Definition/Introduction
Decorticate posturing indicates a patterned motor response observed in neurological and neurosurgical patients with intracranial hypertension and descending transtentorial brainstem herniation syndrome. Flexor posturing with internal rotation of the upper limbs occurs alongside extensor posturing of the lower limbs. Painful stimulation should be applied to cranial nerve dermatomes like the supraorbital ridge to avoid confounding spinal reflexes.[1][2] The rubrospinal tract mediates upper-limb flexion and contributes to lower-limb extension.[3][4] In contrast, the vestibulospinal tract drives extensor posturing in both upper and lower limbs (see Image. Decorticate Posturing).
Decorticate posturing, therefore, implies preserved rubrospinal tract function and suggests that the lesion has not extended below this level.[5] This response corresponds to a motor score of 3 on the Glasgow Coma Scale. Affected patients often exhibit reduced consciousness due to involvement of the reticular activating system in the brainstem.[6]
Genesis of Transtentorial Descending Brainstem Herniation
An increase in intracranial pressure (ICP) is initially buffered by compensatory displacement of cerebrospinal fluid (CSF) and modulation of cerebral blood volume, consistent with the Monro-Kellie doctrine. Once compensatory mechanisms are exhausted, brain tissue begins to herniate through anatomical foramina formed by the falx cerebri and tentorial incisura, initiating the cascade of cerebral herniation syndromes. Subfalcine and uncal herniation occur first, followed by transtentorial descending central brainstem herniation, and ultimately tonsillar herniation.[7]
Anatomical Localization and Pathogenesis Governing Decorticate Posturing
The red nucleus consists of a rostral parvocellular component (RNp) and a caudal magnocellular component (RNm). This structure lies at the intercollicular level. In humans, RNp forms the predominant portion, while RNm occupies only a limited region at the caudal pole of RNp.
RNp receives afferents from the dentate nucleus and sends efferents to the ipsilateral inferior olivary nucleus, forming the dentato-rubro-olivary pathway, also known as the triangle of Guillain-Mollaret. This circuit modulates complex cognitive-motor integration and behavioral refinement. The olivocerebellar pathway encodes and mediates motor learning based on error correction.
The RNm receives afferents from the contralateral deep interpositus nuclei of the cerebellum and gives rise to the rubrospinal tract, which decussates and descends into the spinal cord. This tract terminates in Rexed laminae V, VI, and VII, where it synapses with α- and γ-motor neurons that innervate flexor muscles of the upper limbs. The rubrospinal tract modulates grasping and stereotyped hand movements essential for crawling during infancy. RNm is phylogenetically older and reflects the evolutionary transition from aquatic to terrestrial locomotion. The function of this nucleus parallels the primitive pyramidal tract and facilitates stereotyped motor patterns.
In primates, progressive regression of RNm correlates with the shift from quadrupedal to bipedal locomotion. Despite this regression, RNm retains critical roles in human ontogenesis and motor recovery following pyramidal tract lesions.[8]
The rubrospinal tract preferentially facilitates flexion in the upper limbs. In contrast, the vestibulospinal tracts mediate extension in both upper and lower limbs. Cortical input normally inhibits both descending systems. Decorticate posturing arises from lesions rostral to the red nucleus, eliminating cortical modulation and producing unopposed rubrospinal-mediated upper-limb flexion. Decerebrate posturing occurs with lesions above the vestibular nuclei, removing inhibitory cortical influence and resulting in vestibulospinal-mediated extension of all limbs.[9]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
Etiology of Abnormal Decorticate Motor Posturing
Abnormal posturing serves as a critical clinical sign of significant central nervous system dysfunction. Accurate identification of the underlying cause is essential for timely intervention.
