Neuroanatomy, Cranial Nerve 11 (Accessory)
Neuroanatomy, Cranial Nerve 11 (Accessory)
Introduction
The spinal accessory nerve (SAN, 11th cranial nerve, CN XI) is essential for neck and shoulder movement, as it innervates the sternocleidomastoid (SCM) and trapezius muscles through its spinal root. CN XI also contributes indirectly to intrinsic laryngeal musculature function via its cranial component, which arises from the nucleus ambiguus and merges with the vagus nerve (CN X) to supply motor fibers to the larynx, pharynx, and soft palate. While the SAN is primarily a motor nerve, recent evidence suggests it contains minor sensory (nociceptive) fibers that may play a limited role in sensory afferents to the trapezius and SCM. However, these muscles receive most of their sensory innervation from cervical spinal nerves C2 to C4.
Minor injury can occur with daily movements or behaviors that exceed the elastic capacity of the SAN, such as excessive stretching or carrying heavy weights. However, the nerve may be severely damaged during neck tumor mass removal, particularly when the blood supply is compromised or partial resection is performed. In certain cases, removal of this nerve is accomplished to compensate for a peripheral nerve lesion, transfer it where electrical activity is absent, and attempt to restore limb function.[1][2] Understanding the anatomy and function of CN XI allows clinicians to prevent iatrogenic injury, accurately localize lesions, and implement targeted rehabilitation strategies to preserve or restore motor function.
Structure and Function
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Structure and Function
The SAN has a dual origin but always exits through the jugular foramen, which develops embryologically from the otic capsule and the baseplate. The nerve's spinal root arises from cervical spinal segments C1 to C5 (occasionally C6) and ascends into the skull through the foramen magnum, where it joins the cranial root. This segment then runs superolaterally along the floor of the posterior cranial fossa to enter the dural canal of the jugular foramen, joining small fibers emerging from the medulla and extending caudally to the region of the nucleus ambiguus.
From the jugular foramen, the SAN emerges with the vagus and glossopharyngeal nerves, as well as the sigmoid and inferior petrosal sinuses (see Image. Branches of the Glossopharyngeal, Vagus, and Spinal Accessory Nerves). Entering the jugular foramen are the occipital and pharyngeal meningeal arteries. Upon exiting, CN XI is encased in meningeal dura attached to the periosteum (see Image. Cranial Nerves and Dural Structures).
Once released from the dura, CN XI divides into internal and external branches. The internal branch contains fibers from the cranial portion, forming an anastomosis with the vagus nerve at the upper border of the transverse process of the 1st cervical vertebra (C1) and contributing parasympathetic fibers to the vagal innervation of the pharyngeal and laryngeal regions (see Image. Course of the Vagus Nerve). The external branch consists mainly of fibers from the spinal portion, which descend to innervate the trapezius and SCM (see Image. Hypoglossal, Vagus, and Glossopharyngeal Nerves in the Neck). These muscles also receive motor impulses from cervical nerves C1 to C4.
Cranial roots of the SAN are reportedly wider and more numerous on the right side, particularly in the male body, but confirmation requires further study. The external branch has a close relationship with the jugular vein, both within the jugular foramen and at its cervical exit, passing behind, in front of, or at the vein’s bifurcation.
Current scientific literature describes branches perforating the SCM and trapezius muscle. The nerve courses, with individual anatomical variations, near an imaginary horizontal line from the gonion toward the SCM, posterior to the muscle’s edge, and approximately 4 to 9 cm below the apex of the mastoid process. Another surface landmark is located in the trapezius muscle, approximately 2 to 9 cm above the clavicle toward the acromioclavicular joint.
Gray’s Anatomy describes an additional point slightly below the 1st branch. This point may be located by tracing an oblique line a few centimeters caudally, as the nerve runs obliquely beneath the SCM.
