Introduction
Excess body weight and obesity are significant risk factors for type 2 diabetes (T2D). Clinicians should manage obesity in patients with T2D by adhering to guidelines from the American Diabetes Association and the American Obesity Association, which recommend lifestyle modifications, pharmacological therapies, and surgical options. At the Second Diabetes Surgery Summit (2016), an international consensus conference, experts developed a treatment algorithm for metabolic and bariatric surgery in patients with obesity and diabetes.[1][2]
Issues of Concern
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Issues of Concern
The lifetime risk of developing diabetes in men aged 18 or older increases from 7% to 70% as the body mass index (BMI) increases from less than 18.5 kg/m2 to over 35 kg/m2. In women, the risk increases from 12% to 74% across the same BMI values.[3] Given this strong association, diabetes screening is recommended for all patients with obesity. Managing obesity is crucial for both the prevention and treatment of T2D. Weight loss leads to a significant reduction in the incidence of diabetes in at-risk populations. In a study, lifestyle modifications, including modest weight reduction (5%-10% of baseline weight) and at least 150 minutes of physical activity per week, led to over a 50% reduction in the incidence of diabetes.[4]
Similarly, bariatric surgery has been associated with a 5-fold reduction in T2D incidence over 7 years.[5] Weight loss is also effective in managing T2D. Glycemic control improves proportionally with weight loss, sometimes leading to remission.[6] Treatment of T2D begins with lifestyle management, followed by pharmacological therapy and surgery when necessary.
BMI is the most commonly used metric to assess body weight, and it is calculated by dividing a patient’s weight in kilograms by the square of their height in meters (kg/m2). BMI is used to classify individuals into the following categories:
- Underweight: <18.5 kg/m2
- Healthy weight: 18.5 to 24.9 kg/m2 (18.5-22.9 kg/m2 for Asian populations)
- Overweight: 25 to 29.9 kg/m2 (23-27.4 kg/m2 for Asian populations)
- Obese, class 1: 30 to 34.9 kg/m2 (27.5-32.4 kg/m2 for Asian populations)
- Obese, class 2: 35 to 39.9 kg/m2 (32.5-37.4 kg/m2 for Asian population)
- Obese, class 3: ≥40 kg/m2 (≥37.5 kg/m2 for Asian populations)
The upper BMI value in each category is lower for individuals of Asian descent due to their higher body fat percentage and increased risk of T2D at lower BMI levels. Many international organizations have adopted these adjusted ranges to more accurately define obesity in Asian populations.[7]
Lifestyle Management
Obesity is a chronic medical condition and a known risk factor for the development of T2D. In patients diagnosed with overweight or obesity and T2D, treatment should begin with intensive lifestyle modifications, which include:
- Self-management education for diabetes
- Nutritional counseling
- Increasing physical activity
- Psychosocial care, when indicated
- Smoking cessation for smokers [8]
Patient self-management education fosters a deeper understanding of coexisting chronic conditions and enhances knowledge about self-monitoring and adherence to medical treatment. Patient education begins at the time of diabetes diagnosis, continues annually, and is provided as needed when complications arise.[9] Interprofessional healthcare providers, including nurses, registered dietitians, primary care providers, and specialists, all play essential roles in patient education. Effective teaching methods include motivational interviewing, the use of visual aids, distributing handouts, and utilizing electronic resources to enhance learning.
The goal of lifestyle modification is to achieve at least a 5% weight loss, which is necessary to obtain meaningful health benefits.[10] The Look AHEAD trial offers extensive data on the impact of intensive lifestyle intervention (ILI), demonstrating sustained weight loss greater than 5% in over half of participants, with 27% achieving more than 10% weight loss at 8 years.[11]
Participants in the ILI group required fewer medications for diabetes, hypertension, and lipid management. A daily calorie deficit of 500 to 750 kcal is generally recommended to achieve weight loss. Typically, this results in a daily calorie goal of 1200 to 1500 kcal/d for women and 1500 to 1800 kcal/d for men. Meal replacement plans may help some individuals achieve a targeted calorie deficit, but they are generally not sustainable for long-term use. More sustainable and effective dietary approaches include the DASH (Dietary Approaches to Stop Hypertension) diet and the Mediterranean diet.[12][13]
Among intermittent fasting approaches, modified alternate-day fasting and the 5:2 diet are the only ones shown to produce statistically significant weight loss exceeding 5%.[14]
The chosen diet should be tailored to the patient's cultural and dietary patterns, food availability, and other factors such as hunger and access to healthy foods. Counseling sessions for nutrition, physical activity, and behavioral goals aimed at achieving weight loss should be available to all patients. Standard intensive ILI includes more than 16 sessions over 6 months, with monthly follow-ups for those who achieve target weight loss after 1 year. However, this level of ILI may not be easily accessible or financially feasible in primary care settings.
Individuals with T2D and obesity should be encouraged to gradually increase their physical activity. Most professional guidelines recommend at least 150 minutes of moderate-intensity exercise per week. The optimal plan combines aerobic exercise with 2 to 3 resistance training sessions weekly. Exercising daily or avoiding more than 2 consecutive days without activity helps reduce insulin resistance.[15]
Regular screening for mood disorders and other psychosocial factors associated with diabetes and obesity is essential.[16][17] Addressing coexisting mental health conditions can enhance treatment adherence and improve outcomes in patients with obesity and T2D.