- Anoxic-hypoxic injury: Cardiac arrest, perinatal asphyxia, prolonged hypoxemia, status epilepticus
- Trauma: Moderate-to-severe traumatic brain injury (TBI)
- Vascular events: Acute ischemic stroke, intracerebral hemorrhage, subarachnoid hemorrhage
- Space-occupying lesions: Intracranial tumors, abscesses, hematomas
- Inflammatory conditions: Encephalitis, meningoencephalitis
- Altered CSF dynamics: Acute hydrocephalus, posthemorrhagic ventricular dilatation
- Metabolic disturbances: Dyselectrolytemia (especially hyponatremia or hypernatremia), hepatic encephalopathy, hypoglycemia
- Infectious diseases: Cerebral malaria, brainstem encephalitis, bacterial abscess
- Toxic and drug-related causes: Lead poisoning, methomyl poisoning, neuroleptic malignant syndrome, serotonin syndrome, drug withdrawal states, Reye syndrome
Recognition of the diverse etiologies aids in refining diagnostic pathways and anticipating the severity of underlying brain injury. Prompt treatment directed at the primary cause may reverse posturing and prevent further neurological deterioration.
Salient Radiological Features
Central descending herniation results in obliteration of the perimesencephalic and perimedullary cisterns, truncation of the brainstem, and the appearance of Duret hemorrhages on neuroimaging. These findings reflect severe downward displacement of brain structures and portend a grave prognosis.
Salient Hallmarks During Intracranial Pressure Monitoring
ICP monitoring may reveal a progressive rise in values. Abnormal waveforms include Lundberg A waves (plateau waves peaking at 50 mm Hg and lasting 5 to 20 minutes) and B waves (rhythmic oscillations occurring every 1 to 2 minutes, peaking at 20 to 30 mm Hg). The ICP waveform may also show an elevated dicrotic wave (P2) that exceeds the amplitude of the percussion wave (P1) and the tidal wave (P3), indicating impaired intracranial compliance.
Clinical Significance
Differential Diagnosis
The differential diagnosis for abnormal posturing includes several mimics with distinct clinical and neurophysiologic characteristics. Careful assessment is necessary to avoid misclassification and guide targeted evaluation.
Normal flexion responses lack lower-limb extension and often exhibit shoulder abduction and internal rotation, distinguishing them from true decorticate posturing. Decerebrate posturing consists of bilateral extensor responses and internal limb rotation, indicating preserved vestibulospinal tract integrity but often preceding tonsillar herniation, respiratory failure, and death.[10]
The Lazarus reflex features upper-limb flexion and adduction across the chest, resembling a mummified posture. This reflex is compatible with brainstem death and is differentiated by brainstem areflexia and a positive apnea test.[11][12] Opisthotonus, characterized by severe arching of the back and neck, typically occurs in cerebral palsy, tetanus, poisoning, or postdrowning states.
Paratonia, or gegenhalten, appears in patients with encephalopathy or neurodegenerative disorders. Spasticity involves increased muscle tone with preserved consciousness. Cerebellar fits produce opisthotonic and decerebrate-like posturing, often accompanied by drop attacks without altered awareness.[13] Paroxysmal autonomic instability with dystonia presents as episodic dystonia with hemihidrosis, tachycardia, tachypnea, and mydriasis.[14][15] Tonic status epilepticus may also mimic posturing patterns in unresponsive patients.[16]
Understanding the semiology of abnormal posturing is essential for accurate clinical localization and prognostication. Accurate interpretation of posturing patterns enhances diagnostic precision in comatose or critically ill patients.
Complications
Decorticate posturing often marks the initial stage in the clinical spectrum of descending transtentorial central herniation.[17] Without timely intervention, progression to decerebrate posturing may occur, followed by respiratory arrest due to tonsillar herniation. Patients may exhibit the classic components of the Cushing triad: hypertension, bradycardia, and irregular respiration. Respiratory patterns typically evolve from Cheyne-Stokes respiration to central neurogenic hyperventilation, then to ataxic breathing, and, ultimately, to apnea. This sequence culminates in fixed, dilated pupils and respiratory arrest resulting from medullary respiratory center compression.
Nursing, Allied Health, and Interprofessional Team Interventions
More than 80% of patients presenting with decorticate posturing and bilateral fixed, dilated pupils ultimately die. Reported mortality reaches up to 60% among patients with decorticate posturing and up to 90% in those with decerebrate posturing following a TBI. Financial constraints and caretaker burden, exacerbated by limited infrastructure and the absence of dedicated rehabilitation facilities, further compromise outcomes in low- and middle-income countries.
