Introduction
Brow ptosis is the descent of the eyebrow from its normal anatomical position to a point at which its appearance is cosmetically displeasing, or visual field deficits develop due to excess soft tissue pushing downwards on the eyelid. Brow ptosis may accompany damage to the frontal branch of the facial nerve, impairing the frontalis muscle's elevation of the brow or maintenance of appropriate brow position at rest.[1] Most commonly, though, brow ptosis is seen in older adults due to age-related involutional change of the facial tissues. Over time, the superomedial aspect of the bony orbital rim loses projection, and the fat pads within and around the orbit descend, predisposing the eyebrow to sag. The fact that the lateral aspect of the eyebrow extends beyond the insertion of the frontalis muscle also contributes to lateral brow ptosis. However, in some individuals, compensatory frontalis contraction can cause paradoxical brow elevation with age despite the underlying bony and soft tissue changes.[2]
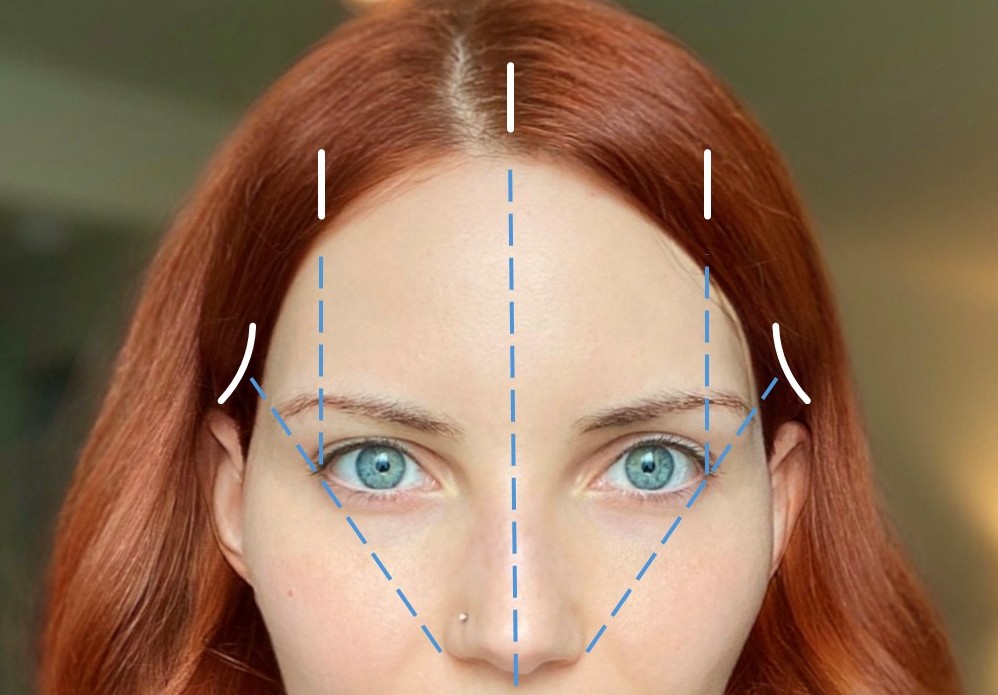
When the eyebrow descends, it compresses the soft tissues of the upper eyelid, weighing them down and often causing excess skin to prolapse over the lid margin and contact the eyelashes, a condition known as pseudoptosis. While pseudoptosis may be mistaken for true blepharoptosis, distinguishing between them is straightforward: elevating the eyebrow to its correct position will alleviate the issue in pseudoptosis, while the lid margin will remain low in cases of true blepharoptosis. There are numerous ways to restore a youthful position to the eyebrows, surgically and nonsurgically, each with advantages and disadvantages. Selecting the most appropriate technique will depend on the patient's goals and the surgeon's expertise and preferences. Each patient has unique eyebrows, determined by shape, position, length, color, density, and prominence. That said, classically accepted aesthetic standards may serve as a starting point for surgical planning if the patient doesn't have specific desires. The medial aspect of the eyebrow is thicker and rounded, and begins along a vertical line through the medial canthus.
In contrast, the lateral end of the eyebrow tapers (more in women than men) and ends roughly on a line drawn through the nasal ala and lateral canthus. The male eyebrow is thick and flat to slightly curved, sitting at the level of the bony supraorbital rim, while the female eyebrow is thinner and often sits above the bony rim; it typically has a peak laterally, above a point located between the lateral limbus of the iris and the lateral canthus (see Image. Brow Positions, Female [Right] and Male [Left]). That said, fashions and cosmetic ideals change with time, particularly for the feminine eyebrow, so the proportions mentioned earlier will not hold for all patients.
Etiology
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Etiology
Brow ptosis is almost always acquired. Congenital brow ptosis is rare and occurs when the facial nerve and/or the frontalis muscle are underdeveloped.
Cases of acquired brow ptosis may arise in a variety of ways:
- Age-related: This is the most common form and is associated with changes in the periorbital tissues. Increased laxity of the connective tissue, skin, and frontalis muscle initially leads to drooping in the lateral third of the eyebrow; this may progress to ptosis of the medial two-thirds if left untreated (see Image. The Frontalis Muscle).[3]
- Traumatic: Damage to the intracranial, intratemporal, or extratemporal facial nerve can cause brow ptosis. A hemifacial palsy will result if the damage occurs anywhere between the facial nerve nucleus proximally and the pes anserinus distally. Damage limited to the frontal branch will denervate the ipsilateral frontalis muscle and parts of the corrugator supercilii, procerus, and orbicularis oculi muscles.[4] Fracture of the temporal bone is one of the most common causes of traumatic facial palsy. Other causes include trauma to the parotid gland, zygomatic arch, and mandibular body.
- Myogenic: Myopathy specific to the facial musculature and systemic myopathy can contribute to brow ptosis via atrophy or denervation of the frontalis muscle. These conditions include myasthenia gravis, myotonic dystrophy, and oculopharyngeal muscular dystrophy.[5]
- Infectious: Ramsay Hunt syndrome is a reactivation of the varicella-zoster virus that leads to facial paralysis and a herpetic rash of the ear canal, auricle, scalp, or oropharyngeal mucous membranes. This condition causes an ipsilateral facial palsy that includes brow ptosis.[6] Many other infectious agents can lead to central or peripheral facial nerve dysfunction, including but not limited to: herpes simplex virus, Borrelia burgdorferi (Lyme disease), Treponema pallidum (syphilis), West Nile virus, human immunodeficiency virus, SARS-CoV-2, and poliovirus.[7][8]
- Spastic: Congenital or acquired spasms of the orbicularis oculi can pull the brow down and away from its anatomic position, eventually causing a permanent change. Examples include blepharospasm and hemifacial spasm.[9]
- Neoplastic: Neoplasms of or infiltrating the facial nerve may affect its function and cause brow ptosis. Some of the most common include cancer of the overlying skin, like melanoma and squamous cell carcinoma, or more proximal masses, like acoustic neuromas.
- Iatrogenic: Operations in the area of the temple and lateral forehead pose a significant risk to the innervation and structural integrity of the brow. Overall, the procedures that pose the highest risk for postoperative facial nerve palsy are temporal artery biopsy, acoustic neuroma resection, and temporomandibular joint procedures. Operations to improve brow and overall facial cosmesis, such as endoscopic and open facelift procedures, can cause facial nerve palsy and exacerbate the problem they were intended to correct, but this occurs in less than 1% of procedures. Botulinum toxin injection also risks brow ptosis; overzealous or misplaced injections effectively denervate the brow elevators.[10]
Epidemiology
Anecdotally, it would appear that most cases are associated with the natural aging process, although literature definitively investigating the epidemiology of brow ptosis is lacking. Congenital brow ptosis is rare, as only 4.9% of facial palsy cases are present at birth.[7] The small proportion of remaining cases is attributable to the other acquired etiologies discussed above.
Pathophysiology
Several soft tissue layers comprise the brow. From superficial to deep, they are the skin, the subcutaneous fat, and the frontalis muscle; deep to this, there are the periosteum and skull—the frontal bone centrally and medially, and the zygomatic bone laterally.[11] The frontalis muscle is the sole elevator of the brow.[12] The depressors of the eyebrow include the orbicularis oculi, procerus, and depressor supercilii muscles (with some anatomists considering the latter to be simply a portion of the orbicularis oculi muscle).[13] The facial nerve innervates all muscles of facial expression; its frontal branch innervates the frontalis and the lateral portions of the orbicularis oculi and corrugator supercilii, while the zygomatic branch innervates the procerus, the medial aspects of the corrugator supercilii and orbicularis oculi, and the depressor supercilii (see Image. Motor and Sensory Supply, Face and Superficial Nerves of the Head and Neck).[14]
Excessive sun exposure, gravity, and the natural involutional degeneration of the skin and underlying tissues are the main contributors to brow ptosis. Denervation of the brow elevators, whether via trauma, surgery, botulinum toxin treatment, or a disease process, will also lead to brow ptosis. Long-term spasm of the brow depressors can cause brow ptosis as well; spasms may result from spastic dystonia after facial denervation, facial tics in conditions like Tourette syndrome, or spastic syndromes like blepharospasm and hemifacial spasm due to irritation of the intracranial facial nerve by the pulsations of a nearby artery (see Image. Typical Blepharospasm).
