Introduction
Hyperthermia is defined as a body temperature over 40 °C. Causes include sepsis, toxidromes, medication reactions, and environmental conditions. In sepsis, a dysregulated immunologic response produces fever. In toxidromes, withdrawal syndromes, and medication reactions, dysregulated metabolism generates endogenous heat. Heat-related illnesses arise when thermoregulatory mechanisms cannot adequately compensate for environmental and metabolic heat. Only heat-related illnesses resulting from environmental exposure respond directly to cooling interventions.
Heat-related illness encompasses a spectrum of conditions that arise when thermoregulatory mechanisms fail. Heat exhaustion is characterized by elevated core body temperature accompanied by orthostatic hypotension, tachycardia, diaphoresis, and tachypnea. Heat stroke is defined by elevated core body temperature with central nervous system involvement, potentially manifesting as delirium, decreased level of consciousness, or ataxia.
Heat-related illness most commonly affects athletes (exertional hyperthermia) but can also occur in hot environments or regions with extreme temperatures (classic hyperthermia). People with impaired thermoregulation or limited coping strategies, such as those at the extremes of age or individuals with comorbidities like obesity, psychiatric disorders, substance use disorders, metabolic disorders, or cardiac conditions, are at higher risk.[1] Most cases in the U.S. occur in patients aged 25 to 64 years.[2]
The rising burden of heat-related illness is exacerbated by climate change, as heat waves increase in frequency and intensity. The risk of morbidity and mortality is influenced by heat exposure, individual susceptibility, and population-level factors, including social determinants of health.[3]
The definitive treatment for heat-related illness is total body cooling. Conduction and evaporation are the 2 primary modes of heat removal. Ice-water immersion has been shown to be the most effective method. However, logistical and resource constraints often limit its use in the emergency department. This intervention may be provided during athletic events, particularly endurance competitions like marathons, where heat-related illnesses are common.
Evaporative cooling using mist and fans is the next most efficient method. Application of ice packs to the groin, axilla, neck, and other areas adjacent to major vessels is less effective. Cooled intravenous fluids have been studied, but evidence remains inconclusive regarding their benefit for neurologic preservation versus potential harm from induced shivering, although they may be considered in select cases.[4]
This activity will outline the procedure for evaporative cooling and describe adjunct methods applicable in the emergency department. Commercially available devices designed for cooling include invasive cooling catheters and noninvasive adhesive pads that circulate chilled water. These devices were originally developed for targeted hypothermia following cardiac arrest but may be applied to heat-related illnesses when available.
Limited literature directly compares these devices with traditional cooling methods. Antipyretics should not be used in heat-related illness, as they may exacerbate coagulopathy and contribute to organ dysfunction. Dantrolene has not been shown to improve recovery and is not indicated for heat-related illness. Benzodiazepines may serve as an adjunct, primarily to control shivering and agitation.
Early recognition and intervention are crucial in managing heat-related illness. Military and sports medicine literature identifies 39 °C as the treatment goal, and achieving this temperature more rapidly is associated with lower patient mortality.[5][6]
Indications
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Indications
Indications for cooling include any signs of heat-related illness in the presence of an elevated body temperature. Historically, heat-related illness has been defined as a core temperature exceeding 40 °C. However, any temperature above normal in a symptomatic patient without another identifiable cause warrants consideration of cooling interventions. The immediate objective is to reduce core temperature below 39 °C, with the ultimate goal of achieving the normal range of 36 °C to 38 °C. Assessment for severe heat stroke should include evaluation of hemodynamic stability to guide the urgency and intensity of rapid cooling.[7]
Contraindications
The only absolute contraindication to cooling is a normal or low body temperature. Hyperthermia may reflect sepsis, toxic ingestion, withdrawal, or another underlying etiology, and disease-specific treatment should not be overlooked. Clinicians should prioritize standard resuscitation measures, emergent management of airway, breathing, and circulation, and medical management guided by a broad differential diagnosis.
Equipment
Several cooling methods are available in the emergency department using standard equipment, including the following:
- Cooling blankets
- Cold intravenous saline
- Ice packs
- Cool water immersion or bath
- Foley catheter irrigation
- Sheets or towels
- Waterproof body bags
Additional equipment that may facilitate cooling includes a spray bottle and a fan.
