Introduction
Vertebrae, along with intervertebral discs, form the vertebral column, or spine, extending from the base of the skull to the coccyx and includes the cervical, thoracic, lumbar, and sacral regions. The spine has several significant roles in the body, including protecting the spinal cord and branching spinal nerves, providing structural support, and allowing for the flexibility and mobility of the body. The intervertebral discs are cartilaginous structures between adjacent vertebrae that support the spine by acting as shock-absorbing cushions to the axial loading of the body.[1][2]
The cervical spine consists of 7 vertebral bodies, numbered C1 to C7, extending from the skull's base to the thoracic spine. The structure of C1, C2, and C7 has distinctive properties that make them unique in comparison to the typical cervical vertebrae, C3 to C6. The anatomy of C3 to C6 consists of a vertebral body, a vertebral arch, and 7 processes. The vertebral arch comprises the pedicles, bony processes that project posteriorly from the vertebral body, and the lamina, which form most of the bony arch. The pedicles and the lamina form a ring around the spinal canal, which harbors the spinal cord. Completing the typical vertebra are 7 processes, which include 2 superior articular facets, 2 inferior articular facets, 1 spinous process, and 2 transverse processes that allow the passage of the vertebral vasculature.
There are 3 atypical vertebrae in the cervical region. C1 (atlas) articulates with the base of the skull. C1 is unique in that it does not contain a body, due to the fusion of the embryological equivalent of the C1 vertebral body with the C2 (axis) vertebrae, which acts as a pivot point for the atlas to rotate. The most distinctive feature of the C2 vertebra is an odontoid process (dens), which arises from the superior aspect of its body and articulates with the posterior surface of C1's anterior arch. C7 is distinguished from other cervical vertebrae by 2 key features: its transverse foramina do not transmit vertebral vessels, and it has an especially long spinous process, which is why it is often called the “vertebra prominens."[3]
While there are 7 cervical vertebrae, there are 8 pairs of cervical nerves, numbered C1 to C8. Each pair of cervical nerves emerges from the spinal cord superior to their corresponding pedicle, except for C8, which exits inferiorly to the C7 pedicle.[4] Cervical disc herniation is the result of the displacement of the nucleus pulposus of the intervertebral disc, which may result in impingement of these traversing nerves as they exit the neural foramen or directly compressing the spinal cord contained within the spinal canal.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
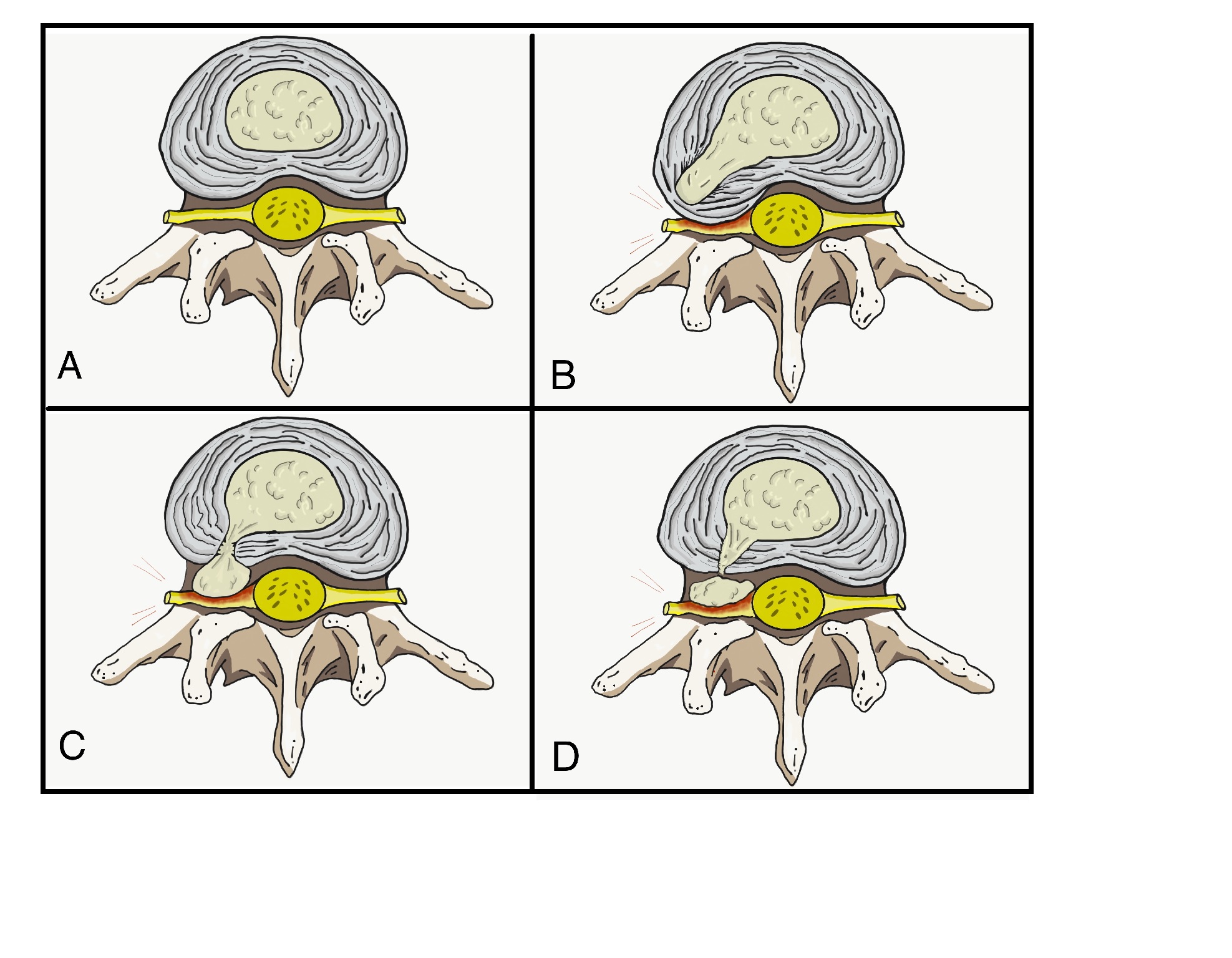
An intervertebral disc is a cartilaginous structure composed of 3 components: an inner nucleus pulposus, an outer annulus fibrosus, and endplates that anchor the discs to adjacent vertebrae. Disc herniation occurs when all or part of the nucleus pulposus protrudes through the annulus fibrosus, and may develop acutely or gradually over time (see Image. Stages of Nucleus Pulposus Herniation). Chronic herniations occur as the intervertebral disc degenerates and dries out with age, typically causing symptoms that develop gradually and are generally less severe. In contrast, acute herniations generally are the result of trauma, resulting in the nucleus pulposus extruding through a defect in the annulus fibrosus. This injury typically results in a sudden onset of more severe symptoms compared to chronic herniations.[5]
Epidemiology
The prevalence of cervical disc herniation increases with age for both men and women and is most common in people in their third to fifth decades of life. This condition occurs more frequently in women, accounting for more than 60% of cases. The most commonly diagnosed patients, regardless of sex, are between the ages of 51 and 60.[6][7]
Pathophysiology
The pathophysiology of herniated discs is thought to be a combination of mechanical compression of the nerve by the bulging nucleus pulposus and a local increase in inflammatory cytokines. Compressive forces can result in varying degrees of microvascular damage, ranging from mild compression, which produces obstruction of venous flow and causes congestion and edema, to severe compression, which can lead to arterial ischemia.