History and Physical
The historical evaluation of an individual with brow ptosis is key to determining the underlying etiology.
- The history of the present illness should focus on the onset and progression of symptoms. Insidious development of brow ptosis in an older patient may indicate an age-related cause. In contrast, patients with a more rapid onset may be experiencing Bell palsy, trauma, neoplasm, or other more unusual pathologies. A waxing and waning course with accompanying fatigability could represent myotonic dystrophy, myasthenia gravis, or oculopharyngeal dystrophy.
- The medical history should specifically evaluate for past instances of facial paralysis of any etiology, even cases long in the past, as well as any injuries in the upper third of the face or the temporal region.
- A history of chemotherapy and/or radiation therapy should be elucidated, as these exposures can speed cutaneous and soft tissue aging.
- The surgical history should reveal all procedures performed in the area of the brow and along the course of the facial nerve, including any neuro-otologic or neurosurgical procedures. Patients should also be asked if they have received chemodenervation with botulinum toxin injections.
- The social history should reveal sun exposure, smoking, and drug use, as they can all expedite involutional changes.
The physical examination should follow a systematic, stepwise approach generalizable to all periorbital aging.
- Neutral brow position should be evaluated by having the patient close their eyes, relax the facial muscles, and open the eyes as gently as possible without raising the brows. This maneuver is challenging for many patients and may require several attempts.
- Brow versus eyelid pathology should be differentiated by manually elevating the brow to the neutral position. A lid still ptotic after brow elevation indicates true blepharoptosis rather than pseudoptosis caused by a drooping brow and excess skin.
- Blepharoptosis should be thoroughly evaluated. The margin-reflex distance (MRD) is recorded. This is the distance measured from the corneal light reflex to the upper lid margin (MRD-1) or lower lid margin (MRD-2). An MRD-1 of less than 2 to 3 mm is indicative of blepharoptosis. The distance must also be measured between the upper eyelid margin and the superior palpebral crease. More than 8 to 10 mm often indicates blepharoptosis due to levator aponeurosis dehiscence. Any brow position or shape asymmetry should also be noted, even if only due to personal grooming. An asymmetric brow with symmetric eyelids may mask blepharoptosis on the side of the elevated brow due to frontalis contraction compensating for a ptotic eyelid. The ice pack test may be employed at the bedside if myasthenia gravis is suspected: placing an ice pack on the patient's eyelids (with a barrier to prevent frostbite) for 2 to 5 minutes will often improve blepharoptosis in patients with myasthenia gravis.[15] Finally, the patient should be evaluated for the Hering phenomenon. Suppose the elevation of a ptotic eyelid, or the eyelid on the side of the elevated brow, produces drooping of the contralateral upper eyelid. In that case, the patient may have bilateral but asymmetric blepharoptosis. Brow height asymmetry is also commonly caused by hemifacial microsomia, which is more frequently present on the right side than on the left.[16] The presence of hemifacial microsomia is definitively confirmed with computed tomography; however, placing a wooden tongue depressor transversely across the patient's bite, posterior to the incisors, when the patient's head is in a neutral position, will demonstrate an asymmetry of lower facial height if the tongue depressor sits at an angle rather than parallel to the floor.
- To complete a thorough periorbital examination, festoons and fat pseudoherniation should be evaluated with digital pressure on the globe while examining the upper and lower eyelids. The former will not enlarge, but the latter will. Festoons will also contract with effortful eye closure and often extend inferior to the inferior orbital rim, while pseudoherniated fat is contained at the rim by the arcus marginalis. Lower eyelid laxity should be evaluated via the snap test. This is performed by distracting the lid from the globe, then releasing and observing lid recoil, which should take no longer than 2 seconds and occur without the patient needing to blink. The lower eyelid vector should be evaluated by observing the relationship between the cornea and the cheek with the patient's head in the Frankfort horizontal position (a line between the top of the external auditory meatus and the inferior orbital rim is oriented parallel to the floor). The vector is negative if the cornea is anterior to the cheek skin at the infraorbital rim. This is associated with aging and an increased risk of ectropion if lower eyelid blepharoplasty is performed without supporting the lower eyelid concomitantly. Finally, tear production should be evaluated via the Schirmer test. Filter paper is inserted into the fornix of the lower eyelid; if there is less than 10 mm of dampness after 5 minutes, tear production is not adequate, and the surgeon must adjust the operative plan accordingly.
- If brow lifting is to be undertaken, the hairline position and shape of the forehead must be visually evaluated to inform the surgeon's choice of operative approach.
- A thorough cranial nerve exam should be performed, especially if damage to the facial nerve is suspected.[11]
Evaluation
Evaluation of brow ptosis outside of a thorough history and physical examination is rarely necessary. However, there are some cases in which imaging and laboratory studies are beneficial or even diagnostic. Myogenic causes of brow ptosis may be elucidated with certain assays; for example, myasthenia gravis may be diagnosed via serologic testing for acetylcholine receptor antibodies.[17] Brow ptosis caused by a neoplasm will necessitate a thorough evaluation of the mass. These assessments vary widely based on the suspected type of neoplasm, including anything from a shave biopsy to magnetic resonance or positron emission tomography scanning. However, if the decision is made to proceed with brow lifting, preoperative facial photographs should be taken and then posted intraoperatively for reference during surgery. The views should include frontal in repose and with raised eyebrows, as well as bilateral profile views in the Frankfort horizontal position with and without eyebrow raising. Not only does eyebrow raising help assess the function of the frontal branch of the facial nerve and the frontalis muscle, but it may also elucidate the presence of blepharoptosis and pseudoherniation of fat within the lower eyelids.
If the patient wishes to undergo brow lifting, the evaluation should also include attention to the patient's forehead anatomy, specifically the height of the forehead and its degree of convexity. The position of the hairline should be noted, as should the degree of brow ptosis, the heaviness of the brow soft tissues, and whether or not additional surgery will be performed concurrently with the brow lift. Critically, the amount of hair on the scalp should be assessed, as well as any personal or family history of hair loss. These details are fundamental for devising an appropriate surgical plan. For example, patients with low hairlines who would benefit from hairline elevation may be good candidates for coronal brow lifting.
On the other hand, if the hairline needs to be lowered, a pretrichial incision would be more appropriate so that forehead skin may be excised and the scalp advanced. If reduction of the bony brow is necessary for gender affirmation, either a coronal or a pretrichial/trichophytic approach will provide the correct exposure; these approaches are also among the most effective in terms of the degree of brow elevation achievable, although suture suspension is the most powerful in that regard. Tall foreheads with prominent convexities are more challenging to address with an endoscopic technique due to the instruments' limited length and visibility around the frontal bone's curvature. The endoscopic left may also elevate the hairline, albeit subtly. Patients in whom hair loss is anticipated may be poor candidates for coronal or pretrichial brow lifting, because of visible scarring, unless a head covering or hairpiece is to be worn routinely.
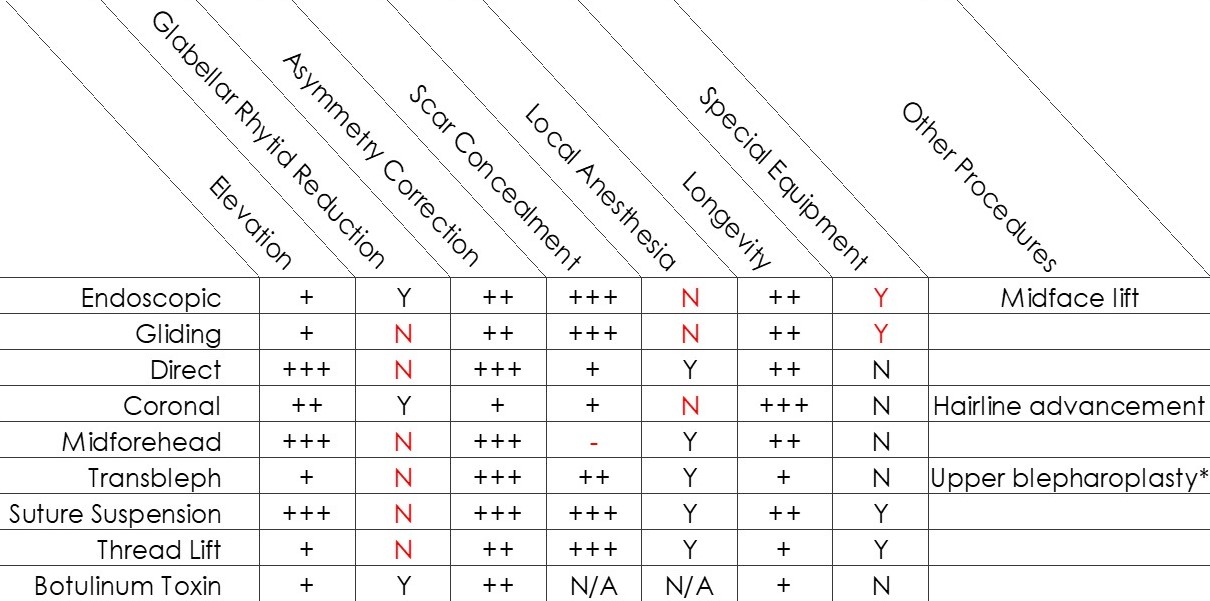
While blepharoplasty may be performed with any surgical brow lift, it is all but mandatory for the transblepharoplasty technique. If midface lifting is desired, it can be accomplished separately from the browlift or as an extension of an endobrow operation. Glabellar rhytids can be reduced through division of the corrugator supercilii muscle using coronal, pretrichial, trichophytic, or endoscopic approaches. Other considerations include the need to correct brow position asymmetry (best achieved with direct, transblepharoplasty, or suture suspension techniques), perform the procedure under local anesthesia (again, direct, transblepharoplasty, or suture suspension), or even avoid surgical intervention altogether (thread lifting or botulinum toxin). For a summary of these considerations and a decision-making aid, please see the Image. Brow Lifting Techniques, Table.