Personnel
A single provider can perform all cooling techniques described in this activity. However, additional personnel facilitate more rapid cooling by enabling parallel interventions.
For example, the physician should assess the patient for the spectrum of heat-related illness, determine the need for external cooling, and evaluate for coexisting injuries or comorbidities. Departmental technicians can prepare and set up equipment, including temperature monitoring devices, vital sign monitors, ice, body bags, and other required supplies. Nursing staff can assist with patient positioning and continuous monitoring of vital signs, with particular attention to core temperature. Environmental or nutrition support personnel can facilitate the timely delivery of ice and other necessary supplies on a patient-by-patient basis.
Preparation
During preparation, the patient should be fully exposed, and intravenous access should be established. The team should assess for external signs of trauma. Continuous cardiac monitoring is recommended when available. Core body temperature should be closely monitored using an intracavitary thermometer, with esophageal, rectal, or bladder probes commonly employed.
Technique or Treatment
The cold-water immersion method cools the patient at an approximate rate of 0.13 °C per minute. The procedure begins by placing the patient in a waterproof body bag. Ice is added first, followed by water to create an ice slurry. The bag may then be secured up to the patient’s chest. The lower extremities may be submerged initially if the bag is too small to accommodate the entire body, with extremities exposed as needed to allow other medical interventions. The bag may be drained by cutting the inferior portion once the patient’s core temperature reaches the target of 39 °C, and the patient is positioned in reverse Trendelenburg.
Evaporative cooling reduces core temperature at an approximate rate of 0.05 °C per minute and involves continuous application of cold water to the skin using sponging or a spray bottle. A fan should be directed at the patient while spraying or sponging to enhance evaporation and accelerate cooling. Alternatively, a sheet may be submerged in ice water, wrung out, and wrapped around the patient. The sheet should be replaced and resubmerged when it loses its cooling effect.
Ice packs may also be applied to the groin, axillae, neck, and torso, which are most effective in lowering core temperature. Cold saline may be infused with caution to monitor for induced shivering. A Foley catheter may be used for bladder irrigation with cold saline. Frequent replacement of ice packs and repeated application of cold water facilitate more rapid cooling.[8][9]
These methods require continuous reapplication of water and ice to maintain efficacy (see Image. Cooling Techniques for Hyperthermia). Monitoring of core temperature is essential to guide ongoing reapplication and prevent overcooling.
Complications
Cooling is a critical intervention for heat-related illness and is associated with few complications. Vital signs must be monitored closely throughout the cooling process. Core body temperature and the presence of shivering should be continuously assessed, as shivering can impede effective cooling. Critically ill patients may further decompensate during intervention. Core temperatures below normal (36 °C) put patients at risk for hypothermia-related complications, including arrhythmias and coagulopathy. Skin integrity should also be monitored, as prolonged exposure to ice can cause tissue damage. Covering ice packs with a towel or sheet and regularly repositioning them mitigates this risk.[10][11][12][13]
Clinical Significance
Rapid reduction of core body temperature is the most critical intervention in managing heat-related illness and heat stroke. Cooling may also serve as an adjunct to standard therapies for conditions that cause secondary hyperthermia. The techniques described are straightforward, effective, and easily implemented in the emergency department. These approaches require minimal training and may be performed by a single provider. The methods are applicable across a variety of clinical environments. Timely identification of patients who will benefit from cooling is essential for effective management.[14]
Enhancing Healthcare Team Outcomes
Hyperthermia can present frequently in certain regions to the emergency department. Some patients may require systemic cooling to prevent neurological injury. Rapid reduction of core body temperature remains the most critical intervention in managing heat-related illness and heat stroke. Optimal cooling is achieved through an interprofessional approach involving neurologists, internists, emergency physicians, and critical care nurses.
Cooling may also serve as an adjunct to standard therapies for conditions causing secondary hyperthermia. Timely identification of patients who will benefit from cooling interventions is essential for effective management.