Adolescents and adults with obesity and diabetes should be screened for tobacco use, including electronic cigarettes. Smoking is associated with an increased risk of developing diabetes, possibly by increasing insulin resistance.[18] Clinicians should offer counseling and consider appropriate pharmacological interventions to support smoking cessation.
Medical Evaluation and Treatment
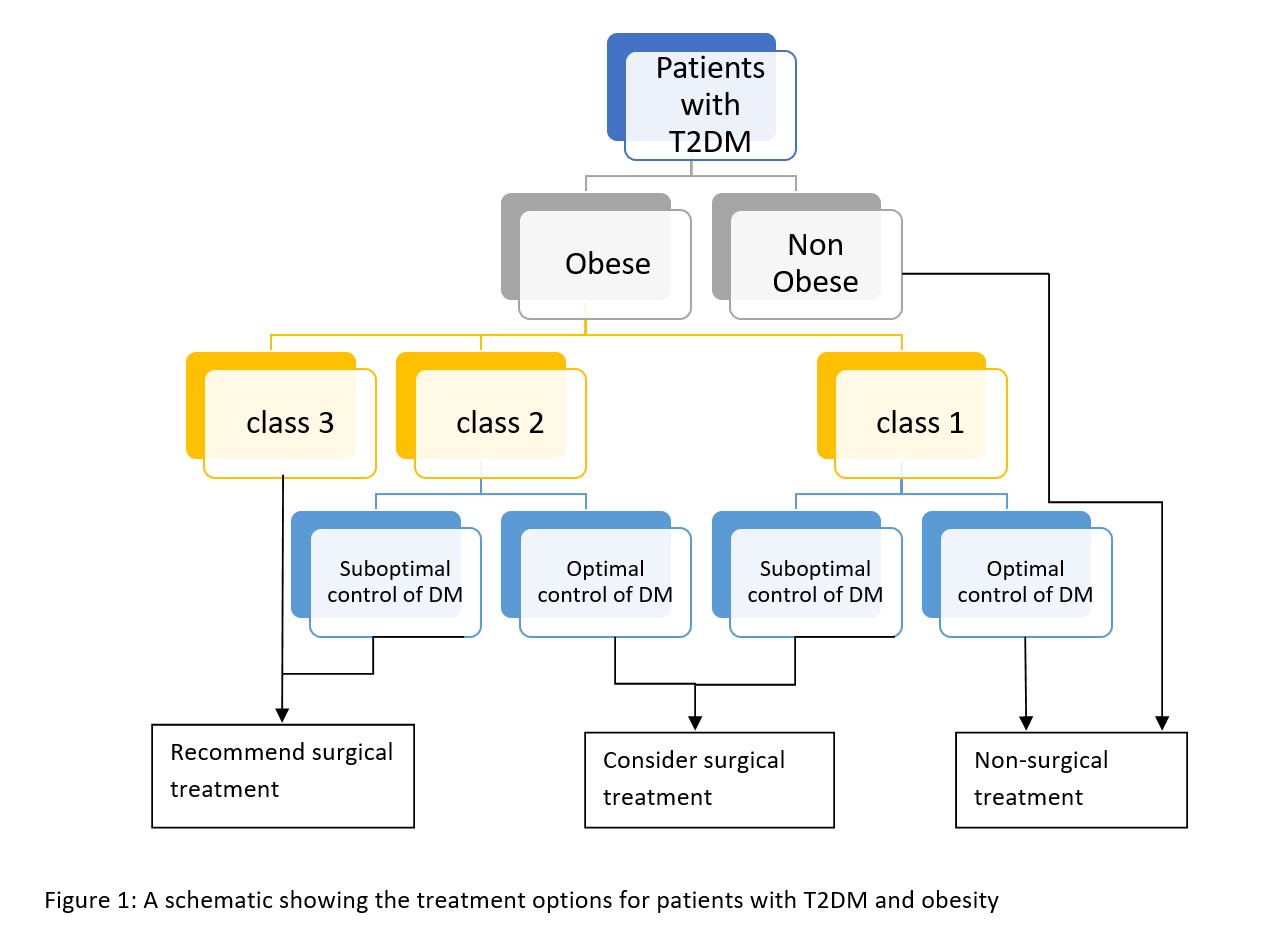
If lifestyle modifications do not result in adequate weight loss, clinicians should evaluate the patient’s medical history for contributing factors. This includes reviewing the use of obesogenic medications, such as thiazolidinediones, beta-blockers, sulfonylureas, insulin, antipsychotics, antidepressants, steroids, and gabapentin (see Image. A Schematic Overview of Treatment Options for Type 2 Diabetes and Obesity).
Pharmacotherapy is recommended as an adjunct to ILI for patients with a BMI over 30 kg/m2 (>25 kg/m2 in Asians) or over 27 kg/m2 (>23 kg/m2 in Asians) if they have a weight-related complication such as hypertension, dyslipidemia, T2D, or sleep apnea.[19]
After initiating therapy, clinicians should closely monitor patients for the efficacy of the medication and potential adverse effects. Early responders who lose at least 5% of their body weight within the first 12 weeks are more likely to achieve sustained and significant weight loss. Most weight loss medications are intended for long-term use. Although medical therapy for weight loss was initially studied for short-term use, evidence supporting long-term use has emerged over the past two decades. However, the United States Food and Drug Administration (FDA) has approved phentermine only for short-term use (<12 weeks) due to concerns about potential abuse.