Treatment / Management
Selection of the most appropriate treatment for a given individual with brow ptosis depends on forehead and brow anatomy, ptosis etiology, severity, and, most importantly, patient goals.[18] For age-related brow ptosis, surgical management is most effective. Surgery may also be indicated for some traumatic, neoplastic, and iatrogenic causes. Those surgeries may include nerve decompression, removal of a neoplasm, or nerve reconstruction with or without additional brow lifting. The most common procedures used to treat brow ptosis are discussed below. Many of these procedures may be combined with other rejuvenation procedures, such as upper blepharoplasty, botulinum toxin injection, or skin resurfacing, to optimize patient outcomes and provide a more holistic approach to facial rejuvenation.(B3)
An in-depth understanding of forehead and periorbital anatomy is fundamental to successfully using the following techniques. Medially, the soft tissue of the brow is composed of the skin, subcutaneous fat, galea aponeurotica, loose areolar tissue, and pericranium. Laterally, the conjoint tendon divides the forehead and temporal regions, a confluence of the galea aponeurotica, temporoparietal fascia (TPF), pericranium, and temporalis muscle fascia. The conjoint tendon must be released to allow the forehead to elevate during any type of subperiosteal brow lifting. Lateral to the conjoint tendon, the soft tissue layers include the skin, subcutaneous fat, TPF, superficial layer of the deep temporal fascia, temporal fat pad, temporalis muscle, and pericranium (see Image. Fascial Planes of the Face).
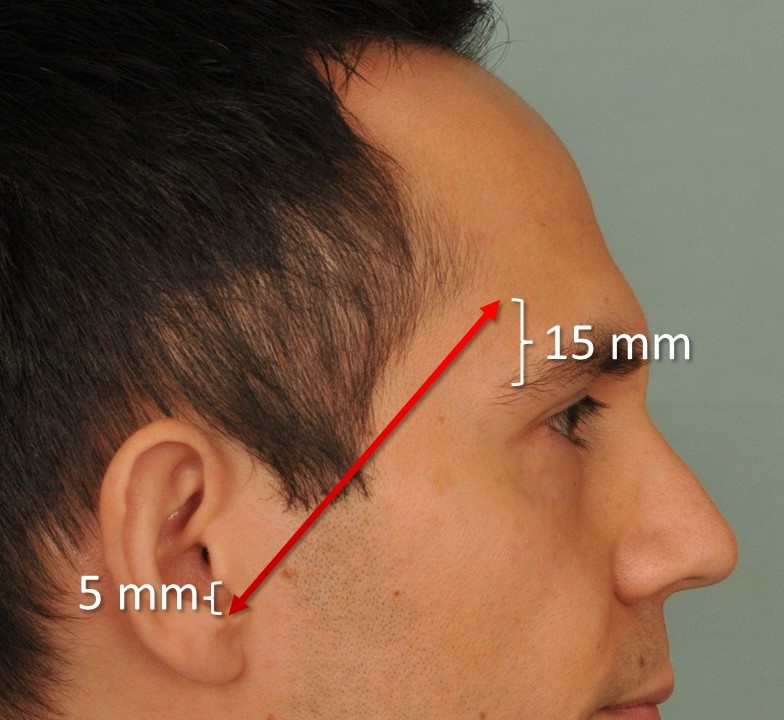
The frontal branch of the facial nerve runs just deep to the TPF along a course approximated by the Pitanguy line. This line runs 0.5 cm below the tragus and 1.5 cm above the lateral extent of the brow (see Image. Pitanguy Line), crossing over the central portion of the zygomatic arch.[19] There may be more than one frontal branch, however, and arborization of the nerve occurs distally, so the Pitanguy line should be considered an indicator of a danger zone, rather than a roadmap to the location of the facial nerve. The supraorbital neurovascular bundle exits the orbit at the midpupillary line and courses superiorly to supply sensation and blood to the lateral brow. The bundle passes through a notch roughly two-thirds of the time and a foramen the other one-third, although the left and right sides may be asymmetric.[20]
Whether there is a notch or a foramen can be an important consideration, particularly during coronal brow lifting, as a foramen may limit the neurovascular bundle's mobility and thereby cause traction or avulsion injuries. The supratrochlear bundle is medial to the supraorbital bundle and supplies sensation and blood to the glabella and medial forehead. Both bundles travel in a plane deep to the frontalis muscle but give off perforating vessels to the overlying skin. Around the periphery of the orbit lies the arcus marginalis, another condensation of connective tissues that brings together the periorbita, the pericranium, and the orbital septum. This too must be divided superiorly and laterally to provide mobility during subperiosteal lifting procedures.
Endoscopic Brow Lift
Described by Isse in 1994, the endoscopic brow lift—or "endobrow" procedure—is one of the most commonly employed approaches to brow lifting (see Image. Endoscopic Brow Lifting, Video).[21] The operation is performed via 5 incisions placed 1 to 2 cm behind the hairline: 1 median and 2 paramedian incisions, each 1 to 2 cm long, and 2 temporal incisions perpendicular to a line drawn from the nasal ala through the lateral canthus. The paramedian incisions are marked directly above the planned peak of the brow. They must be long enough to accommodate whatever apparatus will fixate the forehead in its elevated position (see Image. Endoscopic Brow Lift Incisions). The temporal incisions are used for lateral access to the brow and orbit, but may be converted to fusiform skin excisions if additional temporal lifting is needed. The procedure begins with the development and elevation of a subperiosteal plane down to the level of the supraorbital rims, which can be done under endoscopic visualization or blindly.(B3)
If performed without visualization for rapidity, many surgeons will introduce the endoscope for the last centimeter or so of elevation to ensure the integrity of the supraorbital neurovascular bundles. Posterior subperiosteal elevation is also performed to permit the scalp to move backwards slightly due to the elevated forehead. Laterally, a plane is developed deep to the TPF, on top of the temporalis fascia, and this is followed to the lateral aspect of the orbital rim, taking care to avoid avulsing the medial zygomaticotemporal "sentinel" vein, which lies within 1 cm of the frontal branch of the facial nerve.[22] The periosteum should then be elevated around the orbital rim down to the level of the lateral canthus. However, elevation may continue onto the zygomatic bone if a midface lift is planned. The conjoint tendon must then be released to make the forehead and temporal compartments contiguous, permitting effective brow elevation; dividing the tendon is easiest if approached laterally.
The arcus marginalis is then divided from lateral canthus to lateral canthus to mobilize the brow soft tissues, and the corrugator supercilli muscles may be divided if a reduction in glabellar frown lines is desired, taking care to avoid overly aggressive resection, which may lateralize the medial brows and make them appear unnatural. The forehead is then elevated to the desired position and fixated with one of many methods.[21][23] Resorbable polymer implants may be drilled into the frontal bone to hook the forehead periosteum, suspending it. Alternatively, a "bone bridge" may be drilled into the calvarium, permitting anchorage of a suture that is passed through the periosteum of the forehead. Multiple other techniques have been described as well.[24] If temporal lifting via the lateral incisions is desired, the TPF at the anterior edge of the excision is anchored posterosuperiorly to the temporalis fascia.(B3)
The endoscopic brow lift is best suited for patients with low or average brow height, defined as 6 cm or less from the brow to the hairline, and those without significant forehead curvature or bossing of the brow ridges. Some disadvantages of this technique include the risk of damage to the frontal branch of the facial nerve (which would exacerbate brow ptosis), risk of damage to the supratrochlear and supraorbital nerves (which would cause forehead numbness), difficulty in correcting brow asymmetry (because the forehead is elevated as a unit), and limited ability to achieve a dramatic elevation with this minimally invasive approach (2-4 mm).[25] The most significant limitation on the degree of lift achieved with the endobrow procedure is downward traction from the closure of concomitantly performed upper eyelid blepharoplasty, and the most common complication of this technique is forehead itching.[25]
Gliding Brow Lift
A less technically demanding variant of the endobrow lift is the "gliding brow lift," described by Viterbo and colleagues in 2019.[26] This procedure differs from the traditional endoscopic approach in that the elevation is done blindly in a subcutaneous plane rather than a subperiosteal one. However, similar paramedian incisions are used behind the hairline. The risk of nerve damage is virtually eliminated by dissecting in a subcutaneous plane rather than a subperiosteal one. Still, because skin is very elastic, it must be stabilized effectively during the healing process for the lift to persist. To do so, a "hemostatic net" of 4-0 and 5-0 nylon sutures is placed, taking numerous, regularly spaced bites across the forehead to tack the skin to the underlying muscle. While the sutures appear somewhat alarming immediately after surgery, they reduce the risk of hematoma formation despite the relatively vascular plane of elevation, and they are removed on postoperative day 2. The effect and longevity of this technique are reportedly comparable to those of endoscopic lifting.