Herniated disc material and nerve irritation may induce the production of inflammatory cytokines, which can include: interleukins 1 and 6, substance P, bradykinin, tumor necrosis factor-alpha, and prostaglandins. There may even be an additional role stretching of the nerve root plays in reproducing symptoms. The trajectory of the cervical nerve as it exits the neural foramen makes it susceptible to stretch, in addition to compression from a herniation. This arrangement could partly explain why certain patients experience pain relief from arm abduction, which presumably decreases the amount of stretch the nerve experiences.[8][9]
Herniations are more likely to occur posterolaterally, where the annulus fibrosus is thinner and lacks the structural support from the posterior longitudinal ligament. Due to the proximity of the herniation to the traversing cervical nerve root, a herniation that compresses the cervical root as it exits can result in radiculopathy in the associated dermatome.[10] Nucleus pulposus herniations manifest in several forms. A disc protrusion arises when the nucleus pulposus bulges yet remains confined within the annulus. Breaching through damaged annular fibers allows nucleus pulposus material to escape, producing a disc extrusion. Detached portions of the extruded nucleus pulposus form a sequestered fragment.
Degenerative disc disease, cervical spondylosis, and disc herniation represent interlinked stages of cervical spine degeneration.[11][12] Degenerative disc disease describes the progressive biochemical and structural deterioration of intervertebral discs, leading to dehydration, annular tears, and a loss of shock-absorbing function. This process often contributes to broader osteoarthritic changes of the cervical spine known as cervical spondylosis. Within this context, a disc herniation occurs when compromised annular fibers allow the nucleus pulposus to extend into the spinal canal or neural foramina—a focal complication rooted in the ongoing degeneration of the disc.
History and Physical
History
Cervical disc herniations most commonly occur between C5–C6 and C6–C7 vertebral bodies, causing symptoms at C6 and C7, respectively. The history of these patients should include the chief complaint, onset of symptoms, factors that alleviate and aggravate symptoms, radicular symptoms, and any past treatments. The most common subjective complaints are axial neck pain and ipsilateral arm pain or paresthesias in the associated dermatomal distribution.
Symptom patterns can also categorize cervical disc herniations:
- Axial neck pain: Pain centered in the cervical spine that typically worsens with movement or mechanical stress, such as lifting or prolonged posture.
- Radiculopathy: Radiating arm pain, sensory changes, or motor weakness along 1 or more dermatomes as herniated material compresses a nerve root.[13]
- Myelopathy: This includes spinal cord involvement producing gait disturbance, hand clumsiness, hyperreflexia, or spasticity.[14]
Any single pattern may occur, but patients frequently exhibit overlapping features, eg, neck pain accompanied by radicular symptoms, or radiculopathy evolving into myelopathy as cord compression progresses. Recognizing these symptom constellations clarifies diagnosis and informs the urgency of imaging, nonoperative trials, and the need for timely surgical decompression. As part of evaluating neck pain, it is essential to identify certain red flags indicative of underlying inflammatory conditions, malignancy, or infection.[15] These include:
- Fever, chills
- Night sweats
- Unexplained weight loss
- History of inflammatory arthritis, malignancy, systemic infection, tuberculosis, HIV, immunosuppression, or drug use
- Unrelenting pain
- Point tenderness over a vertebral body
- Cervical lymphadenopathy
Physical Examination
The clinician should assess the patient’s range of motion, which can indicate the severity of pain and degeneration. A thorough neurological examination is necessary to evaluate sensory disturbances, motor weakness, and deep tendon reflex abnormalities. Careful attention should also focus on any sign of spinal cord dysfunction (see Image. Nucleus Pulposus Herniation, Tables). These include the following:
- C1 and C2: Disc herniations do not affect the occiput–C1 and C1–2 levels (ie, intervertebral discs are absent at these articulations)
- C3, C4: Vague neck, trapezial tenderness, and muscle spasms
- C5: Neck, shoulder, and scapula pain; lateral arm paresthesia; primary movements affected include shoulder abduction and elbow flexion; diminished biceps reflex
- This may also show weakness with shoulder flexion, external rotation, and forearm supination.
- C6: Neck, shoulder, and scapula pain; paresthesia of the lateral forearm, lateral hand, and lateral 2 digits; primary movements affected include elbow flexion and wrist extension
- This may also show weakness in shoulder abduction, external rotation, forearm supination, and pronation—diminished brachioradialis reflex.