The intracranial portion of the SAN rests on the vertebral artery at its entry point and is in contact with the denticulate ligaments prior to exiting the jugular foramen. The rigidity of the vessel can influence nerve function, and traction on the cervical segment, whether muscular or vertebral, can also affect the nerve. Vascular calcification or other vasculopathies that stiffen the vessel’s connective tissue and reduce its adaptability are likely to diminish the nerve’s elasticity.
Trauma to the upper cervical region or poor posture can similarly impair nerve function. The number of myelinated fibers in CN XI ranges from 1,700 to 2,000, and the nerve diameter is approximately 2 mm. Recent cadaveric studies have confirmed these anatomical observations.[3]
CN XI primarily contracts the trapezius and SCM. However, the merging of this nerve with the vagus contributes to the motor innervation of intrinsic laryngeal muscles, enabling proper movement of the ipsilateral vocal cords. Additionally, recent research indicates that CN XI contains both motor and sensory components. Ganglia along the intracranial course of this nerve may have a nociceptive role, and these sensory cell bodies could contribute to myalgia of the trapezius and SCM.
Embryology
The SAN shares a common embryological origin with the vagus nerve, as both arise from the same ganglionic crest on the ectoderm. The structure contains motor and sensory components. As development progresses, the cranial termination becomes more sensory, whereas the caudal termination acquires predominantly motor functions.
At approximately 20 days of gestation, the ganglionic crest is lateralized and divided into right and left portions. The caudal portion produces a band of fibers that will become the future SAN, located at the level of the 4th, 5th, and 6th cervical spinal cord segments.
During the 4th week, the nerve separates from its connection with the vagus nerve and extends into a mesodermal mass that will form the SCM. By the end of the 5th week, the nerve lies medial to the dorsal rootlets and connects at irregular intervals to the developing spinal cord, making contact with the 1st spinal ganglion.
The cranial portion develops as a row of ganglia that, once formed, enlarge and connect with the jugular ganglion of the vagus nerve. The SAN elongates and assumes its definitive shape during the 2nd and 3rd months.
Blood Supply and Lymphatics
The proximal, distal, and recurrent branches of the posterior inferior cerebellar artery supply the intracranial portion of the SAN. The spinal roots receive blood supply from the musculospiral branch of the ascending pharyngeal artery and collateral branches of the anterior spinal artery. The occipital artery and branches of the lingual artery supply the extracranial portion. The nerve is accompanied by lymph nodes along its extracranial course through the posterior triangle of the neck. Small veins follow the entire nerve pathway and drain into the external jugular vein.
Nerves
The SAN anastomoses with the root of C1, though some authors report connections with C2 to C3. Other linkages include the stellate ganglion and glossopharyngeal nerve, whose functions have not been established. A branch of the great auricular nerve communicates with CN XI near the jugular foramen. At the upper border of the transverse process of the C1 vertebra, CN XI joins CN X via the Lobstein anastomosis.
Muscles
Along its course, the SAN contacts the levator scapulae muscle and remains superficial to the prevertebral fascia. Medial to the styloid process, the nerve passes in proximity to the stylohyoid and digastric muscles. The muscles directly supplied by CN XI are the trapezius and SCM, along with laryngeal musculature, through collaboration with CN X, such as the palatal, pharyngeal, and laryngeal muscles.
The trapezius and SCM have a branchiomeric origin, with afferent fibers from these muscles projecting to the nucleus of the solitary tract. The trapezius elevates, depresses, adducts, abducts, and externally rotates the scapula. This muscle extends the head while rotating it to the opposite side, and also extends, rotates, and laterally tilts the head. The muscle contributes indirectly to arm flexion and abduction by elevating the scapula beyond approximately 60°. The trapezius is essential for coordinated movement between the shoulder, arm, and neck.
Contraction of a single SCM produces ipsilateral head flexion with contralateral rotation, while bilateral activation extends the head. The SCM can also act as an accessory muscle of inspiration by using the temporal bone as a fixed point to elevate the sternum and clavicles.[4]
Physiologic Variants
Research on the SAN has revealed numerous unexpected variations, reflecting the evolving nature of anatomical knowledge. Cadaveric dissection studies have documented a substantial range of structural differences in this nerve's course, connections, and relationships with other cervical structures.