Coronal Brow Lift
Open coronal approaches constitute a more traditional category of brow-lifting options. Pretrichial incisions are placed at or just in front of the hairline, while trichophytic incisions are hidden just posterior to the hairline; the classic coronal incision passes directly over the vertex of the scalp and may take a zig-zag or undulating shape for the sake of scar camouflage.[27] Dissection is carried forward from the central part of the incision in the subgaleal plane until diving subperiosteally 1 to 2 cm superior to the orbital rim, unless a pericranial osteoplastic flap or a frontal cranioplasty for gender affirmation is planned, in which case, the dissection may be entirely subperiosteal (see Image. Pretrichial Variant of the Coronal Brow Lift). As with the endoscopic lift, the temporal portions of the elevation occur atop the temporalis fascia to protect facial nerve branches, and the conjoint tendons are also released.
If desired, the corrugator supercilii muscles may be divided to smooth the glabella. Division of the arcus marginalis is also essential in open approaches, and avoiding injury to the supraorbital neurovascular bundles is critical. When the bundles pass through foramina, they may obstruct access to the orbital rim and require osteotomies of the inferior rims of the foramina for complete forehead flap mobilization; performing these osteotomies to convert foramina into notches may place the supraorbital nerves at increased risk of injury if not done carefully. After flap elevation, the excess skin and soft tissue are excised as necessary, and the incision is closed in layers. Coronal brow lifts allow for more dramatic brow elevation than the endoscopic option provides, and they do not require expensive endoscopic equipment; however, they result in significant scars that may be revealed by hair loss and are more likely to cause minor complications like forehead numbness, pruritus, and alopecia, as well as long-term anesthesia or hypesthesia posterior to the incision in nearly all patients.[28]
The pretrichial coronal approach is also commonly used for facial feminization procedures, in which the brow lifting operation is accompanied by adjustment of the frontal hairline and reduction of the supraorbital ridge.[29] If concomitant hairline advancement is desired, subcutaneous elevation posterior to the incision will afford 2 to 4 cm of movement. Still, care should be taken during wound closure to avoid tension, widening the scars, and making them more visible just anterior to the new hairline. Pretrichial or trichophytic incisions may be used for cisgender patients as well; they may make the scar more visible along the anterior hairline, but they will avoid the posterior displacement of the hairline seen with a coronal incision. Importantly, it is critical to counsel patients that while forehead numbness after surgery is most likely due to temporary supraorbital or supratrochlear nerve dysfunction, there will always be some degree of hypesthesia or paresthesia that persists posterior to the incision due to transection of distal sensory nerve branches.
Direct Brow Lift
A far less invasive option than coronal approaches, the direct brow lift is performed through a fusiform excision just above the hair-bearing brows. Excess skin and soft tissue are removed to create a considerable lift with a relatively minor procedure that can easily be performed in the clinic under local anesthesia. This procedure is the most effective option for heavy lateral hooding and is the most straightforward procedure for correcting brow asymmetry.[30] Some drawbacks include the risk of visible scarring—particularly over the medial brow, where the skin is more sebaceous—and an increased chance of excessive elevation that may result in a surprised look. Still, because this technique addresses each brow separately, it is ideally suited for alleviating most cases of brow asymmetry.[31] If additional lift is desired, a 3-0 polydioxanone suture can be used to suspend the dermis of the brow to the periosteum. Still, avoiding injuring or encircling the supraorbital nerve with this suture is important, as it may cause numbness or neuropathic pain.
A “deep plane” variant involves incising orbicularis oculi and suspending the muscle and its underlying fat to improve longevity. Still, this technique should only be employed lateral to the supraorbital nerve, thus making it primarily useful for female brows.[30] The technique of a simple direct brow lift is very straightforward, in that it amounts to nothing more than a skin excision; however, determining where and how much skin to remove is key. A simple way to do this is to have the patient sit upright or stand, and then manually lift the eyebrow to its desired position, holding a marking pen at the level of the top of the brow peak, but not touching the skin. Upon releasing the brow, a dot is placed on the skin where the brow sat when elevated. The same procedure is repeated at a few different locations along the superior margin of the eyebrow, which will delineate the superior extent of the excision. The inferior extent will follow the upper margin of the eyebrow (see Images. Direct Brow Lift Marking and Direct Brow Lift.).
Mid-Forehead Brow Lift
The mid-forehead lift is similar to the direct brow lift, which places the skin excision in a transverse forehead rhytid rather than immediately above the eyebrow; this is primarily a procedure of historical interest due to the often readily apparent scarring it produces.[32] With this procedure, a single, long skin excision can be used to lift both brows together, or individual excisions can be employed on each side, symmetrically or asymmetrically, sharing a rhytid or located at different levels. The higher the excisions are placed, the less effective the lift will be, because the greater the expanse of skin between the lifting point and the brows themselves, the more the skin can stretch and allow the brow to descend.
Suture Suspension Brow Lift
For severe brow asymmetry, unilateral suture suspension of the ptotic brow to a titanium miniplate fixated to the frontal bone at the level of the hairline may be effective. As a side benefit, the sutures can be tightened under local anesthesia if the brow ptosis recurs or worsens. Tessa Hadlock developed the percutaneous suture suspension brow lift at the Massachusetts Eye & Ear Infirmary for use with facial paralysis patients, particularly those who wanted to avoid a direct brow lift scar or for whom a direct brow lift would not provide adequate elevation or longevity (see Image. Right Brow Ptosis With Facial Paralysis). A short, pretrichial incision will later accommodate a 5-hole titanium miniplate, and 3 stab incisions above the brow follow that. A 2-0 silk suture is then threaded through the stab incisions with a reusable Keith needle to create two slings, which are in turn anchored to the miniplate (see Image. Suture Suspension Brow Lifting). The key is to pass the suture through the superficial dermis above the brow to maximize the mechanical advantage, then drive the suture down to the periosteum to meet the miniplate. The procedure can provide a nearly unlimited elevation; however, as with any brow lift, the elevation will decrease over time.
Transblepharoplasty Brow Pexy (Internal Brow Lift)
The transblepharoplasty browpexy is a way to combine the treatment of upper lid dermatochalasis or blepharoptosis with the treatment of brow ptosis.[33] These conditions are often comorbid, which makes this approach an efficient one. However, it is best used for the female brow because the suspension point must be lateral to avoid injury to the supraorbital neurovascular bundle. An upper eyelid blepharoplasty is performed first; then, dissection is carried superiorly along the orbital septum until the supraorbital rim is reached. At this point, either the pericranium can be elevated with the brow if a bioresorbable suspension device is drilled into the bone (similar to an endoscopic brow lift), or the periosteum can be left in place and used to anchor a suture that suspends the brow (similar to a direct brow lift). If a suspension suture is used, it is more challenging to get symmetric results, due to the limited access afforded by the blepharoplasty incision, and the brow tends to take on a feminine peak (see Image. Transblepharoplasty Brow Pexy). The lift is slightly broader and easier to reproduce symmetrically if a suspension implant is placed. In this case, the conjoint tendon's inferior portion must be released to facilitate an effective lift, and the arcus marginalis should be disrupted to mobilize the periosteum. Similar to the results of the endoscopic approach, the lift obtained with this procedure is limited because it is performed with upper eyelid blepharoplasty.
Thread Lifting
Barbed resorbable threads are becoming a popular option for treating the aging face at multiple levels, and even for contouring of the arms and belly. For brow lifting, a blunt cannula is used to place bidirectionally barbed 4-0 sutures ("threads") via stab incisions made with an 18-gauge needle. The sutures themselves have barbs oriented away from a central point on the thread, which allows them to pull up on the brow and anchor into the subdermis simultaneously. Multiple threads are typically deployed along several vectors to achieve the desired effect. Once the sutures are in place, the brow is manually manipulated into the desired position while tension is kept on the thread, thus permitting the barbs to engage. The threads can be tied off and then cut, or just cut and left below the skin surface. When the sutures are made of polydioxanone, the lift should last at least 6 months, but the duration is 2 to 3 times as long if poly-L-lactic acid threads are used.[34][35] The most likely complications of this technique are asymmetry and dimpling or rippling of the skin due to the thread not being situated at an even depth within the subdermis. Usually, these irregularities settle with gentle massage and time.(B3)
Selective Chemodenervation
Lastly, botulinum toxin injections can be used to treat spastic brow ptosis or even slightly elevate the brow by decreasing the resting tone of the depressor supercilii muscle and thereby augmenting the opposing action of the frontalis muscle. A small injection of 1 to 2 units placed just under the skin, inferior to the eyebrow at the lateral canthus level, can help elevate the brow's tail (see Image. Chemical Brow Lift With Botulinum Toxin). This technique is typically reserved for the female brow because injecting more medially risks causing blepharoptosis by weakening the levator palpebrae superioris muscle. If blepharoptosis does result, apraclonidine eyedrops will help to alleviate symptoms. The injections should last 3 to 4 months.