FDA-Approved Medications for Long-Term Weight Management in Obesity and Type 2 Diabetes
Phentermine-topiramate, extended-release
This combination medication was approved by the FDA in 2012 and demonstrated an average weight loss of 10% in the SEQUEL trial, compared to less than 2% in the placebo arm.[20] The drug is effective for patients ranging from overweight to class 3 obesity, including those with a BMI of over 45 kg/m2. The initial dose consists of 3.75 mg of phentermine combined with 23 mg of extended-release (ER) topiramate (3.75 mg/23 mg). The dosage can be titrated up to 15 mg/92 mg in 2-week intervals as tolerated.
Common adverse effects include insomnia, increased blood pressure, dry mouth, and paresthesias. This medication should not be used concurrently with monoamine oxidase inhibitors. Because phentermine-topiramate is associated with an increased risk of congenital malformations such as cleft lip or cleft palate, clinicians must confirm that women of childbearing age are not pregnant and are using effective contraception before prescribing.
Liraglutide, semaglutide, and tirzepatide
Liraglutide and semaglutide are glucagon-like peptide-1 (GLP-1) receptor agonists, whereas tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. Although these agents were initially approved for the treatment of T2D, they have also demonstrated significant benefits for weight loss. They promote weight reduction through multiple mechanisms, including enhanced insulin secretion, improved insulin sensitivity, suppression of glucagon, delayed gastric emptying, and increased satiety via central nervous system effects. However, high cost and limited insurance coverage may restrict access to these medications.
Liraglutide, as studied in the SCALE trial, resulted in approximately 5% additional weight loss compared to the placebo.[21] The dosing starts at 0.6 mg daily, administered subcutaneously (SC), and is titrated weekly to a maximum of 3 mg daily SC. The most common adverse effects are gastrointestinal disturbances and nausea.
The STEP clinical trial evaluated semaglutide and demonstrated a 15% to 16% weight loss by week 68.[22] This medication achieves more substantial weight loss compared to semaglutide. The initial dose is 0.25 mg, administered SC once weekly, with gradual increases every 4 weeks up to a maximum dose of 2.4 mg weekly.
The SURMOUNT-2 trial evaluated tirzepatide for weight loss in individuals with T2D and a BMI of over 30 kg/m2 or over 27 kg/m2 with weight-related comorbidities, including T2D.[23] Tirzepatide’s dual mechanism—combining GLP-1 receptor agonism with glucose-dependent GIP activity—provided greater efficacy in glycemic control and weight reduction compared to GLP-1 receptor agonists alone. Approximately 20% weight loss was observed with the maximum 15 mg per week SC dose.
In the Phase III SURPASS trials, once-weekly SC tirzepatide, administered as monotherapy or as add-on therapy to oral glucose-lowering agents and insulin, demonstrated superiority over GLP-1 receptor agonists dulaglutide (0.75 mg) and semaglutide (1 mg).[24] The SURMOUNT-5 trial showed that among participants with obesity but without diabetes, tirzepatide also achieved significantly greater weight loss compared to semaglutide.[25]
Naltrexone-bupropion sustained release
This combination reduces food intake and promotes weight loss through multiple mechanisms. Naltrexone is an opioid antagonist, and bupropion is an antidepressant. The medication must be titrated gradually to minimize intolerance. The starting dose for naltrexone/bupropion is 1 tablet of 8 mg/90 mg daily, which may be increased to 2 tablets of 16 mg/180 mg twice daily as tolerated. This therapy is contraindicated in patients with uncontrolled hypertension, seizure disorders, or those receiving long-term opioid therapy.[26]
Orlistat
Orlistat is a pancreatic lipase inhibitor that prevents the absorption of fat. The medication is administered as a 60-mg tablet, taken 3 times daily with meals. The XENDOS trial demonstrated that treatment with orlistat resulted in approximately 5% weight loss.[27] Common adverse events include flatulence, abdominal pain, and fecal urgency, which can limit the usefulness or tolerability of this medication. Orlistat can also cause malabsorption of fat-soluble vitamins and increase the risk of cholelithiasis and nephrolithiasis.
Surgical Treatment
Surgical obesity treatment is indicated in patients with suboptimal weight loss or uncontrolled hyperglycemia. Surgery is recommended for patients with a BMI of over 40 kg/m2, or a BMI between 35 and 39.9 kg/m2 accompanied by hyperglycemia, weight-related comorbidities, or difficulty achieving sustainable weight loss. The Second Diabetes Surgery Summit reviewed evidence supporting surgery for patients with a BMI of 30 to 34.9 kg/m2.
Metabolic and bariatric surgery is a safe and effective treatment option and should be considered in diabetic patients with a BMI of 30 to 34.9 kg/m2 who exhibit uncontrolled hyperglycemia despite optimal medical therapy. Several surgical options are available for managing obesity, with the most common procedures including Roux-en-Y gastric bypass (RYGB), vertical sleeve gastrectomy (VSG), laparoscopic adjustable gastric banding (LAGB), and biliopancreatic diversion with duodenal switch (BPD).[2]
RYGB and VSG are the most frequently used techniques as they have better long-term outcomes and safety data. BPD is effective, but is associated with increased complications. LAGB is the safest procedure but carries the highest risk of requiring revision and re-intervention.
