Introduction
Glucose is the most abundant carbohydrate in peripheral circulation, and the blood glucose test is the most frequently performed analysis in the clinical laboratory.[1] The body tightly maintains fasting blood glucose levels within the range from 70 to 99 mg/dL through metabolic processes such as gluconeogenesis, glycogenolysis, glycolysis, and glycogenesis. Gluconeogenesis is an anabolic pathway that synthesizes glucose from amino acids and other molecules. In contrast, glycogenolysis is a catabolic pathway involved in breaking glycogen into glucose for energy use.[2] These pathways are activated when the body signals an increased demand for glucose, primarily mediated by the hormone glucagon.
Conversely, glycolysis is a catabolic process that breaks down glucose, and glycogenesis is an anabolic process involved in the buildup of glycogen from glucose molecules. These pathways are activated when the body needs to reduce blood glucose levels, such as after a heavy meal, and are primarily mediated by the hormone insulin. When the body's regulatory hormones fail to maintain glucose levels, high blood glucose levels (hyperglycemia) and low blood glucose levels (hypoglycemia) can occur.[3]
In metabolic conditions such as diabetes mellitus, blood glucose is no longer maintained within normal limits, and thus, patients need medications for glycemic control. Currently, approximately 37 million people in the United States are diagnosed with diabetes mellitus, with over 90% of these cases being type 2 diabetes.[4] Diabetes is a significant cause of morbidity and mortality worldwide; however, hyperglycemia and hypoglycemia are observed in several other medical conditions. Accurate blood glucose measurements are essential in screening, diagnosing, and monitoring patients with a wide variety of metabolic conditions.[5]
Glucose oxidase is one of the most widely used enzymes for glucose detection because it reduces oxygen to hydrogen peroxide (H2O2) while also oxidizing glucose to gluconic acid. At neutral pH, glucose exists in 2 forms—α-D-glucose and β-D-glucose.[6] As the β-D-glucose is consumed in the reaction, the equilibrium of the 2 isomers of glucose is maintained by shifting production towards β-D-glucose, which allows glucose oxidase to act on all the glucose in the solution.[7]
Blood glucose is measured in the laboratory using the glucose oxidase-peroxidase (GOD-POD) method. In this method, glucose is oxidized to gluconic acid, whereas oxygen is simultaneously reduced to hydrogen peroxide by the enzyme glucose oxidase. Hydrogen peroxide is then split to form water and nascent oxygen by the enzyme peroxidase. The nascent oxygen reacts with 4-aminoantipyrine, and in the presence of phenol, this reaction produces quinoneimine, which is a colored compound that can be analyzed using colorimetric analysis. The intensity of the color produced correlates directly with the concentration of glucose in the sample. Colorimetric analysis is performed at 505 nm and compared to the standard, which is treated similarly.[8]
Glucose oxidase enzyme catalyzes the following reaction:
Glucose + O2 + H2O —> Gluconic acid + H2O2
Peroxidase enzyme catalyzes the following reaction:
H2O2 —> H2O + [O]
[O] + 4-aminoantipyrine + phenol —> quinoneimine + H2O
Specimen Requirements and Procedure
Register For Free And Read The Full Article
Search engine and full access to all medical articles
10 free questions in your specialty
Free CME/CE Activities
Free daily question in your email
Save favorite articles to your dashboard
Emails offering discounts
Learn more about a Subscription to StatPearls Point-of-Care
Specimen Requirements and Procedure
Sample Collection and Preparation
A blood sample is drawn into a sodium fluoride vial for glucose testing. Sodium fluoride inhibits the glycolytic enzyme enolase present in red blood cells (RBCs), thereby preventing falsely low blood glucose values due to its anti-glycolytic effects. Plasma is then obtained by centrifuging the blood sample for 10 minutes at 2000 rpm. When calculating blood glucose concentration, it is important to note that glucose concentration in whole blood is estimated to be 10% to 15% lower than the glucose concentration in plasma. The glucose concentration in the plasma's water content is equal to that in the water content of RBCs. However, plasma contains more water and therefore has a higher glucose concentration.[9] Obtaining the glucose concentration from the plasma is important for a more accurate blood glucose reading.
Materials Required for Glucose Estimation Using the GOD-POD Method
- Blood sample collected in a sodium fluoride vial
- Glucose reagent containing glucose oxidase, peroxidase, 4-amino antipyrine, and phenol
- Glucose standard solution containing a known glucose concentration (100 mg/dL)
- Constant temperature incubator set at 37 °C
- Pipettes for sample measuring
- Dry test tubes
- Colorimeter capable of measuring absorbance between 500 and 520 nm
Procedure
- Label 3 clean test tubes as Blank, Standard, and Test.
- Add 10 μL of distilled water to the test tube labeled as Blank.
- Add 10 μL of glucose standard (control) to the test tube labeled as Standard.