- C7: Neck and shoulder pain, paresthesia of the posterior forearm and third digit, diminished triceps reflex.
- The primary movements affected include elbow extension and wrist flexion.
- C8: Neck and shoulder pain; paresthesia of the medial forearm, medial hand, and medial 2 digits; weakness during finger flexion, handgrip, and thumb extension
- T1: Neck and shoulder pain, paresthesia of the medial forearm, weakness of finger abduction and adduction [10]
Provocative tests include the Spurling test, Hoffman test, and Lhermitte sign. The Spurling test can aid in diagnosing acute radiculopathy and is performed by maximally extending the neck and rotating towards the involved side while compressing the head to load the cervical spine axially. This narrows the neuroforamen and may reproduce symptoms consistent with radiculopathy. The Hoffman test and Lhermitte sign can be used to assess for the presence of spinal cord compression and myelopathy. The Hoffmann sign is elicited by holding the third finger and briskly flicking the distal phalanx downward; a positive sign results when there is flexion and adduction of the thumb. The Lhermitte sign is performed by flexing the patient’s neck, which may result in an electrical sensation traveling down the spine and into the extremities.[8][16]
Myelopathy
Degenerative cervical myelopathy manifests with a wide range of symptoms. Common complaints include hand tingling, numbness, clumsiness, weakness, and gait instability.[17] Less typical manifestations represent roughly 40% of cases. A sensation of heavy legs is the only early finding linked to a quicker diagnosis.[18] Physical signs can be subtle. The Tromner sign and overall hyperreflexia offer the greatest sensitivity, whereas Babinski, Tromner, clonus, and the inverted supinator sign show high specificity. Upper motor neuron signs may be absent, so clinicians must integrate the complete symptom profile with imaging studies to establish the diagnosis.[19]
Evaluation
Most cases of acute disc herniation resolve within the first 4 weeks without intervention. Imaging is generally not recommended during this period, as it typically does not alter management. However, imaging should be considered when there is clinical suspicion of serious underlying pathology or evidence of neurologic compromise. Additionally, patients who fail to respond to conservative treatment after 4 to 6 weeks warrant further evaluation.[20] Patients who exhibit red flag symptoms listed above may warrant evaluation with lab markers.
Pertinent lab values in the assessment of cervical disc herniation include:
- Erythrocyte sedimentation rate and C-reactive protein: These are inflammatory markers that should be obtained if a chronic inflammatory condition is suspected, such as rheumatoid arthritis, polymyalgia rheumatica, or seronegative spondyloarthropathy. These can also be beneficial if an infectious etiology is suspected.
- Complete blood count with differential: This is useful when infection or malignancy is suspected.
X-rays are the first test typically performed and are very accessible at most clinics and outpatient offices. Three views (anteroposterior, lateral, and oblique) help assess the overall alignment of the spine as well as the presence of any degenerative or spondylotic changes. These can be further supplemented with lateral flexion and extension views to assess for the presence of instability. If imaging demonstrates an acute fracture, further investigation is required using a computed tomography scan or magnetic resonance imaging (MRI). If there is a concern about atlantoaxial instability, the open-mouth (odontoid) view may assist in diagnosis.
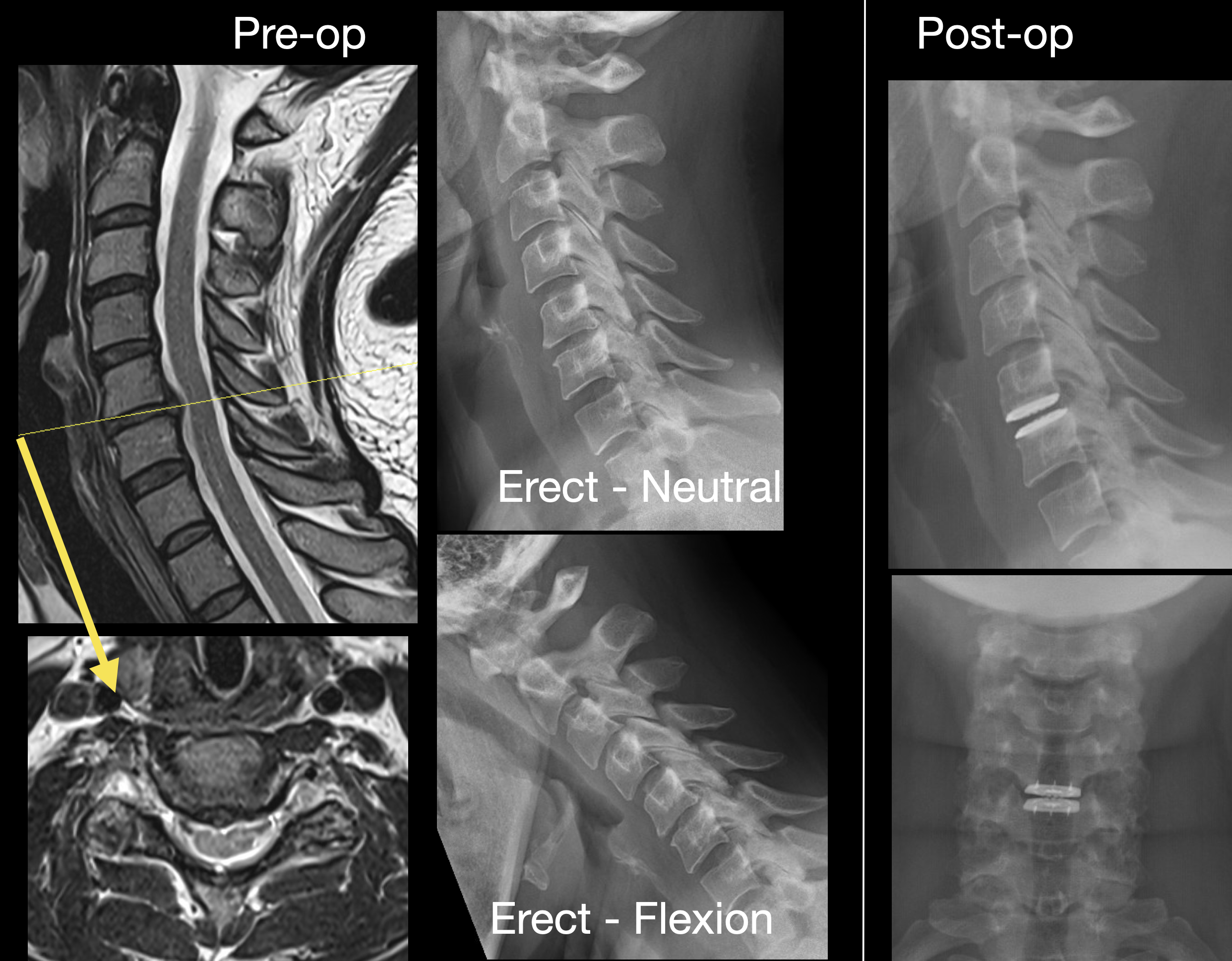
A computed tomography scan is the most sensitive for examining the bony structures of the spine. This imaging can also reveal calcified herniated discs or any insidious process that may lead to bony loss or destruction. In patients who are unable to undergo or are otherwise ineligible for an MRI, computed tomography myelography can be used as an alternative to visualize a herniated disc. MRI is the preferred imaging modality and the most sensitive study for visualizing a herniated disc, as it has the greatest ability to demonstrate soft-tissue structures and the nerve as it exits the foramen (see Images. Cervical Spondylosis, Magnetic Resonance Image; Disc Herniations at C3–4 and C4–5, Magnetic Resonance Image; C5–6 Central Disc Herniation, Magnetic Resonance Image).