Surgery achieves beneficial outcomes by altering gastrointestinal anatomy to induce early satiety, reduce the absorptive surface area, and modulate hormones involved in glucose homeostasis.[28] Surgery also has a positive impact on intestinal glucose metabolism, and it alters pancreatic islet hormone activity, nutrient sensing, and bile acid metabolism.[29][30][31]
RYGB has been shown in multiple human trials to enhance insulin sensitivity. Furthermore, it increases adiponectin levels (an insulin-sensitizing hormone) and muscle insulin receptors, promoting muscle fatty acid metabolism, which in turn reduces lipid accumulation in muscle and liver, and improves insulin sensitivity.[28] Another study demonstrated that RYGB increases insulin secretion through both glucose-dependent and glucose-independent mechanisms.[29] Due to its significant metabolic effects, bariatric surgery is often referred to as metabolic surgery.
Extensive data support the role of bariatric procedures in controlling and, in many cases, preventing T2D.[32][33][34][35][36] Although most randomized controlled trials comparing surgical treatments with ILI have follow-up periods of 1 to 2 years, some have extended to 5 years.[37] The surgical group experienced an average reduction in hemoglobin A1c (HbA1c) of approximately 2%, compared to 0.5% in the conventional treatment group. Most surgical patients achieved an HbA1c of about 6%. Remission of T2D—defined as a nondiabetic HbA1c without medication—was also achieved in the majority. Sustained remission has been reported in 30% to 60% of patients across multiple studies with follow-up periods ranging from 1 to 5 years. However, the benefits may decline over time, particularly in patients with poor preoperative glycemic control, longer diabetes duration, or those who use insulin.[38]
Relapse of T2D occurred in 35% to 50% of patients. In the same study, RYGB was associated with a median disease-free period of 8.3 years. Surgical treatment improves glycemic control and clinical outcomes, even when remission is not achieved. One observational study with a 10- to 20-year follow-up reported significantly fewer complications and higher remission rates in the surgical group.[39]
RYGB and BPD result in the most significant reductions in HbA1c and BMI. Multiple studies have evaluated patients with a BMI of 30 to 35 kg/m2 and uncontrolled T2D, consistently showing improved HbA1c levels and higher remission rates in patients following surgery.[35][40][41][34] LAGB has demonstrated even better outcomes in patients with T2D and a BMI of 25 to 30 kg/m2.[42]
Researchers have examined the economic impact of bariatric procedures on patients with T2D. The cost per quality-adjusted life-year (QALY) for metabolic surgery typically ranges from $3200 to $6300, which is well below the $50,000 estimate for nonsurgical care.[2] A 15-year follow-up of the Swedish Obese Subjects (SOS) study found no significant difference in total healthcare costs between patients with obesity and T2D treated conventionally or with bariatric surgery.[43]
Metabolic surgery has become significantly safer and more effective over the past 2 decades, although outcomes are highly dependent on the surgeon's expertise. Mortality rates are low, ranging from 0.1% to 0.5%. Nonetheless, surgeons must thoroughly discuss potential risks and complications as part of informed consent and shared decision-making.[2][44] Reoperation and readmission rates are 2.5% and 5.1% for RYGB, 0.6% and 5.5% for VSG, and 0.6% and 2% for LAGB, respectively.[45]
Long-term follow-up demonstrates that LAGB has the highest rates of removal or revision. Although VSG is a relatively new procedure, its popularity has increased as surgical experience has improved. BPD is the most complex procedure and carries higher risks of mortality, morbidity, and complications. Clinicians should educate all bariatric surgery patients about the potential for postoperative nutritional deficiencies, such as iron deficiency anemia, hypoglycemia, and bone demineralization, and closely monitor them for both short-term and long-term complications.
Clinical Significance
Many healthcare quality metrics assess the effectiveness of diabetes prevention and treatment. Obesity is a major risk factor for T2D, influencing both its development and severity. Early screening of patients with obesity, combined with intensive treatment, can lead to long-term improvement or remission. Strict diabetes control reduces complications such as ketoacidosis, diabetic ulcers, amputations, soft tissue infections, and osteomyelitis. Additionally, aggressive management of HbA1c lowers the risk of coronary artery disease and chronic kidney disease.
Enhancing Healthcare Team Outcomes
Diabetes is a chronic, disabling illness, and the ongoing obesity epidemic is driving its increasing incidence. Treating obesity is crucial for both preventing and managing T2D, with successful outcomes relying on coordinated, interprofessional care among healthcare providers. Early identification of patients with obesity in primary care is a crucial first step in achieving optimal clinical outcomes.
Nurses are often the first point of contact, and they should accurately measure height and weight, calculate the BMI, and document these measurements consistently. Nursing staff should also review dietary habits and physical activity at baseline and during each follow-up visit. Patients with an elevated BMI are at an increased risk for T2D and should be informed of their BMI category during treatment discussions. Clinicians should support patients in setting individualized weight loss goals, ideally aiming for at least a 10% reduction in body weight to achieve meaningful metabolic improvements. Intensive lifestyle interventions and pharmacotherapy should be initiated in accordance with current clinical guidelines.
Suboptimal glycemic control should be evaluated and managed at every visit. Inadequate weight loss (defined as less than 10%) and ongoing hyperglycemia should prompt referral to an obesity medicine specialist or bariatric surgeon for further evaluation and treatment. Physicians, surgeons, and other clinicians often collaborate in multidisciplinary weight loss programs. Obesity medicine physicians help patients in achieving the target weights needed for surgical eligibility. They also play a critical role postoperatively by identifying complications and supporting healthy behaviors to maintain ongoing weight loss. Although many patients are ineligible for metabolic surgery due to operative risks from advanced cardiac or pulmonary disease, obesity medicine teams can still achieve positive outcomes for this population.