Media
(Click Image to Enlarge)
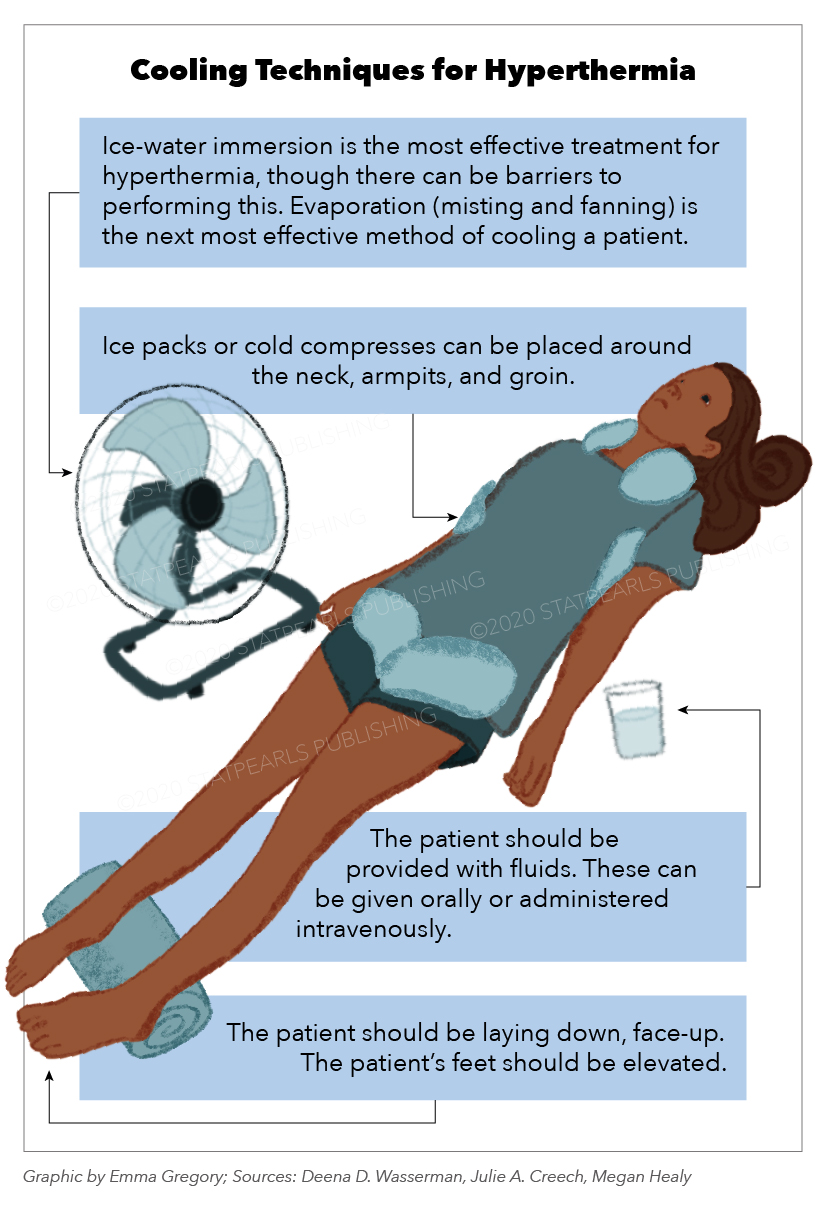
Cooling Techniques for Hyperthermia. This image outlines the recommended steps for treating hyperthermia. The patient is receiving several cooling interventions. The text highlights a hierarchy of effectiveness, with ice-water immersion being the most effective method, followed by evaporation through misting and fanning. The illustration also details the use of ice packs on specific body areas, oral or intravenous fluid administration, and proper patient positioning with elevated feet.