Multiple variables influence prognosis in patients with decorticate posturing. Time to hospital admission, subtype of the primary lesion, management approach (medical versus surgical), and patient age constitute the principal determinants..[18] Among traumatic lesions, acute extradural hematoma is associated with higher survival rates compared to acute subdural hematoma and intracerebral hemorrhage. Adults older than 60 tend to have lower recovery and survival rates compared to younger cohorts. Hypoxic brain injury and penetrating cranial trauma carry particularly poor prognoses.
Early recognition of decorticate posturing in neurological and neurosurgical patients allows for prompt initiation of corrective interventions. Timely administration of mannitol or hypertonic saline, placement of an external ventricular drain, or decompressive hemicraniectomy may halt and potentially reverse the progression of brain herniation. Preventing the transition from decorticate to decerebrate posturing reduces the risk of fatal tonsillar herniation. Management should follow a stepladder algorithm for intracranial hypertension, including the following:
- Rapid evacuation of sizeable mass lesions causing herniation (eg, hematoma, contusion, tumors)
- Physiological neuroprotection
- Sedation, analgesia, and mechanical ventilation
- CSF drainage via ventriculostomy
- Osmotherapy using diuretics, mannitol, or hypertonic saline
- Hyperventilation
- Therapeutic hypothermia
- Barbiturate coma
- Decompressive hemicraniectomy
The Brain Trauma Foundation recommends ICP monitoring in patients with severe TBI (Glasgow Coma Scale score of 3 to 8) who present with abnormalities on head CT or meet at least 2 of the following criteria:
- Age over 40 years
- Systolic blood pressure below 90 mm Hg
- Abnormal posturing
ICP changes may precede overt clinical signs of herniation by up to 6 hours, underscoring the importance of early monitoring in high-risk patients.
Nursing, Allied Health, and Interprofessional Team Monitoring
Aggressive goal-directed therapy combined with a patient-centered care bundle, delivered by an interprofessional team, remains pivotal in optimizing outcomes in this patient population. Such an approach facilitates timely decision-making, reduces complications, and supports continuity of care across treatment phases.
Media
(Click Image to Enlarge)
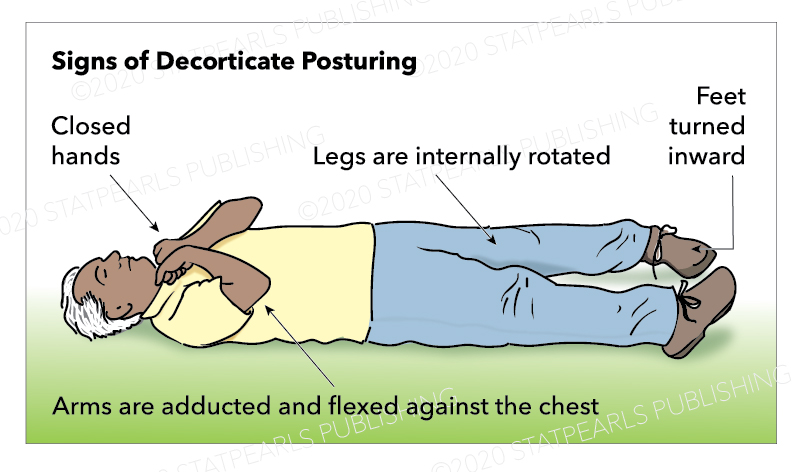
Decorticate Posturing. The image shows a man with flexed arms and clenched fists held across the chest, alongside extended and internally rotated lower limbs. This posture indicates a lesion above the red nucleus with preserved rubrospinal tract function mediating upper limb flexion and unopposed vestibulospinal tract activity causing lower limb extension.