- Add 10 μL of the plasma to the test tube labeled as Test.
- Add 1 mL of GOD-POD reagent to each test tube.
- Mix all tubes thoroughly and incubate at 37 °C for 10 to 15 minutes.
- Measure the optical density of each sample using a colorimeter set at 505 nm.
Table. Reagent Preparation for Glucose Estimation Using the GOD-POD Method
|
Components |
Blank |
Standard |
Test |
|
Distilled water |
10 μL |
— |
— |
|
Glucose standard |
— |
10 μL |
— |
|
Plasma |
— |
— |
10 μL |
|
GOD-POD reagent |
1 mL |
1 mL |
1 mL |
Abbreviation: GOD-POD, glucose oxidase-peroxidase.
Testing Procedures
Enzymatic methods are the most widely used techniques for glucose analysis; however, other methods for glucose quantification include reducing and condensation methods. The least specific of these methods is the reducing method. This technique uses the reducing ability of glucose to reduce metals, such as copper, which yields a color change in the solution. The downfall of this method is that numerous reducing agents can interfere with glucose estimation and produce a significantly falsely elevated result.[6]
Condensation methods use the aldehyde group of glucose, which can react with aromatic compounds, such as o-toluidine, to form glucosamine that produces a green color. The color is then measured to estimate the glucose concentration in the sample. However, other aldoses can cross-react and cause inaccurate results.[6]
Enzymatic methods, such as the GOD-POD and hexokinase methods, are the most widely used methods for glucose estimation in clinical laboratories. The hexokinase method, in particular, is a highly specific modality for determining plasma glucose. The enzymatic method yields NADH through hexokinase-catalyzed transformations of glucose. NADH is then analyzed using spectrophotometry to determine the glucose concentration in the sample.[10]
Interfering Factors
High levels of reducing agents, such as uric acid, vitamin C, and bilirubin, may affect results. 4-aminoantipyrine, a component of the GOD-POD reaction, is an oxidizing agent that can neutralize excess reducing substances in the bloodstream and prevent interference with the coloring agent, phenol. Other potential interfering substances include excess triglycerides, abnormal hematocrit levels, and various drugs and medications.[11]
Results, Reporting, and Critical Findings
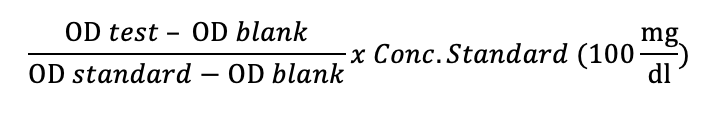
Generally, a normal fasting blood glucose range is from 70 to 99 mg/dL, a fasting blood glucose range from 100 to 125 mg/dL indicates pre-diabetes, and a fasting blood glucose of >125 mg/dL indicates diabetes mellitus. However, there are slight variations in reference ranges between different laboratories, and the reference values of the facility where the test was performed should be used.[12] The optical density (OD) of the Test, Standard, and Blank is measured to calculate a patient's blood glucose level using the GOD-POD method.
(OD of Test − OD of Blank) × Concentration of Standard) / (OD of Standard − OD of Blank)
The optical density of the blank should equal zero, and thus the formula is simplified to:
(OD of Test × Concentration of Standard) / OD of Standard
The optical density of the test is divided by the optical density of the standard, and the value obtained is then multiplied by the known glucose concentration of the mean (100 mg/dL). The value obtained from this calculation is the glucose concentration of the test sample.
Clinical Significance
Glucose is derived from the breakdown of carbohydrates, and its availability is essential for providing energy to the human body. The body tightly controls glucose within a normal, healthy range through endocrine hormones such as insulin and glucagon. Other hormones that can significantly affect glucose levels are cortisol, epinephrine, and thyroid hormone.[13][14] When symptoms of abnormally controlled blood glucose bring a patient to seek medical attention, a blood glucose measurement is an essential aspect of data collection to determine the pathology and treatment of the condition.