Root of the First Cervical Nerve
Four distinct intradural relationship patterns have been described between CN XI and the small roots of C1. In the 1st type, the posterior root is absent, and CN XI anastomoses with the anterior root. In the 2nd type, no connection exists between CN XI and the posterior root. The 3rd type features multiple anastomoses between CN XI and the posterior roots at different points. In the 4th type, CN XI connects to the posterior roots, but the latter lack a connection to the spinal cord.
Other variations in the course of CN XI occur in relation to other neck structures. A recent report describes a linkage between the 1st cervical root and CN XI via the McKenzie nerve. The McKenzie nerve may also connect CNs X and XI near the exit of the jugular foramen.[5]
Cadaveric studies have identified further variations, including duplication of the nerve both inside and outside the skull, the presence of macroganglia in the spinal portion of the intracranial segment, and a lesser occipital nerve with direct branching from CN XI. Communication between CN XI and the facial nerve has also been documented, involving shared motor supply to the SCM.[6]
Internal Jugular Vein
CN XI most often crosses ventral to the internal jugular vein, although it may also pass dorsal or lateral to the vein, or, less commonly, traverse through the vessel. Rarely, the SAN travels medial to the vein. In some cases, the nerve bifurcates near the vein, with branches passing both medially and laterally.
Sternocleidomastoid
CN XI courses along the deep surface of the SCM and may send branches without penetrating the muscle (type A), send a single nonpenetrating branch (type B), or penetrate the muscle deeply (type C). The trapezius muscle is rarely innervated solely by cervical spinal nerves. In rare instances within the cranium, CN XI may form an anastomosis with the facial nerve, resulting in shared innervation of the SCM. The cervical plexus, particularly via C2 and C3, can contribute to CN XI function.
Surgical Considerations
Iatrogenic Lesions
The course of CN XI makes it particularly vulnerable to iatrogenic injuries during procedures involving the posterior triangle of the neck. Palsy following internal jugular vein cannulation is an example. Carotid endarterectomy, cardiac or pulmonary surgery with sternotomy, radiation therapy, cervical lymph node biopsy, and thyroid surgery may produce similar healthcare-associated complications.[7][8][9]