Registered dietitians, nutritionists, and therapists are essential members of the healthcare team, providing regular sessions to support optimal nutrition and physical activity. These healthcare teams may be led by trained professionals such as dietitians, therapists, nurses, physicians, or surgeons. Endocrinology consultations can offer additional strategies for managing persistent hyperglycemia. High-risk patients may require preoperative assessments by cardiologists or pulmonologists, and procedures should be performed in centers with on-site cardiac and pulmonary critical care. Pharmacists play a vital role in adjusting medication dosages, particularly in the perioperative period, as many drugs require weight-based dosing modifications after surgery.
The anesthesia team conducts preoperative evaluations and manages anesthesia-related events during and after metabolic procedures. Physical therapists assist patients with muscle strengthening in the postoperative period. Given the common association between obesity and mental health conditions, such as anxiety, depression, and body image disorders, psychiatry or psychology consultations should be considered when indicated.
Obesity and type 2 diabetes are chronic, systemic conditions that require a coordinated interprofessional approach for effective prevention and management. Members of the interprofessional healthcare team should support patients during their evaluation and treatment, providing them with ample resources and guidance to help them make informed decisions and achieve the best possible clinical outcomes.
Nursing, Allied Health, and Interprofessional Team Interventions
Interprofessional interventions focus on identifying T2D in patients with obesity. Providers should be aware of medications that contribute to weight gain and consider appropriate alternatives. Nurses record BMI at each visit and notify the provider when the value exceeds 25 kg/m2. Patients meeting this threshold are screened for T2D if they have not been previously tested. Primary care clinicians initiate lifestyle interventions for all patients with a BMI of 25 kg/m2 or higher. Standard written instructions about diet and exercise are reviewed at each visit.
Clinicians assist patients in setting realistic, measurable weight loss goals, aiming for a BMI below 25 kg/m2 or a 5% to 10% weight loss. A BMI over 30 kg/m2 alerts providers to consider ILI and pharmacological treatments. Registered dietitians and nutritionists provide patients with knowledge to make informed, healthy dietary choices. Effective outcomes rely on an interprofessional approach with clear communication between primary care providers and endocrinologists. When ILI and pharmacotherapy do not achieve adequate diabetes control and weight loss, timely referral to bariatric and metabolic surgeons is crucial for optimal care.
Nursing, Allied Health, and Interprofessional Team Monitoring
Members of the interprofessional team caring for patients with diabetes and obesity monitor HbA1c, body weight, BMI, and lifestyle changes at every visit. Clinicians educate patients about potential medication adverse effects and adjust doses as needed, whereas pharmacists reinforce this counseling and manage medication reconciliation.
After metabolic surgery, patients require close monitoring by the healthcare team. Although surgical patients require fewer medications because of improved metabolic parameters, there is a higher risk of hypoglycemia. Nurses identify and document complications such as wound dehiscence, perforation, and signs of infection, and promptly alert healthcare providers. Clinicians, dietitians, and nutritionists assess for signs of metabolic derangements, including vitamin and mineral deficiencies or malabsorption syndromes. Avoiding continuous use of nonsteroidal anti-inflammatory drugs during the first month helps prevent erosion of anastomosis sites. Internal quality metrics evaluate remission rates, procedural safety, postoperative recovery, and long-term outcomes after surgery.
Obesity increases the risk of T2D, cardiovascular disease, and numerous other chronic health conditions. Effective healthcare teams routinely screen for obesity and diabetes, using BMI to assess the severity of obesity. ILI and pharmacological therapy aim for at least 10% weight loss. Patients who do not achieve adequate weight loss or glycemic control despite optimal medical treatment should be referred for bariatric surgery. Over the past two decades, these procedures have become increasingly safe and effective. Continued postoperative monitoring by the interprofessional team is essential for early detection of complications and sustained clinical improvement.