Differential Diagnosis
Brow ptosis is a fairly straightforward and well-defined diagnosis, but it may be confused with or obscured by other periorbital pathologies. Asymmetric brow ptosis may seem like unilateral pathology unless a thorough physical examination reveals that the more ptotic side was masking the appearance of the less ptotic side. Severe dermatochalasis or blepharoptosis may distract the physician from identifying concomitant brow ptosis. A thorough history and physical examination will reveal whether a patient’s brow ptosis is age-related, traumatic, myogenic, spasm-induced, infectious, neoplastic, or iatrogenic.
Prognosis
The prognosis for brow ptosis highly depends on the etiology and the patient's primary concerns. Full resolution and patient satisfaction can usually be achieved for those mainly focused on the visual field deficits caused by their ptotic brows.[36] That said, patients must be counseled that effective rejuvenation does not mean a permanent cessation of facial aging, but rather an offset by 5 to 10 years, so that while they may look persistently younger than expected based on biological age, the brows will descend over time nonetheless. Patients whose concerns are primarily cosmetic have higher dissatisfaction rates than those with predominantly functional complaints. Patients with non–age-related etiologies have more varied prognoses.
Complications
Complications of brow lifting include numbness of the forehead due to supratrochlear or supraorbital nerve damage (5.5%), alopecia (2.8%), temporary or permanent brow asymmetry due to asymmetric elevation or motor nerve injury (1.7%), and patient dissatisfaction (7.4%). Dissatisfaction may stem from many issues, including persistent discomfort from implanted suspension devices, insufficient brow elevation, excessive brow elevation, division of the corrugator muscles that leads to a "surprised" appearance, and unsightly scarring. Nonsurgical brow rejuvenation complications are infrequent. The most common complication of botulinum toxin treatment is periorbital bruising in 1.7% of patients or transient blepharoptosis.[10]
Deterrence and Patient Education
Patients should be educated to their desired level of detail on the pathophysiology of the cause of brow ptosis. Once a sufficient understanding of the pathology is achieved, surgical and non-surgical treatment options should be explained to inform a decision. A thorough discussion of common and rare complications of the selected treatment method is essential before undertaking an operative intervention.
Enhancing Healthcare Team Outcomes
Brow ptosis is a relatively common problem but is frequently misdiagnosed or overlooked due to more apparent upper eyelid pathologies, often because the patient's presenting chief complaint will focus on "eyelid drooping" even when the brow ptosis may be more severe than the dermatochalasis. When patients present to primary care clinicians, they should be referred to a facial plastic, general plastic, or oculoplastic surgeon for definitive treatment. Following this, close coordination among nurses, surgeons, and primary care managers is key to optimizing outcomes and minimizing complications. Cases that are not age-related may require further consultation with neurosurgeons, infectious disease specialists, neurologists, rheumatologists, or other specialists. Intraoperatively, an interprofessional staff of specialty-trained nurses, technicians, and anesthesia providers who are familiar with the equipment and selected procedure will support an experienced surgeon to execute a safe and effective procedure.
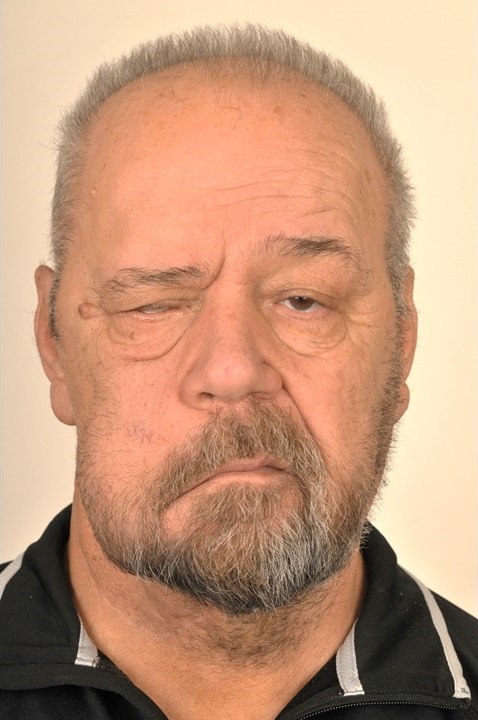
Media
(Click Image to Enlarge)
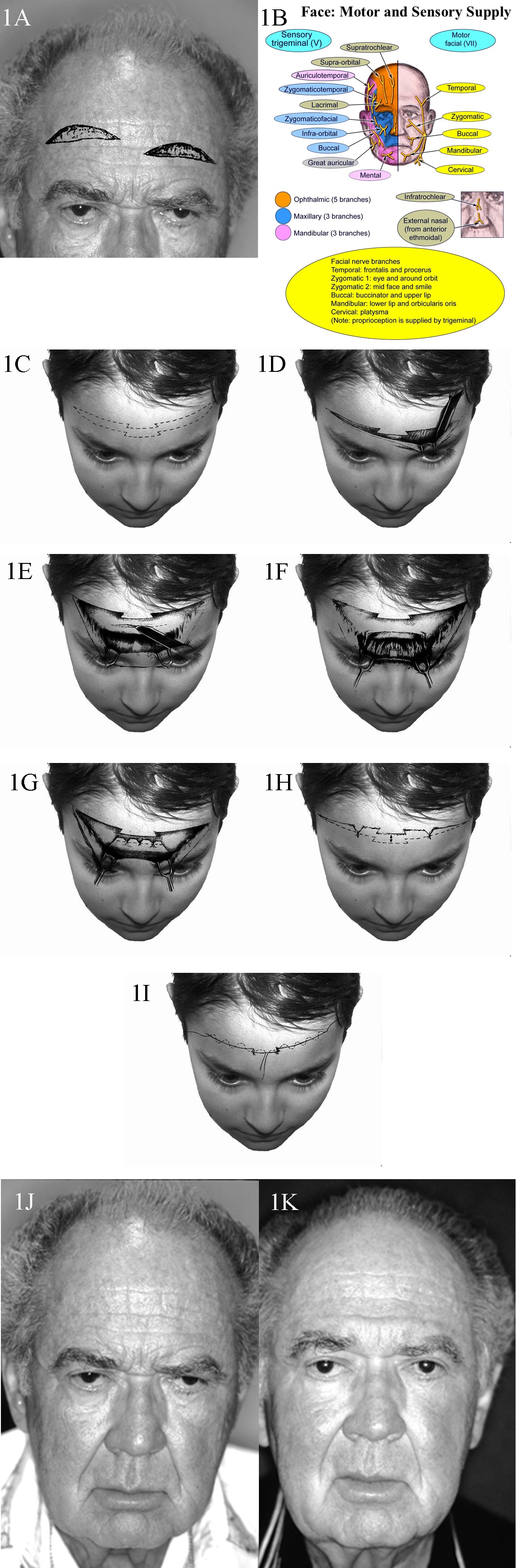
Motor and Sensory Supply, Face. 1A. Patient with typical upper lid ptosis and severe brow ptosis. Incisions for midforehead lift may be staggered to prevent a long horizontal scar. 1B. Face sensory and motor nerve supply. 1C. Transverse forehead incisions may be staggered or broken up to improve the final scar. 1D. Dissection performed in the subcutaneous plane. 1E. Transverse incisions are made in the galea to access the corrugator and procerus muscles. These incisions are kept in the middle to prevent injury to the supraorbital nerve branches. 1F. Once exposed, the corrugator and procerus muscles are attenuated. 1G. The galea is shortened as desired, and sutures are placed. 1H. Elevation of the cutaneous structures is obtained, and relevant trimming is performed. 1I. Meticulous subcuticular closure is performed with no tension on the skin edges. 1J. A man with markedly overactive corrugator and procerus muscles. 1K. A reasonable elevation of his brows has been achieved.