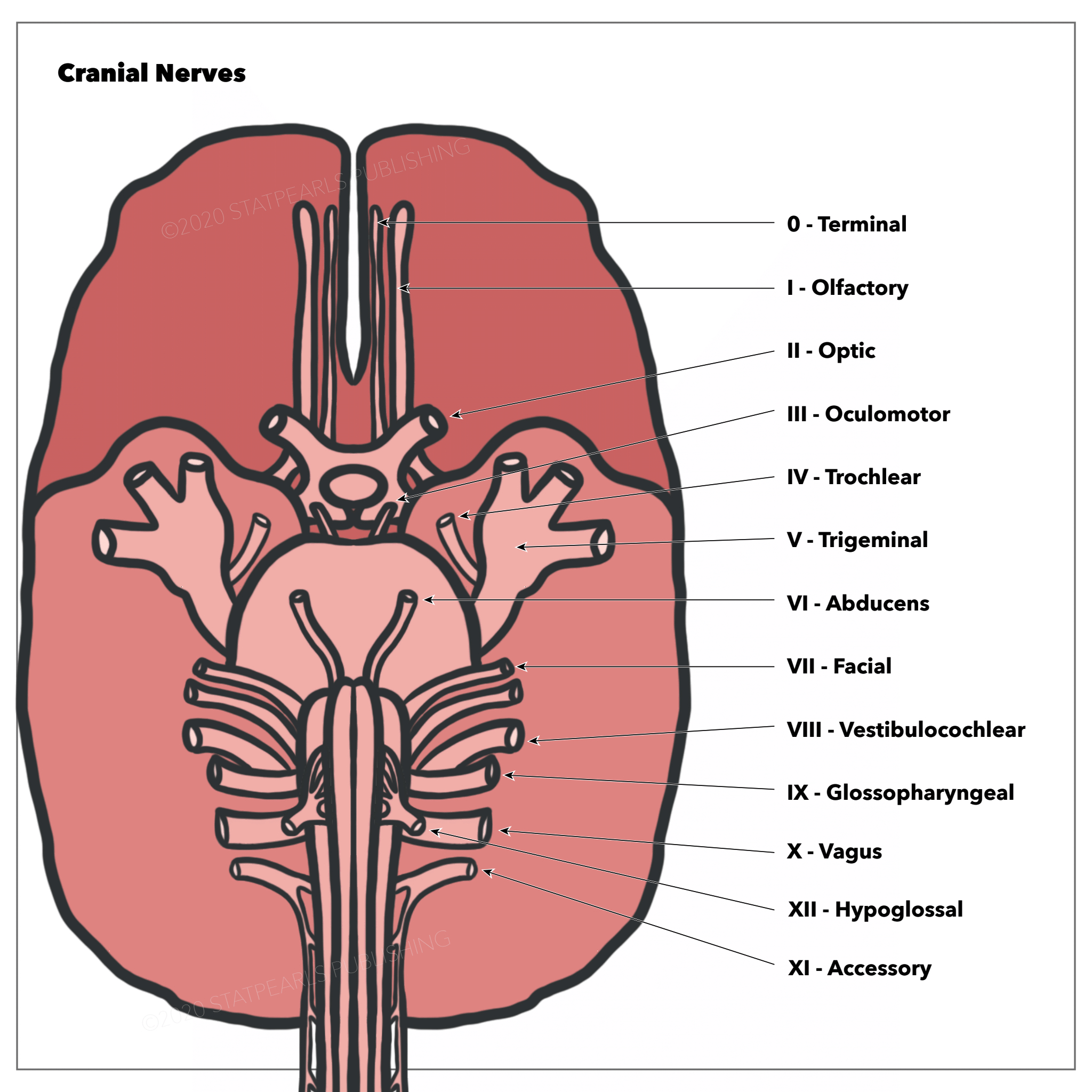
Direct Pathologies
Direct injuries involving CN XI are uncommon but typically cause trapezius and SCM dysfunction. These conditions may result from cervical lesions affecting the foramen magnum, jugular foramen, or intracranial area (see Image. Relationships of the Cranial Nerves to the Base of the Brain). Aneurysms of the internal carotid or posterior inferior cerebellar artery may cause permanent ischemic injury. Atlas or hyoid bone fractures can also compress the nerve.
Systemic Conditions
Several syndromes may impair CN XI function, including Collet-Sicard, Vernet, jugular foramen, Schmidt, Villaret, Garcin, Guillain-Barré (pharyngo-cervico-brachial variant), Sandifer, and Eagle syndromes. Rarely, infections such as diphtheria, poliomyelitis, and tetanus may also involve the nerve. Other systemic conditions that can produce CN XI dysfunction include botulism, sarcoidosis, diabetes, vitamin B12 deficiency, and tumors.
Nerve Transfer
CN XI may be used in neurotization and reinnervation procedures involving cervical plexus target nerves, such as the radial, suprascapular, musculocutaneous, and axillary nerves. In patients with quadriplegia, CN XI may be transferred to replace the phrenic nerve. Conversely, when CN XI is permanently damaged, reinnervation may be achieved using the upper trunk of the brachial plexus, particularly fascicles destined for the axillary nerve.
Clinical Significance
The strength and bulk of the trapezius and SCM are assessed during clinical evaluation for CN XI injury. Trapezius function is tested by asking the patient to elevate the shoulders with and without resistance. SCM function is evaluated by instructing the patient to rotate the head to either side against resistance. Muscle inspection may reveal atrophy or fasciculations.[10]
Trapezius dysfunction or paralysis is most often neurogenic, as CN XI is exposed along its superficial course in the posterior triangle of the neck. Injury may result from blunt trauma, such as in contact sports like football and hockey, or penetrating trauma, including gunshot wounds or deep lacerations from sharp objects or weapons.