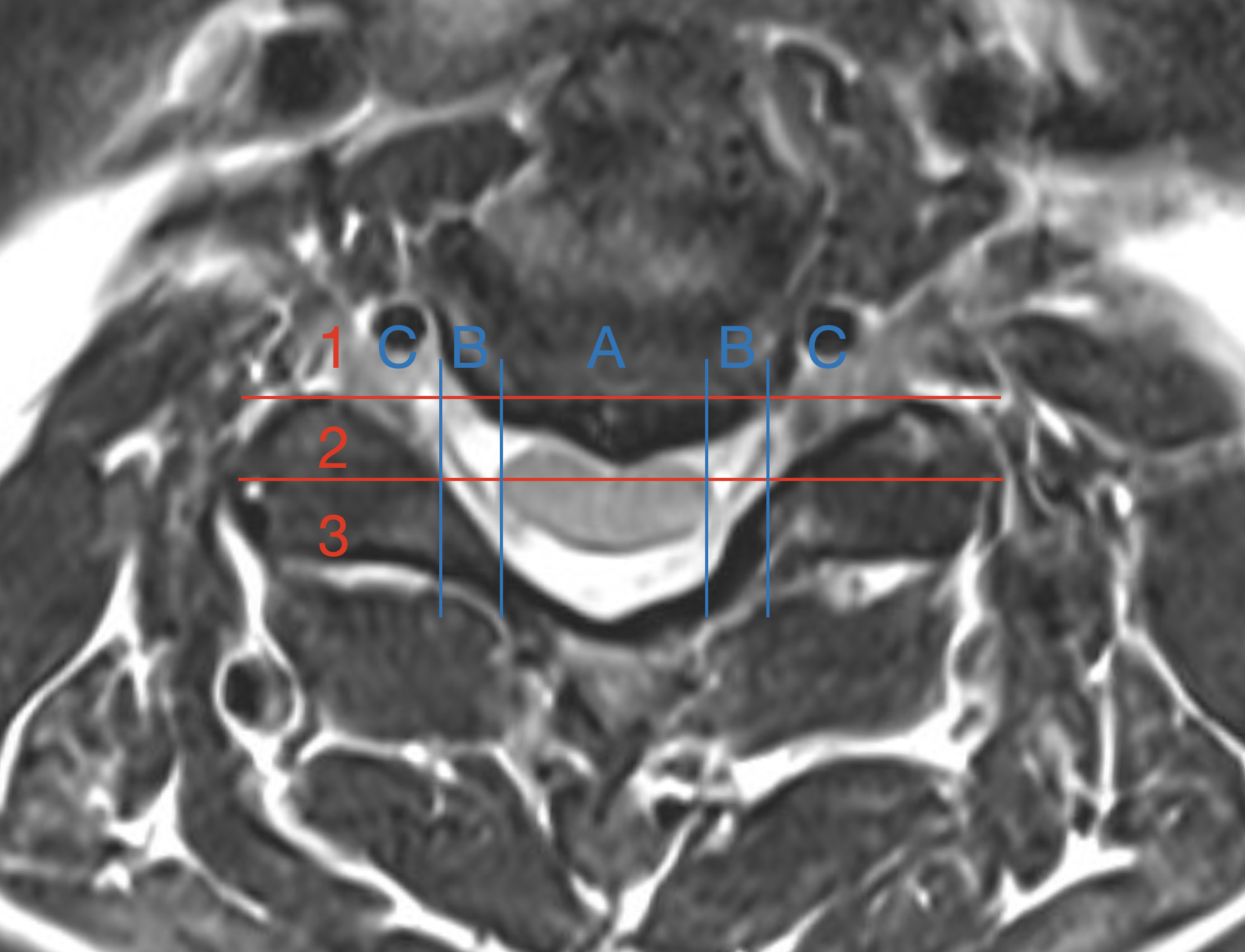
A recent attempt to classify the location and size of disc herniations introduced the foramen facet spinal system, which categorizes cervical disc herniations seen on MRI by their posterior depth and mediolateral location (see Image. Foramen Facet Spinal Disc Herniations, Magnetic Resonance Image). A posterior foraminal line and a line through the midpoint of the facet joint serve as fixed reference landmarks. Grade 1 lesions remain anterior to the foraminal line, grade 2 lesions reach the articular midline, and grade 3 lesions extend beyond. Location code A denotes central compression, B denotes paracentral compression, and C denotes foraminal compression, with AB used when central and paracentral contact are equal, yielding 7 distinct classes.[21] Electrodiagnostic testing, including electromyography and nerve conduction studies, may be useful for patients with inconclusive symptoms or imaging results, and can help differentiate cervical pathology from peripheral mononeuropathy. The sensitivity of detecting cervical radiculopathy with electrodiagnostic testing ranges from 50% to 71%.[22]
Treatment / Management
Conservative Treatment
Acute cervical radiculopathies secondary to a herniated disc are typically managed with nonsurgical treatments, as 75% to 90% of patients improve. Modalities that can be used include:
- Collar immobilization: During the acute inflammatory period, approximately 1 week of collar immobilization may benefit patients with acute neck pain.