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)
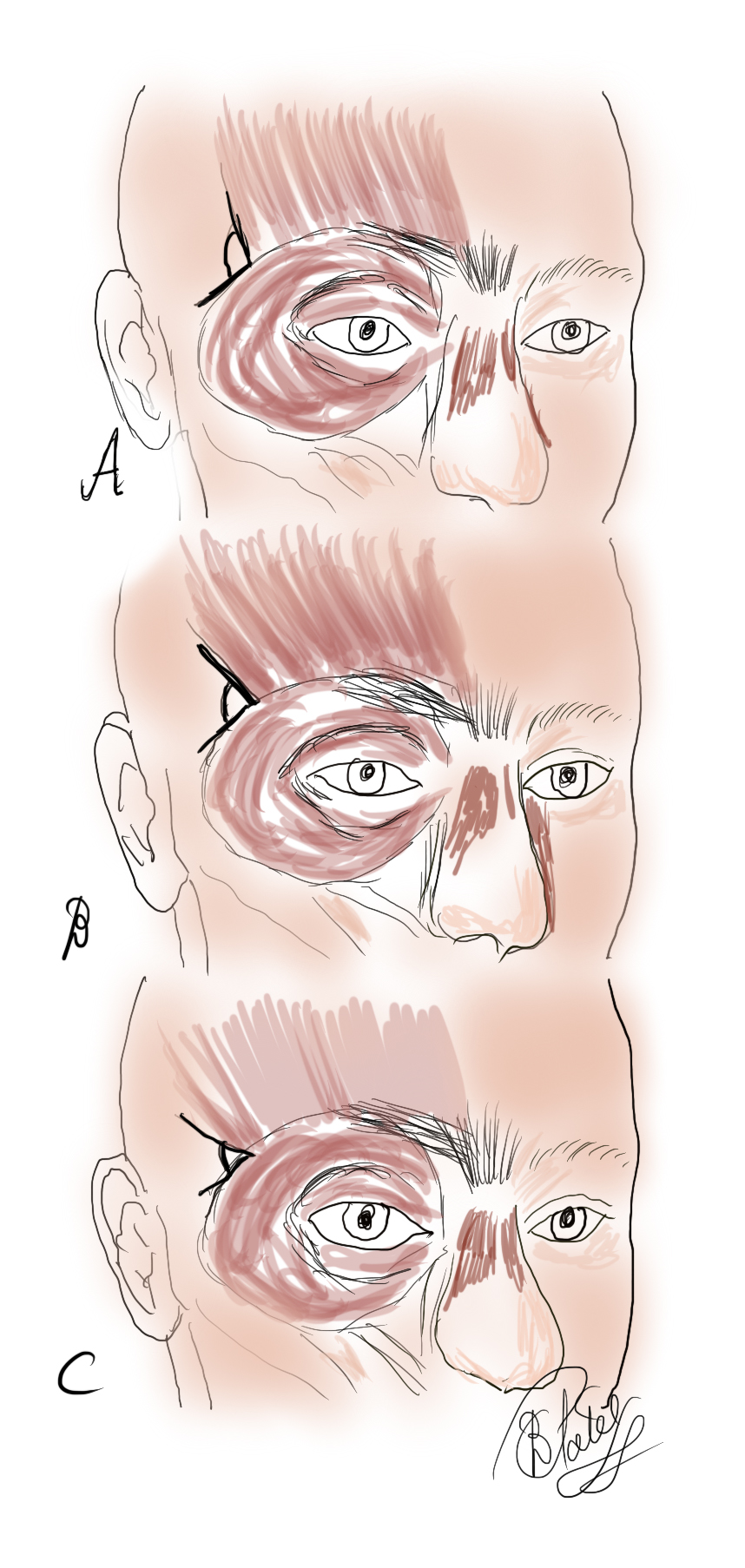
The Frontalis Muscle. The angle of insertion of the frontalis muscle laterally as measured against the orbital orbicularis oculi varies A. Large B. Intermediate C. Small It is thought that with aging, the angle becomes smaller with less lateral support to the brow, thereby contributing to lateral brow ptosis
Contributed by BCK Patel, MD, FRCS
(Click Video to Play)
Typical Blepharospasm, Video. There is an increased blink rate and intermittent but random squeezing of the eyelids and periorbital tissues with overactivity of the corrugator, procerus, and orbicularis muscles. Note the associated brow ptosis, ptosis, and dermatochalasis, all of which are worsened by the blepharospasm.
Contributed by BCK Patel, MD, FRCS
(Click Image to Enlarge)
(Click Video to Play)
Pretrichial Variant of the Coronal Brow Lift, Video. The forehead may be elevated in either a subgaleal/submuscular plane or a subperiosteal plane, with the subperiosteal elevation employed more commonly for gender affirmation surgery. This provides access for frontal cranioplasty. The pretrichial incision is made to look irregular in the central aspect of the hairline for the sake of scar camouflage. Varying amounts of skin excision can be performed depending on whether hairline adjustment is required and how much eyebrow and temporal lift are desired.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
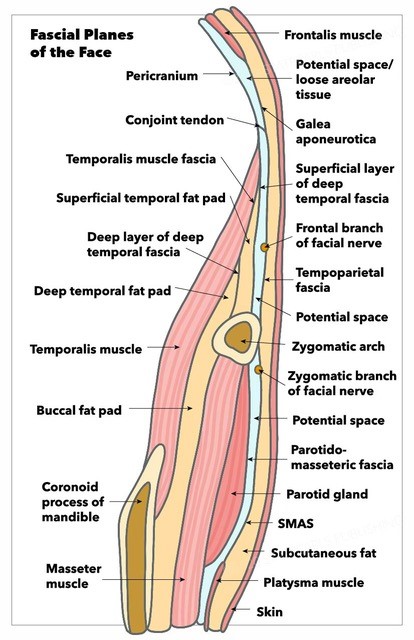
Fascial Planes of the Face. This illustration depicts the fascial planes of the face, highlighting the continuity of the frontalis muscle, galea aponeurotica, temporoparietal fascia, superficial musculoaponeurotic system, platysma, and the location of the facial nerve.
Contributed by K Humphreys and MH Hohman, MD, FACS
(Click Image to Enlarge)
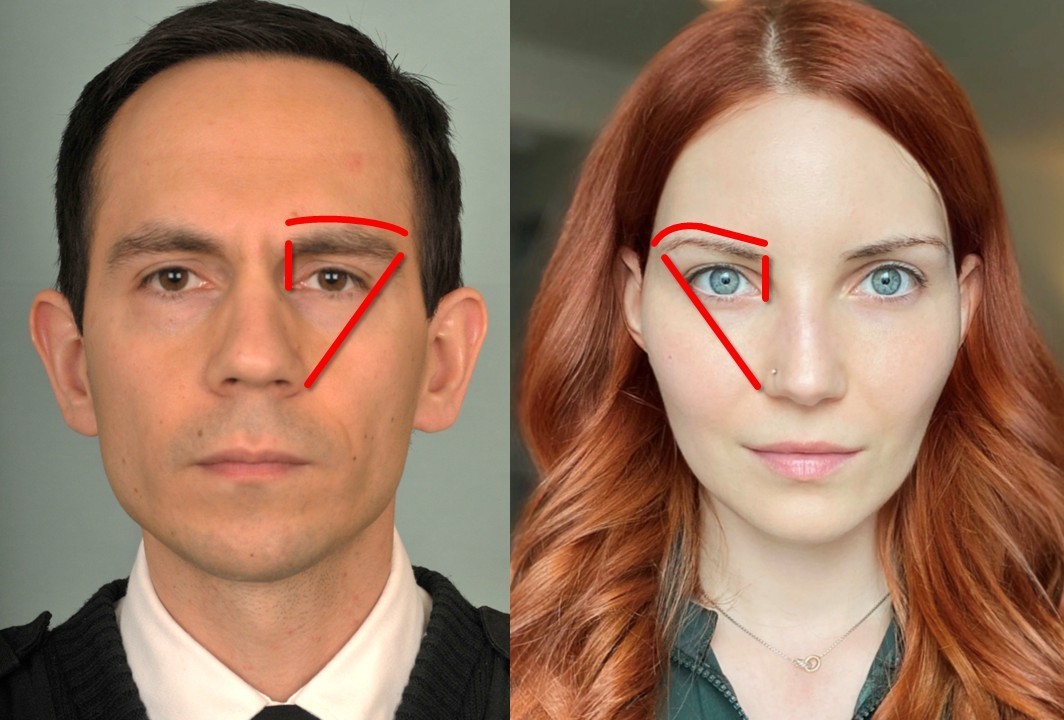
Brow Positions, Female (Right) and Male (Left). Note that the female brow rests above the superior orbital rim, and the male brow sits at the level of the superior orbital rim. The female brow also has a peak above the lateral canthus and is more precisely groomed than the male brow, which does not have a prominent arch or peak. Both brows extend from the medial canthus to a line running from the lateral aspect of the nasal ala through the lateral canthus.
Contributed by M Hohman, MD, FACS, and L Martin, BS
(Click Image to Enlarge)
(Click Video to Play)
Chemical Brow Lift With Botulinum Toxin, Video. Botulinum toxin is used to weaken the depressor supercilii portion of the orbicularis oculi muscle: 1 to 2 units of onabotulinumtoxinA are injected just under the skin/on top of the muscle, at a point on a vertical line below the peak of the brow. This injection will emphasize the brow arch and is therefore typically used for patients who desire a feminine eyebrow appearance. Injection medial to the lateral limbus raises the risk of causing blepharoptosis.