Various degrees of dysfunction may arise from repetitive traction injuries or compression neuropathy. CN XI should be evaluated when scapular winging, abnormal or asymmetric neck rotational posture, trapezius atrophy, shoulder pain, or impaired shoulder abduction is suspected.
Strength and reflexes may be assessed using specific maneuvers. A small hammer may be applied to the clavicular insertion of the SCM to elicit its reflex. SCM strength is evaluated by having the patient rotate the head from side to side against resistance. Trapezius contraction is tested by placing the examiner’s hands at the base of the patient’s neck over the trapezius and asking the patient to elevate the shoulders.
Instrumental Evaluation
Several methods can investigate potential CN XI injury. Imaging options include x-ray (for the skull base and styloid process), video cinematography, computed tomography, magnetic resonance imaging, angiography, and ultrasound. Electrophysiological techniques such as electromyography (EMG), spinal nerve root electrical activation, and transcranial magnetic stimulation can help assess nerve function.
Lateral Scapular Winging
Trapezius paralysis secondary to CN XI injury causes the affected shoulder to droop, producing lateral scapular winging. Compared with the contralateral side, the scapula shows inferior translation, and the inferior angle rotates laterally. In subtle cases, the winging may be elicited by having the patient push against a wall with outstretched arms, allowing the examiner to observe the deformity more clearly.
Workup for lateral scapular winging begins with radiographs of the chest, cervical spine, shoulder, and scapula. EMG and nerve conduction studies serve as valuable adjuncts to support physical examination findings. Once confirmed, CN XI recovery may be monitored serially at 3- to 6-month intervals.
Other Issues
Physiotherapy
CN XI rehabilitation should include electrostimulation of the SCM and trapezius muscles. Specific exercises to actively engage these muscles, as well as proprioceptive exercises, should be incorporated.
Osteopathy
Osteopathic interventions may improve tissue mobility, particularly in the presence of scars. Such approaches may also help reduce pain or inflammatory markers, as suggested by studies involving other pathological conditions.