Graphic by E Gregory
References
Pryor RR, Haboian K, Fitts T, Stooks JJ. Tarp-Assisted Cooling for Exertional Heat Stroke Treatment in Wildland Firefighting. Wilderness & environmental medicine. 2023 Dec:34(4):490-497. doi: 10.1016/j.wem.2023.08.002. Epub 2023 Sep 23 [PubMed PMID: 37748988]
Yeargin S, Hirschhorn R, Grundstein A. Heat-Related Illnesses Transported by United States Emergency Medical Services. Medicina (Kaunas, Lithuania). 2020 Oct 17:56(10):. doi: 10.3390/medicina56100543. Epub 2020 Oct 17 [PubMed PMID: 33080867]
Sorensen C, Hess J. Treatment and Prevention of Heat-Related Illness. The New England journal of medicine. 2022 Oct 13:387(15):1404-1413. doi: 10.1056/NEJMcp2210623. Epub 2022 Sep 28 [PubMed PMID: 36170473]
McDermott BP, Atkins WC. Whole-body cooling effectiveness of cold intravenous saline following exercise hyperthermia: a randomized trial. The American journal of emergency medicine. 2023 Oct:72():188-192. doi: 10.1016/j.ajem.2023.07.053. Epub 2023 Aug 2 [PubMed PMID: 37562177]
Level 1 (high-level) evidenceNye EA, Edler JR, Eberman LE, Games KE. Optimizing Cold-Water Immersion for Exercise-Induced Hyperthermia: An Evidence-Based Paper. Journal of athletic training. 2016 Jun 2:51(6):500-1. doi: 10.4085/1062-6050-51.9.04. Epub 2016 Jul 21 [PubMed PMID: 27441949]
Comp G, Pugsley P, Sklar D, Akhter M, McElhinny M, Erickson E, Feinstein B, Enenbach M, Williams L, Pearlmutter J, Stowell JR. Heat Stroke Management Updates: A Description of the Development of a Novel In-Emergency Department Cold-Water Immersion Protocol and Guide for Implementation. Annals of emergency medicine. 2025 Jan:85(1):43-52. doi: 10.1016/j.annemergmed.2024.07.013. Epub 2024 Sep 24 [PubMed PMID: 39320280]
Butts CL, Spisla DL, Adams JD, Smith CR, Paulsen KM, Caldwell AR, Ganio MS, McDermott BP. Effectiveness of Ice-Sheet Cooling Following Exertional Hyperthermia. Military medicine. 2017 Sep:182(9):e1951-e1957. doi: 10.7205/MILMED-D-17-00057. Epub [PubMed PMID: 28885961]
O'Connor JP. Simple and effective method to lower body core temperatures of hyperthermic patients. The American journal of emergency medicine. 2017 Jun:35(6):881-884. doi: 10.1016/j.ajem.2017.01.053. Epub 2017 Jan 30 [PubMed PMID: 28162872]
Lissoway JB, Lipman GS, Grahn DA, Cao VH, Shaheen M, Phan S, Weiss EA, Heller HC. Novel application of chemical cold packs for treatment of exercise-induced hyperthermia: a randomized controlled trial. Wilderness & environmental medicine. 2015 Jun:26(2):173-9. doi: 10.1016/j.wem.2014.11.006. Epub 2015 Mar 12 [PubMed PMID: 25771030]
Level 1 (high-level) evidenceTan PM, Teo EY, Ali NB, Ang BC, Iskandar I, Law LY, Lee JK. Evaluation of Various Cooling Systems After Exercise-Induced Hyperthermia. Journal of athletic training. 2017 Feb:52(2):108-116. doi: 10.4085/1062-6050-52.1.11. Epub 2017 Feb 3 [PubMed PMID: 28156130]
Krishnan SS, Nigam P, Bachh O, Vasudevan MC. Quad Fever: Treatment through Lowering of Ambient Temperature. Indian journal of critical care medicine : peer-reviewed, official publication of Indian Society of Critical Care Medicine. 2018 Jan:22(1):43-45. doi: 10.4103/ijccm.IJCCM_295_17. Epub [PubMed PMID: 29422733]
Lovett ME, Moore-Clingenpeel M, Ayad O, O'Brien N. Reduction of hyperthermia in pediatric patients with severe traumatic brain injury: a quality improvement initiative. Journal of neurosurgery. Pediatrics. 2018 Feb:21(2):164-170. doi: 10.3171/2017.8.PEDS17104. Epub 2017 Dec 1 [PubMed PMID: 29192867]
Level 2 (mid-level) evidenceLiu G, Li ZG, Gao JS. Hypothermia in neonatal hypoxic-ischemic encephalopathy (HIE). European review for medical and pharmacological sciences. 2017 Oct:21(4 Suppl):50-53 [PubMed PMID: 29165765]
Bindu B, Bindra A, Rath G. Temperature management under general anesthesia: Compulsion or option. Journal of anaesthesiology, clinical pharmacology. 2017 Jul-Sep:33(3):306-316. doi: 10.4103/joacp.JOACP_334_16. Epub [PubMed PMID: 29109627]