- Traction: This may be beneficial in reducing the radicular symptoms associated with disc herniations. Theoretically, traction would widen the neuroforamen and relieve the stress placed on the affected nerve, which, in turn, would improve symptoms. This therapy involves placing approximately 8 to 12 lbs of traction at an angle of approximately 24° of neck flexion for 15 to 20 minutes.
- Pharmacotherapy: There is no evidence to demonstrate the efficacy of nonsteroidal anti-inflammatory drugs in treating cervical radiculopathy. However, they are commonly used and can be beneficial for some patients.
- The analgesic effect does not differ between COX-1 and COX-2 inhibitors; however, COX-2 inhibitors may be associated with decreased gastrointestinal toxicity.
- Clinicians can consider steroidal anti-inflammatory medications, typically prednisone, in severe acute pain for a short period. A typical regimen involves a prepackaged, tapered dose of Methylprednisolone that decreases from 24 mg to 0 mg over 7 days.
- Opioid medications are generally avoided due to a lack of supporting evidence and a higher risk of side effects.
- When muscle spasms are severe, a short course of muscle relaxants, such as cyclobenzaprine at 5 mg, taken orally 3 times daily, may be considered.
- Antidepressants like amitriptyline and anticonvulsants such as gabapentin and pregabalin are sometimes used to manage neuropathic pain and can offer moderate pain relief.
- Physical therapy: These treatments are commonly prescribed following a brief period of rest and immobilization. They include a range of motion exercises, strengthening exercises, ice, heat, ultrasound, and electrical stimulation therapy. Although frequently used, there is no evidence to show that they are more effective than a placebo. However, since they have not been shown to cause harm and may offer some benefit, their use is recommended when myelopathy is not present.
- Cervical manipulation: There is limited evidence suggesting that cervical manipulation may provide short-term benefits for neck pain and cervicogenic headaches. Complications from manipulation are rare and can include worsening radiculopathy, myelopathy, spinal cord injury, and vertebral artery injury.[5][8][23]
Interventional Treatments
Perineural injections (translaminar and transforaminal epidurals, selective nerve root blocks) are an option when MRI confirms pathology. These procedures should take place under radiologic guidance.[23] Over the past few years, neuromodulation techniques have been widely used to manage radicular pain secondary to disc herniations.[24] These neuromodulatory techniques primarily consist of a spinal cord stimulation device and an intrathecal pain pump.[25][26] These devices provide minimally invasive and efficacious treatment options for patients who are not candidates for surgical intervention.(A1)
Surgical Treatment
Indications for surgical intervention include severe or progressive neurological compromise and significant pain that is refractory to nonoperative measures. Several techniques are described based on pathology. The gold standard remains the anterior cervical discectomy with fusion, as it allows for the removal of the pathology and prevents recurrent neural compression by performing a fusion (see Figure. Zero Profile Implant, Cervical Disc Prolapse Radiograph). A posterior laminoforaminotomy can be a consideration in patients with lateral herniations. Total disc replacement is a relatively new treatment option, although its specific indications are still debated.[8]
Differential Diagnosis
Accurate diagnosis requires a structured differential because many disorders replicate the pain or neurologic deficits of cervical disc herniation. Differential diagnoses include:
- Brachial plexus injury
- Degenerative cervical spondylosis
- Muscle strain
- Parsonage-Turner syndrome
- Peripheral nerve entrapment
- Tendinopathies of the shoulder
Prognosis
Pain, restricted motion, and radiculopathy resulting from a herniated disc typically subside on their own within 6 weeks in most patients, due to enzymatic resorption or phagocytosis of the extruded disc material. There may also be a change in the hydration of the extruded material or a decrease in the local edema, resulting in pain reduction and restoration of function. In approximately one-third of patients, symptoms persist despite nonoperative intervention. If symptoms persist beyond 6 weeks, the likelihood of improvement without surgical intervention decreases.[23][27]
Complications
Without intervention, cervical disc herniation, causing compression of neural structures, can cause irreversible neurological impairment. Complications from steroid injections are typically mild and occur in 3% to 35% of cases. Other, more serious complications can include:
Complications from surgical intervention include:
- Infection
- Recurrent laryngeal, superior laryngeal, and hypoglossal nerve injuries
- Esophageal injury
- Vertebral and carotid injuries
- Dysphagia
- Horner syndrome
- Pseudoarthrosis
- Adjacent segment degeneration [29]
Anterior cervical discectomy with fusion is a widely performed procedure to treat disc herniations. According to a meta-analysis, the overall morbidity rate is about 16%, with a mortality rate of 0.1%. The most frequent complication is prevertebral or neck swelling, occurring in 11.3% of cases, followed by pseudarthrosis at 10% and dysphagia at 9.5% occurrence.[30]
Deterrence and Patient Education
Cervical disc herniation often develops from accumulated mechanical stress and modifiable lifestyle factors. Patients benefit from guidance to reduce repetitive overhead tasks, heavy lifting, prolonged driving, and exposure to vibrating tools. Incorporating scheduled microbreaks, ergonomic workstation redesign, and mechanical aids can help reduce cervical load. Emphasizing smoking cessation is critical, as nicotine restricts disc nutrition and delays healing.