Contributed by MH Hohman, MD, FACS, and J Miller, LPN
(Click Image to Enlarge)
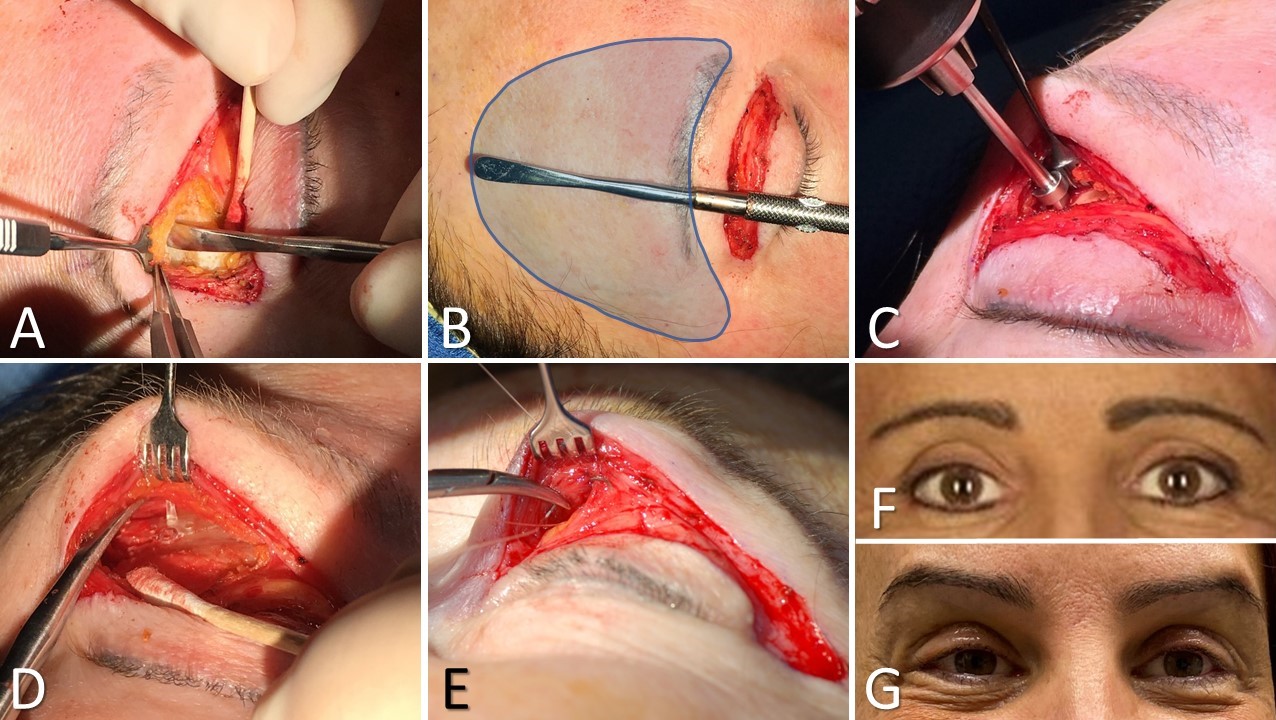
Transblepharoplasty Brow Pexy. The following describe this image: A) Dissection is carried along the orbital septum to the frontal bone, where a subperiosteal flap (pictured) or a subdermal flap is elevated. B) The extent of elevation is marked in blue. C) A well is drilled into the frontal bone if a resorbable suspension implant is to be used. D) The implant is placed into the bone and suspends the periosteum of the brow in an elevated position. E) Alternatively, a long-lasting resorbable suture may be used to suspend the subdermis of the brow to the periosteum. F) Preoperative view. G) One week after suture-based transblepharoplasty brow pexy.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
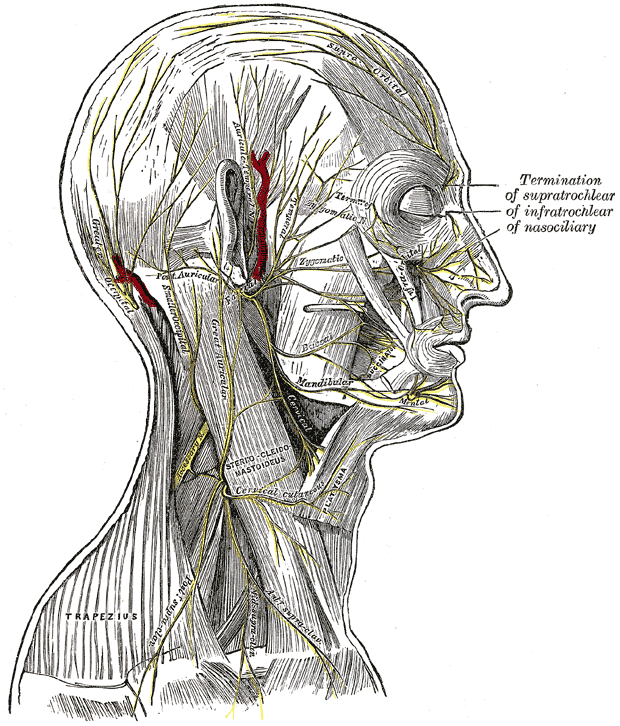
Superficial Nerves of the Head and Neck. The image illustrates the nerves of the scalp, face, and side of the neck. Branches of the facial and auriculotemporal nerves, as well as other cranial nerve divisions, are shown. Terminations of the supratrochlear, infratrochlear, and nasociliary nerves are also labeled. Muscular attachments, vascular structures, and cutaneous distributions are clearly depicted.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
(Click Video to Play)
Suture Suspension Brow Lifting, Video. A short pretrichial incision is made and carried down to the frontal bone to permit placement of a titanium miniplate. Then, 3 stab incisions are made just superior to the brow, and 2 sutures (2-0 silk) are passed to act as slings between the brow and the miniplate. After lifting the brow the desired amount, the sutures are tied to the miniplate, which is screwed down onto the frontal bone. The wound is then closed in 2 layers.
Contributed by MH Hohman, MD, FACS
(Click Image to Enlarge)
Endoscopic Brow Lift Incisions. A 1 to 2 cm midline incision is made 1 to 2 cm behind the hairline. Symmetrical 1 to 2 cm paramedian incisions are made 1 to 2 cm behind the hairline, above the peaks of the brows. Curvilinear temporal incisions, 2 to 3 cm in length, are made 1 to 2 cm behind the hairline, perpendicular to lines running through the nasal alae and lateral canthi. These incisions can be converted to fusiform excisions if additional temporal lifting is desired.
Contributed by MH Hohman, MD, FACS, and L Martin, BS
(Click Video to Play)
Direct Brow Lift Marking, Video. This image depicts a clinician making the preprocedural brow markings directly on the patient's skin.
Contributed by MH Hohman, MD, FACS, and AG Vincent, MD, FACS
(Click Video to Play)
Direct Brow Lift, Video. After marking, the skin is excised down to the level of the muscle, taking care to avoid injury to the supraorbital neurovascular bundle. The dermis of the brow may be suspended to the periosteum with 1 or 3-0 polydioxanone sutures, if a greater lift is desired. Closure is then accomplished in two layers: deep dermal, buried, interrupted 5-0 poliglecaprone sutures and skin surface simple, interrupted 6-0 plain gut.
Contributed by MH Hohman, MD, FACS
(Click Video to Play)
Endoscopic Brow Lifting, Video. This video demonstrates the critical steps of endoscopic brow lifting: developing a subperiosteal flap centrally, developing a sub-temporoparietal fascia flap laterally, joining the planes by dividing the conjoint tendon, avoiding the frontal branch of the facial nerve by preserving the sentinel vein, preserving the supraorbital neurovascular bundle, dividing the corrugator supercilii muscles if desired, releasing the arcus marginalis from lateral canthus to lateral canthus, suspending the frontal periosteum to complete the brow lift, and suspending the temporoparietal fascia to the temporalis fascia laterally for additional temporal lift.