Media
(Click Image to Enlarge)
References
Cohen RV, Shikora S, Petry T, Caravatto PP, Le Roux CW. The Diabetes Surgery Summit II Guidelines: a Disease-Based Clinical Recommendation. Obesity surgery. 2016 Aug:26(8):1989-91. doi: 10.1007/s11695-016-2237-6. Epub [PubMed PMID: 27189354]
Rubino F, Nathan DM, Eckel RH, Schauer PR, Alberti KG, Zimmet PZ, Del Prato S, Ji L, Sadikot SM, Herman WH, Amiel SA, Kaplan LM, Taroncher-Oldenburg G, Cummings DE, Delegates of the 2nd Diabetes Surgery Summit. Metabolic Surgery in the Treatment Algorithm for Type 2 Diabetes: A Joint Statement by International Diabetes Organizations. Diabetes care. 2016 Jun:39(6):861-77. doi: 10.2337/dc16-0236. Epub [PubMed PMID: 27222544]
Narayan KM, Boyle JP, Thompson TJ, Gregg EW, Williamson DF. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes care. 2007 Jun:30(6):1562-6 [PubMed PMID: 17372155]
Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM, Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 2002 Feb 7:346(6):393-403 [PubMed PMID: 11832527]
Level 1 (high-level) evidenceBooth H, Khan O, Prevost T, Reddy M, Dregan A, Charlton J, Ashworth M, Rudisill C, Littlejohns P, Gulliford MC. Incidence of type 2 diabetes after bariatric surgery: population-based matched cohort study. The lancet. Diabetes & endocrinology. 2014 Dec:2(12):963-8 [PubMed PMID: 25466723]
Level 2 (mid-level) evidenceKahan S, Fujioka K. Obesity Pharmacotherapy in Patients With Type 2 Diabetes. Diabetes spectrum : a publication of the American Diabetes Association. 2017 Nov:30(4):250-257. doi: 10.2337/ds17-0044. Epub [PubMed PMID: 29151715]
Misra A. Ethnic-Specific Criteria for Classification of Body Mass Index: A Perspective for Asian Indians and American Diabetes Association Position Statement. Diabetes technology & therapeutics. 2015 Sep:17(9):667-71. doi: 10.1089/dia.2015.0007. Epub 2015 Apr 22 [PubMed PMID: 25902357]
Level 3 (low-level) evidencePowers MA, Bardsley JK, Cypress M, Funnell MM, Harms D, Hess-Fischl A, Hooks B, Isaacs D, Mandel ED, Maryniuk MD, Norton A, Rinker J, Siminerio LM, Uelmen S. Diabetes Self-management Education and Support in Adults With Type 2 Diabetes: A Consensus Report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes care. 2020 Jul:43(7):1636-1649. doi: 10.2337/dci20-0023. Epub 2020 Jun 8 [PubMed PMID: 32513817]
Level 3 (low-level) evidenceAmerican Diabetes Association. 5. Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2021. Diabetes care. 2021 Jan:44(Suppl 1):S53-S72. doi: 10.2337/dc21-S005. Epub [PubMed PMID: 33298416]
Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. Journal of the Academy of Nutrition and Dietetics. 2015 Sep:115(9):1447-63. doi: 10.1016/j.jand.2015.02.031. Epub 2015 Apr 29 [PubMed PMID: 25935570]
Level 1 (high-level) evidenceLook AHEAD Research Group. Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring, Md.). 2014 Jan:22(1):5-13. doi: 10.1002/oby.20662. Epub [PubMed PMID: 24307184]
Level 1 (high-level) evidenceAzadbakht L, Fard NR, Karimi M, Baghaei MH, Surkan PJ, Rahimi M, Esmaillzadeh A, Willett WC. Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes care. 2011 Jan:34(1):55-7. doi: 10.2337/dc10-0676. Epub 2010 Sep 15 [PubMed PMID: 20843978]
Level 1 (high-level) evidenceD'Innocenzo S, Biagi C, Lanari M. Obesity and the Mediterranean Diet: A Review of Evidence of the Role and Sustainability of the Mediterranean Diet. Nutrients. 2019 Jun 9:11(6):. doi: 10.3390/nu11061306. Epub 2019 Jun 9 [PubMed PMID: 31181836]
Patikorn C, Roubal K, Veettil SK, Chandran V, Pham T, Lee YY, Giovannucci EL, Varady KA, Chaiyakunapruk N. Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-analyses of Randomized Clinical Trials. JAMA network open. 2021 Dec 1:4(12):e2139558. doi: 10.1001/jamanetworkopen.2021.39558. Epub 2021 Dec 1 [PubMed PMID: 34919135]
Level 1 (high-level) evidenceLittle JP, Gillen JB, Percival ME, Safdar A, Tarnopolsky MA, Punthakee Z, Jung ME, Gibala MJ. Low-volume high-intensity interval training reduces hyperglycemia and increases muscle mitochondrial capacity in patients with type 2 diabetes. Journal of applied physiology (Bethesda, Md. : 1985). 2011 Dec:111(6):1554-60. doi: 10.1152/japplphysiol.00921.2011. Epub 2011 Aug 25 [PubMed PMID: 21868679]
Level 3 (low-level) evidenceKulzer B, Albus C, Herpertz S, Kruse J, Lange K, Lederbogen F, Petrak F. Psychosocial Factors and Diabetes. Experimental and clinical endocrinology & diabetes : official journal, German Society of Endocrinology [and] German Diabetes Association. 2023 Feb:131(1-02):94-109. doi: 10.1055/a-1946-3863. Epub 2023 Feb 2 [PubMed PMID: 36731492]