Instruction on maintaining neutral cervical posture during daily activities is equally important. Aligning the ears with the shoulders, placing screens at eye level, and rotating the trunk rather than twisting the neck when lifting can help protect cervical structures. Regular aerobic conditioning, combined with targeted neck and scapular strengthening, improves endurance and reduces the risk of recurrence, with supervised exercise programs often showing better adherence and outcomes.
Patients should be informed that approximately 90% of acute cervical disc herniations improve within 12 weeks without surgery, supporting initial nonoperative management when appropriate. Pharmacologic treatment may include short courses of nonsteroidal anti-inflammatory drugs or oral steroids to relieve acute radicular pain. At the same time, opioids should be reserved for severe, refractory cases due to the risk of dependence and delayed recovery. Adjunctive strategies can relieve symptoms, such as heat and intermittent cervical traction.
A soft cervical collar may help alleviate episodes of severe pain, but it should be used briefly to avoid stiffness. A contoured pillow that preserves cervical lordosis can enhance nighttime comfort. High-velocity cervical manipulation should be avoided, as it may worsen neurologic compromise. Patients should understand the importance of seeking prompt reassessment if they experience new or progressive weakness, gait disturbance, bladder or bowel dysfunction, or persistent severe pain. Early imaging and referral to a specialist help prevent irreversible neurologic damage. Providing a clear follow-up plan and reinforcing adherence to exercise and lifestyle modifications support recovery and empower patients to participate in their care actively. Offering reliable educational resources from organizations such as the American Academy of Orthopedic Surgeons and the American Academy of Physical Medicine and Rehabilitation can further support informed decision-making and shared discussions about surgical options when indicated.
Enhancing Healthcare Team Outcomes
Neck pain is a common concern in primary care and specialty clinics. The differential diagnosis is broad, and disc herniations often coexist with other cervical spine conditions. A careful history, including prior treatments, and a detailed physical examination, especially with attention to neurologic findings, helps clinicians assess the severity of the disease and determine the urgency of further evaluation.
Managing cervical disc herniations can be complex and typically requires an interprofessional team. This team may include primary care clinicians, emergency clinicians, orthopedic surgeons, neurosurgeons, radiologists, pain specialists, chiropractors, physical therapists, nurses, and pharmacists. Primary care clinicians gather a thorough history, perform targeted neurologic exams, and identify red flags that prompt urgent imaging. Radiologists interpret MRI or computed tomography studies to confirm nerve or cord compression, which helps guide treatment planning.
Most cervical disc herniations improve within several weeks without the need for invasive treatment. When symptoms persist, conservative measures, such as nonsteroidal anti-inflammatory drugs and physical therapy, are often effective for many patients. Pharmacists play a critical role by counseling patients on pain medication options, monitoring for adverse effects and events, and collaborating with clinicians to limit adverse outcomes. If opioids are used, their prescription is carefully monitored by the healthcare team. For patients experiencing significant pain, referral to a pain specialist for consideration of image-guided injections may be appropriate. Nurses encourage participation in rehabilitation programs, support adherence to treatment plans, and communicate progress or setbacks to the interprofessional team. Physical therapists create individualized exercise plans to enhance strength and flexibility, monitor functional improvements, and adjust interventions as necessary.