Contributed by Katherine Humphreys
References
Clark A, Das JM, Mesfin FB. Trauma Neurological Exam. StatPearls. 2025 Jan:(): [PubMed PMID: 29939692]
de Sousa I, Woodward S. The Glasgow Coma Scale in adults: doing it right. Emergency nurse : the journal of the RCN Accident and Emergency Nursing Association. 2016 Dec 7:24(8):33-39 [PubMed PMID: 27923300]
McPherson JG, Chen A, Ellis MD, Yao J, Heckman CJ, Dewald JPA. Progressive recruitment of contralesional cortico-reticulospinal pathways drives motor impairment post stroke. The Journal of physiology. 2018 Apr 1:596(7):1211-1225. doi: 10.1113/JP274968. Epub 2018 Feb 19 [PubMed PMID: 29457651]
Riddle CN, Edgley SA, Baker SN. Direct and indirect connections with upper limb motoneurons from the primate reticulospinal tract. The Journal of neuroscience : the official journal of the Society for Neuroscience. 2009 Apr 15:29(15):4993-9. doi: 10.1523/JNEUROSCI.3720-08.2009. Epub [PubMed PMID: 19369568]
Level 3 (low-level) evidenceVadhan J, Das JM. Neuroanatomy, Red Nucleus. StatPearls. 2025 Jan:(): [PubMed PMID: 31869092]
Whitney E, Alastra AJ. Neuroanatomy, Decerebrate Rigidity. StatPearls. 2025 Jan:(): [PubMed PMID: 31613467]
Munakomi S, Das JM. Brain Herniation. StatPearls. 2025 Jan:(): [PubMed PMID: 31194403]
Basile GA, Quartu M, Bertino S, Serra MP, Boi M, Bramanti A, Anastasi GP, Milardi D, Cacciola A. Red nucleus structure and function: from anatomy to clinical neurosciences. Brain structure & function. 2021 Jan:226(1):69-91. doi: 10.1007/s00429-020-02171-x. Epub 2020 Nov 12 [PubMed PMID: 33180142]
Knight J, Decker LC. Decerebrate and Decorticate Posturing. StatPearls. 2025 Jan:(): [PubMed PMID: 32644561]
WARD AA Jr. Decerebrate rigidity. Journal of neurophysiology. 1947 Mar:10(2):89-103 [PubMed PMID: 20291835]
Hannawi Y, Abers MS, Geocadin RG, Mirski MA. Abnormal movements in critical care patients with brain injury: a diagnostic approach. Critical care (London, England). 2016 Mar 14:20():60. doi: 10.1186/s13054-016-1236-2. Epub 2016 Mar 14 [PubMed PMID: 26975183]
Moon JW, Hyun DK. Chronic Brain-Dead Patients Who Exhibit Lazarus Sign. Korean journal of neurotrauma. 2017 Oct:13(2):153-157. doi: 10.13004/kjnt.2017.13.2.153. Epub 2017 Oct 31 [PubMed PMID: 29201852]
Serino D, Caputo D, Fusco L. Cerebellar fits in the 2000s. Brain & development. 2018 Jan:40(1):77-80. doi: 10.1016/j.braindev.2017.06.011. Epub 2017 Jul 19 [PubMed PMID: 28734691]
Takahashi C, Hinson HE, Baguley IJ. Autonomic dysfunction syndromes after acute brain injury. Handbook of clinical neurology. 2015:128():539-51. doi: 10.1016/B978-0-444-63521-1.00034-0. Epub [PubMed PMID: 25701906]
Buerger KJ, Salazar R. Alternating hemidystonia following traumatic brain injury as an unusual presentation of paroxysmal autonomic instability with dystonia syndrome. BMJ case reports. 2014 Nov 20:2014():. doi: 10.1136/bcr-2014-206102. Epub 2014 Nov 20 [PubMed PMID: 25414239]
Level 3 (low-level) evidenceFernández-Torre JL, Riancho J, Martín-García M, Martínez-de Las Cuevas G, Bosque-Varela P. Tonic status epilepticus in a centenarian woman. Epileptic disorders : international epilepsy journal with videotape. 2019 Feb 1:21(1):92-96. doi: 10.1684/epd.2019.1031. Epub [PubMed PMID: 30816845]
Knight J, Rayi A. Transtentorial Herniation. StatPearls. 2025 Jan:(): [PubMed PMID: 32809371]
Wei Y, Cui Y, Pang X, Wang W. A systematic review and meta-analysis on abnormal posturing among brain injury patients. Arquivos de neuro-psiquiatria. 2024 Apr:82(4):1-10. doi: 10.1055/s-0044-1785689. Epub 2024 Apr 23 [PubMed PMID: 38653484]
Level 1 (high-level) evidence