Annesi JJ. Moderation of Mood in the Transfer of Self-Regulation From an Exercise to an Eating Context: Short- and Long-Term Effects on Dietary Change and Obesity in Women. International journal of behavioral medicine. 2019 Jun:26(3):323-328. doi: 10.1007/s12529-019-09772-9. Epub [PubMed PMID: 30734155]
Maddatu J, Anderson-Baucum E, Evans-Molina C. Smoking and the risk of type 2 diabetes. Translational research : the journal of laboratory and clinical medicine. 2017 Jun:184():101-107. doi: 10.1016/j.trsl.2017.02.004. Epub 2017 Mar 6 [PubMed PMID: 28336465]
Son JW, Kim S. Comprehensive Review of Current and Upcoming Anti-Obesity Drugs. Diabetes & metabolism journal. 2020 Dec:44(6):802-818. doi: 10.4093/dmj.2020.0258. Epub 2020 Dec 23 [PubMed PMID: 33389955]
Garvey WT, Ryan DH, Look M, Gadde KM, Allison DB, Peterson CA, Schwiers M, Day WW, Bowden CH. Two-year sustained weight loss and metabolic benefits with controlled-release phentermine/topiramate in obese and overweight adults (SEQUEL): a randomized, placebo-controlled, phase 3 extension study. The American journal of clinical nutrition. 2012 Feb:95(2):297-308. doi: 10.3945/ajcn.111.024927. Epub 2011 Dec 7 [PubMed PMID: 22158731]
Level 1 (high-level) evidenceDavies MJ, Bergenstal R, Bode B, Kushner RF, Lewin A, Skjøth TV, Andreasen AH, Jensen CB, DeFronzo RA, NN8022-1922 Study Group. Efficacy of Liraglutide for Weight Loss Among Patients With Type 2 Diabetes: The SCALE Diabetes Randomized Clinical Trial. JAMA. 2015 Aug 18:314(7):687-99. doi: 10.1001/jama.2015.9676. Epub [PubMed PMID: 26284720]
Level 1 (high-level) evidenceWilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, McGowan BM, Rosenstock J, Tran MTD, Wadden TA, Wharton S, Yokote K, Zeuthen N, Kushner RF, STEP 1 Study Group. Once-Weekly Semaglutide in Adults with Overweight or Obesity. The New England journal of medicine. 2021 Mar 18:384(11):989-1002. doi: 10.1056/NEJMoa2032183. Epub 2021 Feb 10 [PubMed PMID: 33567185]
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, Kiyosue A, Zhang S, Liu B, Bunck MC, Stefanski A, SURMOUNT-1 Investigators. Tirzepatide Once Weekly for the Treatment of Obesity. The New England journal of medicine. 2022 Jul 21:387(3):205-216. doi: 10.1056/NEJMoa2206038. Epub 2022 Jun 4 [PubMed PMID: 35658024]
France NL, Syed YY. Tirzepatide: A Review in Type 2 Diabetes. Drugs. 2024 Feb:84(2):227-238. doi: 10.1007/s40265-023-01992-4. Epub 2024 Feb 23 [PubMed PMID: 38388874]
Aronne LJ, Horn DB, le Roux CW, Ho W, Falcon BL, Gomez Valderas E, Das S, Lee CJ, Glass LC, Senyucel C, Dunn JP, SURMOUNT-5 Trial Investigators. Tirzepatide as Compared with Semaglutide for the Treatment of Obesity. The New England journal of medicine. 2025 May 11:():. doi: 10.1056/NEJMoa2416394. Epub 2025 May 11 [PubMed PMID: 40353578]
Grunvald E, Shah R, Hernaez R, Chandar AK, Pickett-Blakely O, Teigen LM, Harindhanavudhi T, Sultan S, Singh S, Davitkov P, AGA Clinical Guidelines Committee. AGA Clinical Practice Guideline on Pharmacological Interventions for Adults With Obesity. Gastroenterology. 2022 Nov:163(5):1198-1225. doi: 10.1053/j.gastro.2022.08.045. Epub 2022 Oct 20 [PubMed PMID: 36273831]
Level 1 (high-level) evidenceTorgerson JS, Hauptman J, Boldrin MN, Sjöström L. XENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patients. Diabetes care. 2004 Jan:27(1):155-61 [PubMed PMID: 14693982]
Level 1 (high-level) evidenceThaler JP, Cummings DE. Minireview: Hormonal and metabolic mechanisms of diabetes remission after gastrointestinal surgery. Endocrinology. 2009 Jun:150(6):2518-25. doi: 10.1210/en.2009-0367. Epub 2009 Apr 16 [PubMed PMID: 19372197]
Salehi M, Woods SC, D'Alessio DA. Gastric bypass alters both glucose-dependent and glucose-independent regulation of islet hormone secretion. Obesity (Silver Spring, Md.). 2015 Oct:23(10):2046-52. doi: 10.1002/oby.21186. Epub 2015 Aug 28 [PubMed PMID: 26316298]
Tremaroli V, Karlsson F, Werling M, Ståhlman M, Kovatcheva-Datchary P, Olbers T, Fändriks L, le Roux CW, Nielsen J, Bäckhed F. Roux-en-Y Gastric Bypass and Vertical Banded Gastroplasty Induce Long-Term Changes on the Human Gut Microbiome Contributing to Fat Mass Regulation. Cell metabolism. 2015 Aug 4:22(2):228-38. doi: 10.1016/j.cmet.2015.07.009. Epub [PubMed PMID: 26244932]
Breen DM, Rasmussen BA, Kokorovic A, Wang R, Cheung GW, Lam TK. Jejunal nutrient sensing is required for duodenal-jejunal bypass surgery to rapidly lower glucose concentrations in uncontrolled diabetes. Nature medicine. 2012 Jun:18(6):950-5. doi: 10.1038/nm.2745. Epub [PubMed PMID: 22610279]
Level 3 (low-level) evidenceMingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Leccesi L, Nanni G, Pomp A, Castagneto M, Ghirlanda G, Rubino F. Bariatric surgery versus conventional medical therapy for type 2 diabetes. The New England journal of medicine. 2012 Apr 26:366(17):1577-85. doi: 10.1056/NEJMoa1200111. Epub 2012 Mar 26 [PubMed PMID: 22449317]