When conservative management is unsuccessful or if significant neurological deficits develop, surgical referral is indicated. Spine surgeons and neurosurgeons can then discuss operative options with the patient. While moderate evidence supports certain surgical interventions, decisions should be patient-centered and multidisciplinary.[31] Ultimately, coordinated communication among all members of the interprofessional team helps optimize outcomes for patients with cervical disc disease.
Media
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)
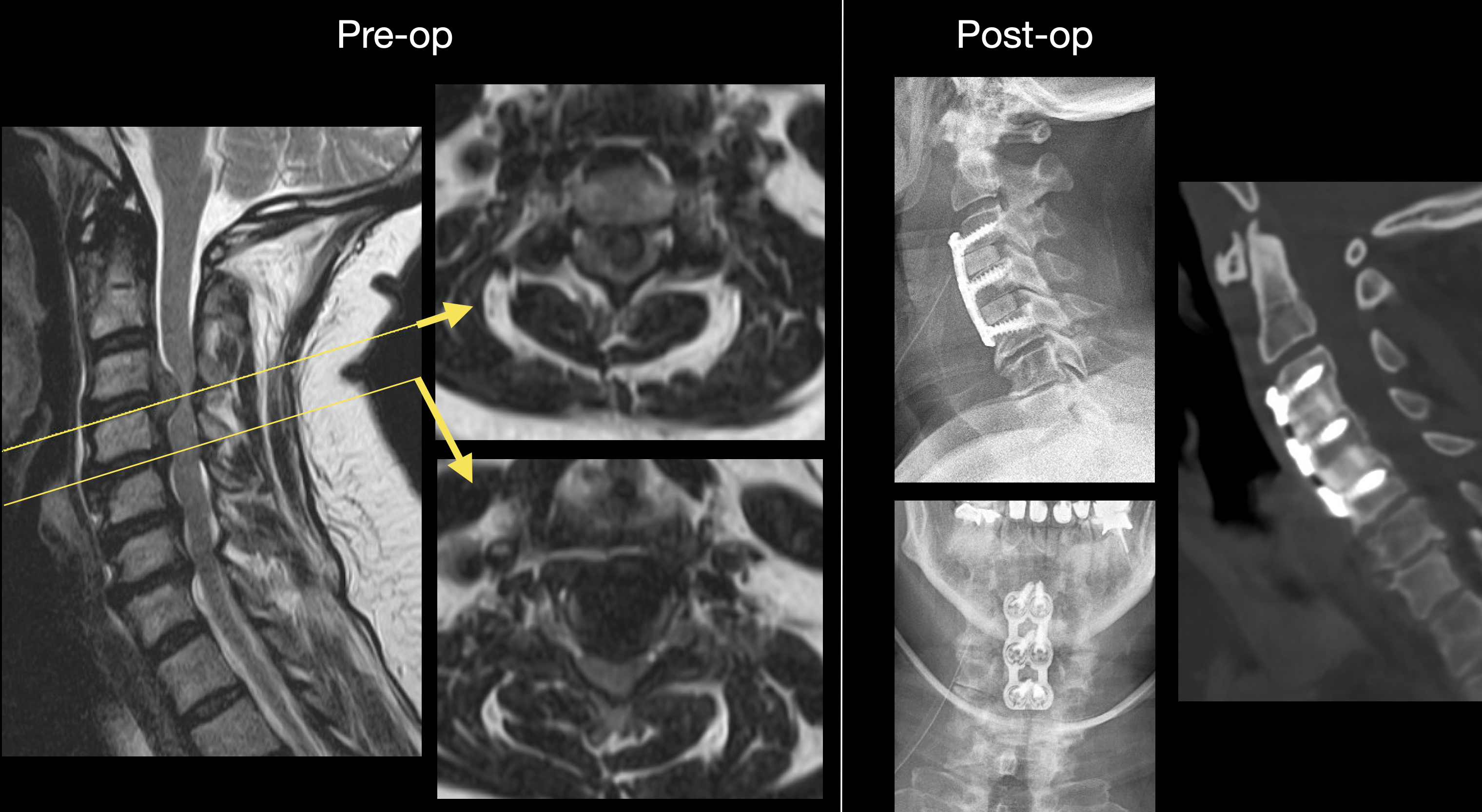
Disc Herniations at C3–4 and C4–5, Magnetic Resonance Image. The sagittal and axial T2 magnetic resonance image views show disc herniations mainly at C3–4 and C4–5. The disc herniations were treated with a C3–C5 anterior cervical discectomy and fusion using an allograft strut graft, anterior plate, and screw instrumentation. Anteroposterior and lateral radiographs were obtained. Postoperative sagittal CT (bone window) demonstrates C3–C5 fusion.
Contributed by K Margetis, MD, PhD
(Click Image to Enlarge)
References
DeSai C, Jozsa F, Agarwal A. Neuroanatomy, Spine. StatPearls. 2025 Jan:(): [PubMed PMID: 30252389]
Waxenbaum JA, Reddy V, Futterman B. Anatomy, Back, Intervertebral Discs. StatPearls. 2025 Jan:(): [PubMed PMID: 29262063]
Bogduk N. Functional anatomy of the spine. Handbook of clinical neurology. 2016:136():675-88. doi: 10.1016/B978-0-444-53486-6.00032-6. Epub [PubMed PMID: 27430435]
Lee JH, Cheng KL, Choi YJ, Baek JH. High-resolution Imaging of Neural Anatomy and Pathology of the Neck. Korean journal of radiology. 2017 Jan-Feb:18(1):180-193. doi: 10.3348/kjr.2017.18.1.180. Epub 2017 Jan 5 [PubMed PMID: 28096728]
Caridi JM, Pumberger M, Hughes AP. Cervical radiculopathy: a review. HSS journal : the musculoskeletal journal of Hospital for Special Surgery. 2011 Oct:7(3):265-72 [PubMed PMID: 23024624]
Kolenkiewicz M, Włodarczyk A, Wojtkiewicz J. Diagnosis and Incidence of Spondylosis and Cervical Disc Disorders in the University Clinical Hospital in Olsztyn, in Years 2011-2015. BioMed research international. 2018:2018():5643839. doi: 10.1155/2018/5643839. Epub 2018 Mar 25 [PubMed PMID: 29770333]
Kim YK, Kang D, Lee I, Kim SY. Differences in the Incidence of Symptomatic Cervical and Lumbar Disc Herniation According to Age, Sex and National Health Insurance Eligibility: A Pilot Study on the Disease's Association with Work. International journal of environmental research and public health. 2018 Sep 25:15(10):. doi: 10.3390/ijerph15102094. Epub 2018 Sep 25 [PubMed PMID: 30257414]
Level 3 (low-level) evidenceRhee JM, Yoon T, Riew KD. Cervical radiculopathy. The Journal of the American Academy of Orthopaedic Surgeons. 2007 Aug:15(8):486-94 [PubMed PMID: 17664368]
Doughty CT, Bowley MP. Entrapment Neuropathies of the Upper Extremity. The Medical clinics of North America. 2019 Mar:103(2):357-370. doi: 10.1016/j.mcna.2018.10.012. Epub [PubMed PMID: 30704687]
Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. StatPearls. 2025 Jan:(): [PubMed PMID: 28722852]
Fakhoury J, Dowling TJ. Cervical Degenerative Disc Disease. StatPearls. 2025 Jan:(): [PubMed PMID: 32809607]
Sharrak S, Al Khalili Y. Cervical Disc Herniation. StatPearls. 2025 Jan:(): [PubMed PMID: 31536225]
Magnus W, Viswanath O, Viswanathan VK, Mesfin FB. Cervical Radiculopathy. StatPearls. 2025 Jan:(): [PubMed PMID: 28722858]
Donnally III CJ, Hanna A, Odom CK. Cervical Myelopathy. StatPearls. 2025 Jan:(): [PubMed PMID: 29493937]
Binder AI. Cervical spondylosis and neck pain. BMJ (Clinical research ed.). 2007 Mar 10:334(7592):527-31 [PubMed PMID: 17347239]
Malanga GA, Landes P, Nadler SF. Provocative tests in cervical spine examination: historical basis and scientific analyses. Pain physician. 2003 Apr:6(2):199-205 [PubMed PMID: 16883381]
Jiang Z, Davies B, Zipser C, Margetis K, Martin A, Matsoukas S, Zipser-Mohammadzada F, Kheram N, Boraschi A, Zakin E, Obadaseraye OR, Fehlings MG, Wilson J, Yurac R, Cook CE, Milligan J, Tabrah J, Widdop S, Wood L, Roberts EA, Rujeedawa T, Tetreault L, AO Spine RECODE-DCM Diagnostic Criteria Incubator. The Frequency of Symptoms in Patients With a Diagnosis of Degenerative Cervical Myelopathy: Results of a Scoping Review. Global spine journal. 2024 May:14(4):1395-1421. doi: 10.1177/21925682231210468. Epub 2023 Nov 2 [PubMed PMID: 37917661]