A randomized controlled trial demonstrated that EMG biofeedback targeting scapular motion in patients with oral cancer and concomitant CN XI dysfunction improved scapular and shoulder arthrokinematics.[11] A recent study of 26 patients with SAN injury showed that gentle manual therapy combined with physiotherapy improved muscle tone and kinematics in the region supplied by this nerve.[12] A case report described SAN palsy (drooping shoulder) secondary to chronic lymphocytic leukemia, an extremely rare occurrence. Early diagnosis made resolution possible.[13]
Media
(Click Image to Enlarge)

Cranial Nerves and Dural Structures. Sagittal section showing the meninges of the dura mater, its processes, and major dural venous sinuses, including the straight, inferior sagittal, and transverse sinuses. The tentorium cerebelli and diaphragma sellae are visible. Cranial nerves IX to XII are labeled, including the accessory nerve (9th cranial nerve, CN XI), along with CNs V to VIII, III, and IV. The great cerebral vein, ophthalmic artery, optic nerves, and olfactory tract are also depicted.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
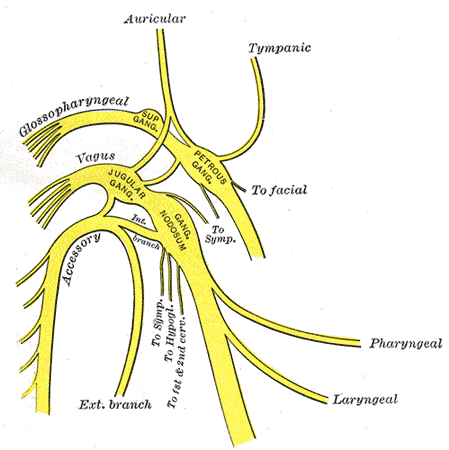
Branches of the Glossopharyngeal, Vagus, and Spinal Accessory Nerves. This diagram shows the major branches, ganglia, and connections of the glossopharyngeal, vagus, and spinal accessory nerves in relation to each other.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
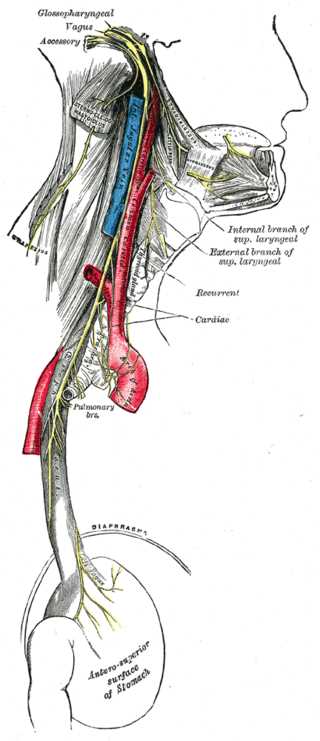
Course of the Vagus Nerve. This diagram shows the path of the vagus nerve as it travels from the neck through the thorax to the abdomen. The image highlights the vagus nerve coursing alongside the glossopharyngeal and spinal accessory nerves, as well as neighboring structures that include the carotid artery, esophagus, pulmonary branches, recurrent laryngeal nerves, diaphragm, and the anterior surface of the stomach.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
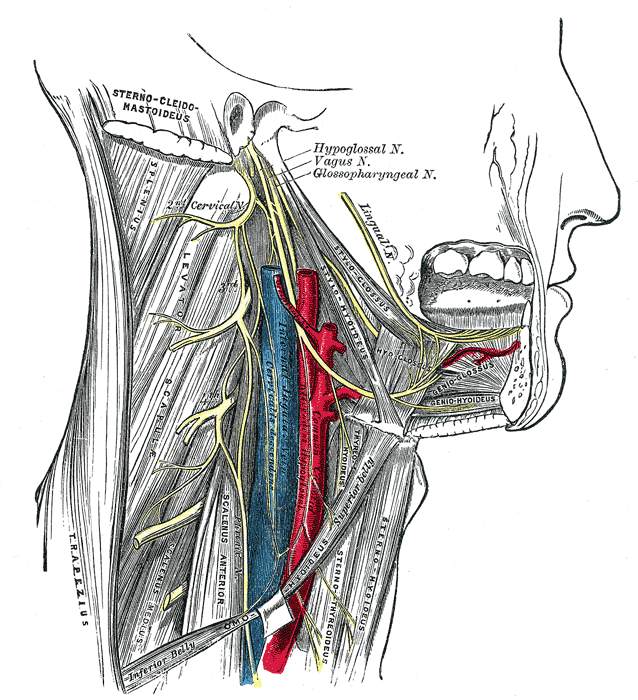
Hypoglossal, Vagus, and Glossopharyngeal Nerves in the Neck. This diagram shows the course of these cranial nerves in relation to the sternocleidomastoid, levator scapulae, scalenus anterior, geniohyoid, and stylohyoid muscles, as well as the cervical plexus, common carotid artery, and surrounding anatomical structures.