Level 1 (high-level) evidenceSchauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, Thomas S, Abood B, Nissen SE, Bhatt DL. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. The New England journal of medicine. 2012 Apr 26:366(17):1567-76. doi: 10.1056/NEJMoa1200225. Epub 2012 Mar 26 [PubMed PMID: 22449319]
Level 1 (high-level) evidenceIkramuddin S, Korner J, Lee WJ, Connett JE, Inabnet WB, Billington CJ, Thomas AJ, Leslie DB, Chong K, Jeffery RW, Ahmed L, Vella A, Chuang LM, Bessler M, Sarr MG, Swain JM, Laqua P, Jensen MD, Bantle JP. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA. 2013 Jun 5:309(21):2240-9. doi: 10.1001/jama.2013.5835. Epub [PubMed PMID: 23736733]
Level 1 (high-level) evidenceParikh M, Chung M, Sheth S, McMacken M, Zahra T, Saunders JK, Ude-Welcome A, Dunn V, Ogedegbe G, Schmidt AM, Pachter HL. Randomized pilot trial of bariatric surgery versus intensive medical weight management on diabetes remission in type 2 diabetic patients who do NOT meet NIH criteria for surgery and the role of soluble RAGE as a novel biomarker of success. Annals of surgery. 2014 Oct:260(4):617-22; discussion 622-4. doi: 10.1097/SLA.0000000000000919. Epub [PubMed PMID: 25203878]
Level 3 (low-level) evidenceDing SA, Simonson DC, Wewalka M, Halperin F, Foster K, Goebel-Fabbri A, Hamdy O, Clancy K, Lautz D, Vernon A, Goldfine AB. Adjustable Gastric Band Surgery or Medical Management in Patients With Type 2 Diabetes: A Randomized Clinical Trial. The Journal of clinical endocrinology and metabolism. 2015 Jul:100(7):2546-56. doi: 10.1210/jc.2015-1443. Epub 2015 Apr 24 [PubMed PMID: 25909333]
Level 1 (high-level) evidenceMingrone G, Panunzi S, De Gaetano A, Guidone C, Iaconelli A, Nanni G, Castagneto M, Bornstein S, Rubino F. Bariatric-metabolic surgery versus conventional medical treatment in obese patients with type 2 diabetes: 5 year follow-up of an open-label, single-centre, randomised controlled trial. Lancet (London, England). 2015 Sep 5:386(9997):964-73. doi: 10.1016/S0140-6736(15)00075-6. Epub [PubMed PMID: 26369473]
Level 1 (high-level) evidenceArterburn DE, Bogart A, Sherwood NE, Sidney S, Coleman KJ, Haneuse S, O'Connor PJ, Theis MK, Campos GM, McCulloch D, Selby J. A multisite study of long-term remission and relapse of type 2 diabetes mellitus following gastric bypass. Obesity surgery. 2013 Jan:23(1):93-102. doi: 10.1007/s11695-012-0802-1. Epub [PubMed PMID: 23161525]
Level 2 (mid-level) evidenceSjöström L, Peltonen M, Jacobson P, Ahlin S, Andersson-Assarsson J, Anveden Å, Bouchard C, Carlsson B, Karason K, Lönroth H, Näslund I, Sjöström E, Taube M, Wedel H, Svensson PA, Sjöholm K, Carlsson LM. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014 Jun 11:311(22):2297-304. doi: 10.1001/jama.2014.5988. Epub [PubMed PMID: 24915261]
Level 2 (mid-level) evidenceLiang Z, Wu Q, Chen B, Yu P, Zhao H, Ouyang X. Effect of laparoscopic Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus with hypertension: a randomized controlled trial. Diabetes research and clinical practice. 2013 Jul:101(1):50-6. doi: 10.1016/j.diabres.2013.04.005. Epub 2013 May 22 [PubMed PMID: 23706413]
Level 1 (high-level) evidenceCourcoulas AP, Goodpaster BH, Eagleton JK, Belle SH, Kalarchian MA, Lang W, Toledo FG, Jakicic JM. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA surgery. 2014 Jul:149(7):707-15. doi: 10.1001/jamasurg.2014.467. Epub [PubMed PMID: 24899268]
Level 1 (high-level) evidenceWentworth JM, Playfair J, Laurie C, Ritchie ME, Brown WA, Burton P, Shaw JE, O'Brien PE. Multidisciplinary diabetes care with and without bariatric surgery in overweight people: a randomised controlled trial. The lancet. Diabetes & endocrinology. 2014 Jul:2(7):545-52. doi: 10.1016/S2213-8587(14)70066-X. Epub 2014 Apr 7 [PubMed PMID: 24731535]
Level 1 (high-level) evidenceKeating C, Neovius M, Sjöholm K, Peltonen M, Narbro K, Eriksson JK, Sjöström L, Carlsson LM. Health-care costs over 15 years after bariatric surgery for patients with different baseline glucose status: results from the Swedish Obese Subjects study. The lancet. Diabetes & endocrinology. 2015 Nov:3(11):855-65. doi: 10.1016/S2213-8587(15)00290-9. Epub 2015 Sep 17 [PubMed PMID: 26386667]
Aminian A, Brethauer SA, Kirwan JP, Kashyap SR, Burguera B, Schauer PR. How safe is metabolic/diabetes surgery? Diabetes, obesity & metabolism. 2015 Feb:17(2):198-201. doi: 10.1111/dom.12405. Epub 2014 Nov 19 [PubMed PMID: 25352176]
Birkmeyer NJ, Dimick JB, Share D, Hawasli A, English WJ, Genaw J, Finks JF, Carlin AM, Birkmeyer JD, Michigan Bariatric Surgery Collaborative. Hospital complication rates with bariatric surgery in Michigan. JAMA. 2010 Jul 28:304(4):435-42. doi: 10.1001/jama.2010.1034. Epub [PubMed PMID: 20664044]