Level 2 (mid-level) evidenceMunro CF, Yurac R, Moritz ZC, Fehlings MG, Rodrigues-Pinto R, Milligan J, Margetis K, Kotter MRN, Davies BM. Targeting earlier diagnosis: What symptoms come first in Degenerative Cervical Myelopathy? PloS one. 2023:18(3):e0281856. doi: 10.1371/journal.pone.0281856. Epub 2023 Mar 31 [PubMed PMID: 37000805]
Jiang Z, Davies B, Zipser C, Margetis K, Martin A, Matsoukas S, Zipser-Mohammadzada F, Kheram N, Boraschi A, Zakin E, Obadaseraye OR, Fehlings MG, Wilson J, Yurac R, Cook CE, Milligan J, Tabrah J, Widdop S, Wood L, Roberts EA, Rujeedawa T, Tetreault L, AO Spine RECODE-DCM Diagnostic Criteria Incubator. The value of Clinical signs in the diagnosis of Degenerative Cervical Myelopathy - A Systematic review and Meta-analysis. Global spine journal. 2024 May:14(4):1369-1394. doi: 10.1177/21925682231209869. Epub 2023 Oct 30 [PubMed PMID: 37903098]
Level 1 (high-level) evidenceJenkins HJ, Downie AS, Moore CS, French SD. Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropractic & manual therapies. 2018:26():48. doi: 10.1186/s12998-018-0217-8. Epub 2018 Nov 21 [PubMed PMID: 30479744]
Level 3 (low-level) evidenceWang S, Zhao T, Han D, Zhou X, Wang Y, Zhao F, Shi J, Shi G. Classification of cervical disc herniation myelopathy or radiculopathy: a magnetic resonance imaging-based analysis. Quantitative imaging in medicine and surgery. 2023 Aug 1:13(8):4984-4994. doi: 10.21037/qims-22-1387. Epub 2023 May 29 [PubMed PMID: 37581078]
Level 2 (mid-level) evidenceCohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clinic proceedings. 2015 Feb:90(2):284-99. doi: 10.1016/j.mayocp.2014.09.008. Epub [PubMed PMID: 25659245]
Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. American family physician. 2010 Jan 1:81(1):33-40 [PubMed PMID: 20052961]
Deer TR, Jain S, Hunter C, Chakravarthy K. Neurostimulation for Intractable Chronic Pain. Brain sciences. 2019 Jan 24:9(2):. doi: 10.3390/brainsci9020023. Epub 2019 Jan 24 [PubMed PMID: 30682776]
Deer TR, Grider JS, Lamer TJ, Pope JE, Falowski S, Hunter CW, Provenzano DA, Slavin KV, Russo M, Carayannopoulos A, Shah JM, Harned ME, Hagedorn JM, Bolash RB, Arle JE, Kapural L, Amirdelfan K, Jain S, Liem L, Carlson JD, Malinowski MN, Bendel M, Yang A, Aiyer R, Valimahomed A, Antony A, Craig J, Fishman MA, Al-Kaisy AA, Christelis N, Rosenquist RW, Levy RM, Mekhail N. A Systematic Literature Review of Spine Neurostimulation Therapies for the Treatment of Pain. Pain medicine (Malden, Mass.). 2020 Nov 7:21(7):1421-1432. doi: 10.1093/pm/pnz353. Epub [PubMed PMID: 32034422]
Level 1 (high-level) evidenceJain S, Malinowski M, Chopra P, Varshney V, Deer TR. Intrathecal drug delivery for pain management: recent advances and future developments. Expert opinion on drug delivery. 2019 Aug:16(8):815-822. doi: 10.1080/17425247.2019.1642870. Epub 2019 Jul 19 [PubMed PMID: 31305165]
Level 3 (low-level) evidenceKraemer J. Natural course and prognosis of intervertebral disc diseases. International Society for the Study of the Lumbar Spine Seattle, Washington, June 1994. Spine. 1995 Mar 15:20(6):635-9 [PubMed PMID: 7604337]
Peene L, Cohen SP, Brouwer B, James R, Wolff A, Van Boxem K, Van Zundert J. 2. Cervical radicular pain. Pain practice : the official journal of World Institute of Pain. 2023 Sep:23(7):800-817. doi: 10.1111/papr.13252. Epub 2023 Jun 4 [PubMed PMID: 37272250]
Cheung JP, Luk KD. Complications of Anterior and Posterior Cervical Spine Surgery. Asian spine journal. 2016 Apr:10(2):385-400. doi: 10.4184/asj.2016.10.2.385. Epub 2016 Apr 15 [PubMed PMID: 27114784]
Tavanaei R, Ansari A, Hatami A, Heidari MJ, Dehghani M, Hajiloo A, Khorasanizadeh M, Margetis K. Postoperative complications of anterior cervical discectomy and fusion: A comprehensive systematic review and meta-analysis. North American Spine Society journal. 2025 Mar:21():100596. doi: 10.1016/j.xnsj.2025.100596. Epub 2025 Feb 8 [PubMed PMID: 40145067]
Level 1 (high-level) evidenceGebremariam L, Koes BW, Peul WC, Huisstede BM. Evaluation of treatment effectiveness for the herniated cervical disc: a systematic review. Spine. 2012 Jan 15:37(2):E109-18. doi: 10.1097/BRS.0b013e318221b5af. Epub [PubMed PMID: 21587105]
Level 1 (high-level) evidence