Contributed by MH Hohman, MD, FACS
References
Perumal B, Meyer DR. Facial Asymmetry: Brow and Ear Position. Facial plastic surgery : FPS. 2018 Apr:34(2):230-234. doi: 10.1055/s-0038-1636903. Epub 2018 Feb 21 [PubMed PMID: 29466811]
Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB. The Facial Aging Process From the "Inside Out". Aesthetic surgery journal. 2021 Sep 14:41(10):1107-1119. doi: 10.1093/asj/sjaa339. Epub [PubMed PMID: 33325497]
Glass LR, Lira J, Enkhbold E, Dimont E, Scofield S, Sherwood PR, Winn BJ. The lateral brow: position in relation to age, gender, and ethnicity. Ophthalmic plastic and reconstructive surgery. 2014 Jul-Aug:30(4):295-300. doi: 10.1097/IOP.0000000000000095. Epub [PubMed PMID: 25069068]
Level 2 (mid-level) evidenceGordin E, Lee TS, Ducic Y, Arnaoutakis D. Facial nerve trauma: evaluation and considerations in management. Craniomaxillofacial trauma & reconstruction. 2015 Mar:8(1):1-13. doi: 10.1055/s-0034-1372522. Epub [PubMed PMID: 25709748]
Nair AG, Patil-Chhablani P, Venkatramani DV, Gandhi RA. Ocular myasthenia gravis: a review. Indian journal of ophthalmology. 2014 Oct:62(10):985-91. doi: 10.4103/0301-4738.145987. Epub [PubMed PMID: 25449931]
Jeon Y, Lee H. Ramsay Hunt syndrome. Journal of dental anesthesia and pain medicine. 2018 Dec:18(6):333-337. doi: 10.17245/jdapm.2018.18.6.333. Epub 2018 Dec 28 [PubMed PMID: 30637343]
Hohman MH, Hadlock TA. Etiology, diagnosis, and management of facial palsy: 2000 patients at a facial nerve center. The Laryngoscope. 2014 Jul:124(7):E283-93. doi: 10.1002/lary.24542. Epub 2014 Jan 15 [PubMed PMID: 24431233]
Level 2 (mid-level) evidenceEscalante DA, Malka RE, Wilson AG, Nygren ZS, Radcliffe KA, Ruhl DS, Vincent AG, Hohman MH. Determining the Prognosis of Bell's Palsy Based on Severity at Presentation and Electroneuronography. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2022 Jan:166(1):151-157. doi: 10.1177/01945998211004169. Epub 2021 Mar 30 [PubMed PMID: 33784203]
Lee S, Park S, Lew H. Long-term Efficacy of Botulinum Neurotoxin-A Treatment for Essential Blepharospasm. Korean journal of ophthalmology : KJO. 2018 Feb:32(1):1-7. doi: 10.3341/kjo.2017.0030. Epub 2018 Jan 24 [PubMed PMID: 29376224]
Hohman MH, Bhama PK, Hadlock TA. Epidemiology of iatrogenic facial nerve injury: a decade of experience. The Laryngoscope. 2014 Jan:124(1):260-5. doi: 10.1002/lary.24117. Epub 2013 Apr 18 [PubMed PMID: 23606475]
Level 2 (mid-level) evidenceKashkouli MB, Abdolalizadeh P, Abolfathzadeh N, Sianati H, Sharepour M, Hadi Y. Periorbital facial rejuvenation; applied anatomy and pre-operative assessment. Journal of current ophthalmology. 2017 Sep:29(3):154-168. doi: 10.1016/j.joco.2017.04.001. Epub 2017 Apr 25 [PubMed PMID: 28913505]
Costin BR, Wyszynski PJ, Rubinstein TJ, Choudhary MM, Chundury RV, McBride JM, Levine MR, Perry JD. Frontalis Muscle Asymmetry and Lateral Landmarks. Ophthalmic plastic and reconstructive surgery. 2016 Jan-Feb:32(1):65-8. doi: 10.1097/IOP.0000000000000577. Epub [PubMed PMID: 26505231]
Lee EJ, Hwang K. Depressor muscle division through a subbrow excision for the improvement of brow ptosis. The Journal of craniofacial surgery. 2013 Nov:24(6):1987-90. doi: 10.1097/SCS.0b013e3182a28bc8. Epub [PubMed PMID: 24220387]
Level 3 (low-level) evidenceTakezawa K, Townsend G, Ghabriel M. The facial nerve: anatomy and associated disorders for oral health professionals. Odontology. 2018 Apr:106(2):103-116. doi: 10.1007/s10266-017-0330-5. Epub 2017 Dec 14 [PubMed PMID: 29243182]
Kearsey C, Fernando P, D'Costa D, Ferdinand P. The use of the ice pack test in myasthenia gravis. JRSM short reports. 2010 Jun 30:1(1):14. doi: 10.1258/shorts.2009.090037. Epub 2010 Jun 30 [PubMed PMID: 21103106]
Level 3 (low-level) evidenceXu S, Zhang Z, Tang X, Yin L, Liu W, Shi L. The influence of gender and laterality on the incidence of hemifacial microsomia. The Journal of craniofacial surgery. 2015 Mar:26(2):384-7. doi: 10.1097/SCS.0000000000001336. Epub [PubMed PMID: 25723655]
Wang S, Breskovska I, Gandhy S, Punga AR, Guptill JT, Kaminski HJ. Advances in autoimmune myasthenia gravis management. Expert review of neurotherapeutics. 2018 Jul:18(7):573-588. doi: 10.1080/14737175.2018.1491310. Epub 2018 Jul 4 [PubMed PMID: 29932785]
Level 3 (low-level) evidenceKarimi N, Kashkouli MB, Sianati H, Khademi B. Techniques of Eyebrow Lifting: A Narrative Review. Journal of ophthalmic & vision research. 2020 Apr-Jun:15(2):218-235. doi: 10.18502/jovr.v15i2.6740. Epub 2020 Apr 6 [PubMed PMID: 32308957]
Level 3 (low-level) evidencePitanguy I, Ramos AS. The frontal branch of the facial nerve: the importance of its variations in face lifting. Plastic and reconstructive surgery. 1966 Oct:38(4):352-6 [PubMed PMID: 5926990]
Apinhasmit W, Chompoopong S, Methathrathip D, Sansuk R, Phetphunphiphat W. Supraorbital Notch/Foramen, Infraorbital Foramen and Mental Foramen in Thais: anthropometric measurements and surgical relevance. Journal of the Medical Association of Thailand = Chotmaihet thangphaet. 2006 May:89(5):675-82 [PubMed PMID: 16756055]
Isse NG. Endoscopic facial rejuvenation: endoforehead, the functional lift. Case reports. Aesthetic plastic surgery. 1994 Winter:18(1):21-9 [PubMed PMID: 8122572]
Level 3 (low-level) evidenceTrinei FA, Januszkiewicz J, Nahai F. The sentinel vein: an important reference point for surgery in the temporal region. Plastic and reconstructive surgery. 1998 Jan:101(1):27-32 [PubMed PMID: 9427913]
Zins JE, Coombs DM. Endoscopic Brow Lift. Clinics in plastic surgery. 2022 Jul:49(3):357-363. doi: 10.1016/j.cps.2022.02.003. Epub [PubMed PMID: 35710151]
Raggio BS, Winters R. Endoscopic Brow Lift. StatPearls. 2025 Jan:(): [PubMed PMID: 31424804]
Perez PB, Gunter AE, Moody MP, Vincent AG, Perez CR, Serra RM, Hohman MH. Investigating Long-Term Brow Stabilization by Endotine-Assisted Endoscopic Brow Lift with Concomitant Upper Lid Blepharoplasty. The Annals of otology, rhinology, and laryngology. 2021 Oct:130(10):1139-1147. doi: 10.1177/0003489421997653. Epub 2021 Feb 25 [PubMed PMID: 33631951]
Viterbo F, Auersvald A, O'Daniel TG. Gliding Brow Lift (GBL): A New Concept. Aesthetic plastic surgery. 2019 Dec:43(6):1536-1546. doi: 10.1007/s00266-019-01486-3. Epub 2019 Sep 11 [PubMed PMID: 31511923]
Dutton JW Jr, Chang IA, Zins JE. The Hairline Brow Lift. Clinics in plastic surgery. 2022 Jul:49(3):349-356. doi: 10.1016/j.cps.2022.01.004. Epub 2022 May 13 [PubMed PMID: 35710150]
Dunn T, Hohman MH. Pretrichial Brow Lift. StatPearls. 2025 Jan:(): [PubMed PMID: 34033394]
Hohman MH, Teixeira J. Transgender Surgery of the Head and Neck. StatPearls. 2025 Jan:(): [PubMed PMID: 33760488]
Fakih-Gomez N, Martins L, Dagher E, Obeid PM, Guzmán-Velázquez YA, Muñoz-Gonzalez C. Deep Plane Direct Brow Lift. Aesthetic plastic surgery. 2025 May:49(9):2385-2398. doi: 10.1007/s00266-025-04775-2. Epub 2025 Mar 10 [PubMed PMID: 40064642]
Jawad BA, Raggio BS. Direct Brow Lift. StatPearls. 2025 Jan:(): [PubMed PMID: 32644687]
Patel BC, Malhotra R. Mid Forehead Brow Lift. StatPearls. 2025 Jan:(): [PubMed PMID: 30571073]
Balado AS, Stevens HP. Lateral Hooding of the Brow Revisited: Reverse Brow Lifting Versus the ROOF Lift. Aesthetic plastic surgery. 2020 Apr:44(2):630-632. doi: 10.1007/s00266-020-01631-3. Epub 2020 Feb 4 [PubMed PMID: 32020281]
Myung Y, Jung C. Mini-midface Lift Using Polydioxanone Cog Threads. Plastic and reconstructive surgery. Global open. 2020 Jun:8(6):e2920. doi: 10.1097/GOX.0000000000002920. Epub 2020 Jun 24 [PubMed PMID: 32766067]
Hong GW, Kim SB, Park SY, Wan J, Yi KH. Thread Lifting Materials: A Review of Its Difference in Terms of Technical and Mechanical Perspective. Clinical, cosmetic and investigational dermatology. 2024:17():999-1006. doi: 10.2147/CCID.S457352. Epub 2024 May 6 [PubMed PMID: 38737945]
Level 3 (low-level) evidenceBooth AJ, Murray A, Tyers AG. The direct brow lift: efficacy, complications, and patient satisfaction. The British journal of ophthalmology. 2004 May:88(5):688-91 [PubMed PMID: 15090424]
Level 2 (mid-level) evidence