Henry Vandyke Carter, Public Domain, via Wikimedia Commons
(Click Image to Enlarge)
References
Singh O, Das JM. Anatomy, Head and Neck: Jugular Foramen. StatPearls. 2025 Jan:(): [PubMed PMID: 30860742]
Salandy S, Rai R, Gutierrez S, Ishak B, Tubbs RS. Neurological examination of the infant: A Comprehensive Review. Clinical anatomy (New York, N.Y.). 2019 Sep:32(6):770-777. doi: 10.1002/ca.23352. Epub 2019 Mar 8 [PubMed PMID: 30848525]
Roberts SO, Cardozo A. A detailed review of the spinal accessory nerve and its anatomical variations with cadaveric illustration. Anatomical science international. 2024 Jun:99(3):239-253. doi: 10.1007/s12565-024-00770-w. Epub 2024 May 2 [PubMed PMID: 38696101]
Svenberg Lind C, Lundberg B, Hammarstedt Nordenvall L, Heiwe S, Persson JK, Hydman J. Quantification of Trapezius Muscle Innervation During Neck Dissections: Cervical Plexus Versus the Spinal Accessory Nerve. The Annals of otology, rhinology, and laryngology. 2015 Nov:124(11):881-5. doi: 10.1177/0003489415589365. Epub 2015 Jun 1 [PubMed PMID: 26032955]
Carsky K, Iwanaga J, Clark M, Aysenne A, Tubbs RS. A Nerve of McKenzie With a Variant Communicating Branch Between the Vagus Nerve and Cranial Root of the Accessory Nerve: A Cadaveric Case Report. Cureus. 2021 Apr 7:13(4):e14343. doi: 10.7759/cureus.14343. Epub 2021 Apr 7 [PubMed PMID: 33972901]
Level 3 (low-level) evidenceTubbs RS, Ajayi OO, Fries FN, Spinner RJ, Oskouian RJ. Variations of the accessory nerve: anatomical study including previously undocumented findings-expanding our misunderstanding of this nerve. British journal of neurosurgery. 2017 Feb:31(1):113-115. doi: 10.1080/02688697.2016.1187253. Epub 2016 May 24 [PubMed PMID: 27216244]
Level 3 (low-level) evidenceBuño BO 2nd, Cruz FM. Neuro-ophthalmological presentation of giant intracavernous carotid artery aneurysm in a child. BMJ case reports. 2018 Nov 28:11(1):. doi: 10.1136/bcr-2018-225842. Epub 2018 Nov 28 [PubMed PMID: 30567093]
Level 3 (low-level) evidenceMayer JA, Hruby LA, Salminger S, Bodner G, Aszmann OC. Reconstruction of the spinal accessory nerve with selective fascicular nerve transfer of the upper trunk. Journal of neurosurgery. Spine. 2019 Jul 1:31(1):133-138. doi: 10.3171/2018.12.SPINE18498. Epub 2019 Apr 5 [PubMed PMID: 30952116]
Bhatnagar A. Spinal accessory nerve transfer to the suprascapular nerve to restore shoulder function in brachial plexus injury: Management nuances. Neurology India. 2019 Jan-Feb:67(Supplement):S29-S31. doi: 10.4103/0028-3886.250725. Epub [PubMed PMID: 30688229]
AlShareef S, Newton BW. Accessory Nerve Injury. StatPearls. 2025 Jan:(): [PubMed PMID: 30335278]
Chen YH, Liang WA, Lin CR, Huang CY. A randomized controlled trial of scapular exercises with electromyography biofeedback in oral cancer patients with accessory nerve dysfunction. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2022 Oct:30(10):8241-8250. doi: 10.1007/s00520-022-07263-4. Epub 2022 Jul 11 [PubMed PMID: 35821447]
Level 1 (high-level) evidenceSimsek F, Naci B, Kilicoglu MB, Alkan Z, Topcuoglu OM, Gormez A, Hafiz G, Okyar AF. Can Manual Therapy Alter Muscle Stiffness in Patients With Spinal Accessory Nerve Injury? Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2025 Jul:173(1):115-125. doi: 10.1002/ohn.1236. Epub 2025 Mar 24 [PubMed PMID: 40125732]
Al-Deerawi Z, Shaladi A, Borg AG, Stanislas M, Barrak H. Accessory Nerve Palsy as the Initial Manifestation of Chronic Lymphocytic Leukemia: A Case Report. The American journal of case reports. 2025 Jun 1:26():e948534. doi: 10.12659/AJCR.948534. Epub 2025 Jun 1 [PubMed PMID: 40450388]
Level 3 (low-level) evidence