic MT, Quencer R, Mroz TE. Spine Surgeon Treatment Variability: The Impact on Costs. Global spine journal. 2018 Aug:8(5):498-506. doi: 10.1177/2192568217739610. Epub 2017 Dec 15 [PubMed PMID: 30258756]
Qaseem A, Wilt TJ, McLean RM, Forciea MA, Clinical Guidelines Committee of the American College of Physicians, Denberg TD, Barry MJ, Boyd C, Chow RD, Fitterman N, Harris RP, Humphrey LL, Vijan S. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of internal medicine. 2017 Apr 4:166(7):514-530. doi: 10.7326/M16-2367. Epub 2017 Feb 14 [PubMed PMID: 28192789]
Level 1 (high-level) evidenceLandau WM, Nelson DA, Armon C, Argoff CE, Samuels J, Backonja MM. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2007 Aug 7:69(6):614; author reply 614-5 [PubMed PMID: 17679685]
Level 3 (low-level) evidenceChou R, Hashimoto R, Friedly J, Fu R, Bougatsos C, Dana T, Sullivan SD, Jarvik J. Epidural Corticosteroid Injections for Radiculopathy and Spinal Stenosis: A Systematic Review and Meta-analysis. Annals of internal medicine. 2015 Sep 1:163(5):373-81. doi: 10.7326/M15-0934. Epub [PubMed PMID: 26302454]
Level 1 (high-level) evidenceStretanski MF,Vu L, Fluoroscopy Discography Assessment, Protocols, and Interpretation. StatPearls. 2025 Jan; [PubMed PMID: 34283485]
Antohe BA, Rață M, Rață B, Rață G. Efficiency of physical therapy and osteopathic techniques in the treatment of operated and recurrent lumbar disc herniation - A case report. Journal of bodywork and movement therapies. 2025 Jun:42():243-248. doi: 10.1016/j.jbmt.2024.12.009. Epub 2024 Dec 15 [PubMed PMID: 40325676]
Level 3 (low-level) evidenceChou R, Loeser JD, Owens DK, Rosenquist RW, Atlas SJ, Baisden J, Carragee EJ, Grabois M, Murphy DR, Resnick DK, Stanos SP, Shaffer WO, Wall EM, American Pain Society Low Back Pain Guideline Panel. Interventional therapies, surgery, and interdisciplinary rehabilitation for low back pain: an evidence-based clinical practice guideline from the American Pain Society. Spine. 2009 May 1:34(10):1066-77. doi: 10.1097/BRS.0b013e3181a1390d. Epub [PubMed PMID: 19363457]
Level 1 (high-level) evidenceZhou L, Cai F, Zhu H, Xu Y, Tang J, Wang W, Li Z, Wu J, Ding Z, Xi K, Chen L, Gu Y. Immune-defensive microspheres promote regeneration of the nucleus pulposus by targeted entrapment of the inflammatory cascade during intervertebral disc degeneration. Bioactive materials. 2024 Jul:37():132-152. doi: 10.1016/j.bioactmat.2024.03.020. Epub 2024 Mar 20 [PubMed PMID: 38549774]
Machado ES, Soares FP, Vianna de Abreu E, de Souza TADC, Meves R, Grohs H, Ambach MA, Navani A, de Castro RB, Pozza DH, Caldas JMP. Systematic Review of Platelet-Rich Plasma for Low Back Pain. Biomedicines. 2023 Aug 28:11(9):. doi: 10.3390/biomedicines11092404. Epub 2023 Aug 28 [PubMed PMID: 37760845]
Level 1 (high-level) evidenceYue C, Wu Y, Xia Y, Xin T, Gong Y, Tao L, Shen C, Zhu Y, Shen M, Wang D, Shen J. Tbxt alleviates senescence and apoptosis of nucleus pulposus cells through Atg7-mediated autophagy activation during intervertebral disk degeneration. American journal of physiology. Cell physiology. 2024 Aug 1:327(2):C237-C253. doi: 10.1152/ajpcell.00126.2024. Epub 2024 Jun 10 [PubMed PMID: 38853649]
Tseng YC, Yang YS, Wu YC, Chiu SK, Lin TY, Yeh KM. Infectious sacroiliitis caused by Staphylococcus aureus following acupuncture: a case report. Acupuncture in medicine : journal of the British Medical Acupuncture Society. 2014 Feb:32(1):77-80. doi: 10.1136/acupmed-2013-010457. Epub 2013 Oct 17 [PubMed PMID: 24135310]
Level 3 (low-level) evidenceMatic S, Teodosic V, Zagorac S. Mycobacterium chelonae hand infection following acupuncture: a case report and literature review. Frontiers in medicine. 2024:11():1482236. doi: 10.3389/fmed.2024.1482236. Epub 2024 Nov 21 [PubMed PMID: 39640982]
Level 3 (low-level) evidenceAmlie E, Weber H, Holme I. Treatment of acute low-back pain with piroxicam: results of a double-blind placebo-controlled trial. Spine. 1987 Jun:12(5):473-6 [PubMed PMID: 2957801]
Level 1 (high-level) evidenceSchoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. International journal of general medicine. 2010 Jul 21:3():209-14 [PubMed PMID: 20689695]
Buttermann GR. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy. A prospective, randomized study. The Journal of bone and joint surgery. American volume. 2004 Apr:86(4):670-9 [PubMed PMID: 15069129]
Level 1 (high-level) evidenceHeo DH, Sharma S, Park CK. Endoscopic Treatment of Extraforaminal Entrapment of L5 Nerve Root (Far Out Syndrome) by Unilateral Biportal Endoscopic Approach: Technical Report and Preliminary Clinical Results. Neurospine. 2019 Mar:16(1):130-137. doi: 10.14245/ns.1938026.013. Epub 2019 Mar 31 [PubMed PMID: 30943715]
Shen Z, Zhong ZM, Wu Q, Zheng S, Shen X, Chen J. Predictors for Poor Outcomes After Percutaneous Endoscopic Lumbar Discectomy: A Retrospective Study of 241 Patients. World neurosurgery. 2019 Jun:126():e422-e431. doi: 10.1016/j.wneu.2019.02.068. Epub 2019 Feb 28 [PubMed PMID: 30825632]
Level 2 (mid-level) evidenceMahawar B, Kannan A, Mahawar V, Srinivasan S. Intrathecal pain pumps in pain relief. Clinical radiology. 2023 Apr:78(4):240-244. doi: 10.1016/j.crad.2023.02.002. Epub 2023 Feb 16 [PubMed PMID: 36841671]
Silva H, Barbosa P, Fernandes V, Pereira L, Gomes A. Severe Case of Intrathecal Baclofen Withdrawal: A Case Report. Cureus. 2025 Mar:17(3):e81141. doi: 10.7759/cureus.81141. Epub 2025 Mar 25 [PubMed PMID: 40276449]
Level 3 (low-level) evidence