Some physiological conditions associated with hyperglycemia include a high carbohydrate diet, anxiety, emotional stress, and pregnancy. Pathological conditions associated with hyperglycemia include hyperpituitarism, hyperthyroidism, hyperadrenalism, and diabetes mellitus.[15]
Diabetes mellitus can be further classified into type I and type II. Type I diabetes is caused by autoimmune destruction of beta-cells within the pancreas and typically presents early in life. The beta-cells are responsible for insulin secretion; thus, in type 1 diabetes, there is an absolute insulin deficiency. Type II diabetes is more of a progressive loss of function of the beta-cells and is mainly due to insulin resistance. Type II diabetes typically occurs in adults with risk factors such as obesity, a sedentary lifestyle, and a family history of the disease. Chronically elevated glucose levels can lead to microvascular damage within the kidneys, the eyes, and the peripheral nerves; this damage can manifest as nephropathy, retinopathy, and neuropathy.[16]
Hyperpituitarism, hyperthyroidism, and hyperadrenalism are disorders in which aberrant hormonal signaling within the body increases the breakdown of molecules into glucose or the production of glucose. Although the pathophysiology of these disorders is different from that of diabetes mellitus, one of their manifestations is abnormally elevated blood glucose levels, and, thus, accurate measurements of glucose levels aid in the clinical diagnosis.[17]
Hypoglycemia can also occur physiologically, such as during prolonged fasting or after intense, strenuous exercise. Pathological conditions associated with hypoglycemia include insulin overdose or an insulin-secreting tumor, hypothyroidism, hypopituitarism, and Addison disease. Excess insulin causes the body to take up too much glucose from the blood and thus causes hypoglycemia. Hypothyroidism, hypopituitarism, and Addison disease are all disorders in which the body's endocrine hormones that signal the body's organs to increase blood glucose are lacking. Although other symptoms are associated with these diseases, hypoglycemia is a common and clinically relevant finding.[18]
Just as well-controlled blood glucose is essential for overall health, accurate glucose measurements are crucial for a clinician to provide the best care to a patient.
Quality Control and Lab Safety
A blank test and a standard (or control) with a known glucose concentration allow for accurate results independent of the technical faults with the colorimeter or instruments used in the analysis. Each test performed on an unknown sample should include samples with normal and abnormal glucose concentrations to allow for appropriate quality control. If the control results deviate from expected values, it is important to review the procedure, the colorimeter, and the instruments for possible issues.[19]
Enhancing Healthcare Team Outcomes
The physiological regulation of blood glucose and the clinical application of the GOD-POD method, an enzymatic assay widely used in laboratory medicine, are essential components of accurate diagnosis and effective management of glucose-related disorders. Accurate glucose measurement is critical for diagnosing and managing diabetes mellitus, endocrine disorders, and other metabolic conditions. The timely diagnosis, appropriate treatment, and quality laboratory practice strengthen the clinician's competence in glucose testing and clinical correlation.
Effective glucose management requires coordinated efforts across the healthcare team. Clinicians and advanced practitioners are responsible for ordering appropriate tests, interpreting results, and initiating treatment. Nurses play a key role in administering therapies, monitoring patient responses, and educating patients on glucose monitoring. Pharmacists contribute by verifying medication safety, identifying drug interactions, and advising on insulin and glucose-lowering agents. Laboratory professionals ensure accurate and timely test results, whereas dietitians support long-term glycemic control through nutritional guidance. Collaborative communication, shared decision-making, and role clarity enhance team performance, promote patient-centered care, reduce diagnostic delays, and improve outcomes in managing hypo- and hyperglycemia.
Media
References
Bonetti G, Cancelli V, Coccoli G, Piccinelli G, Brugnoni D, Caimi L, Carta M. Which sample tube should be used for routine glucose determination? Primary care diabetes. 2016 Jun:10(3):227-32. doi: 10.1016/j.pcd.2015.11.003. Epub 2015 Dec 4 [PubMed PMID: 26657574]
Nakrani MN, Wineland RH, Anjum F. Physiology, Glucose Metabolism. StatPearls. 2025 Jan:(): [PubMed PMID: 32809434]
Han HS, Kang G, Kim JS, Choi BH, Koo SH. Regulation of glucose metabolism from a liver-centric perspective. Experimental & molecular medicine. 2016 Mar 11:48(3):e218. doi: 10.1038/emm.2015.122. Epub 2016 Mar 11 [PubMed PMID: 26964834]
Level 3 (low-level) evidenceHossain MJ, Al-Mamun M, Islam MR. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health science reports. 2024 Mar:7(3):e2004. doi: 10.1002/hsr2.2004. Epub 2024 Mar 22 [PubMed PMID: 38524769]
Reed J, Bain S, Kanamarlapudi V. A Review of Current Trends with Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future Perspectives. Diabetes, metabolic syndrome and obesity : targets and therapy. 2021:14():3567-3602. doi: 10.2147/DMSO.S319895. Epub 2021 Aug 10 [PubMed PMID: 34413662]
Level 3 (low-level) evidenceWalker HK, Hall WD, Hurst JW, McMillin JM. Blood Glucose. Clinical Methods: The History, Physical, and Laboratory Examinations. 1990:(): [PubMed PMID: 21250092]
Tao Z, Raffel RA, Souid AK, Goodisman J. Kinetic studies on enzyme-catalyzed reactions: oxidation of glucose, decomposition of hydrogen peroxide and their combination. Biophysical journal. 2009 Apr 8:96(7):2977-88. doi: 10.1016/j.bpj.2008.11.071. Epub [PubMed PMID: 19348778]
Ambade VN, Sharma YV, Somani BL. METHODS FOR ESTIMATION OF BLOOD GLUCOSE : A COMPARATIVE EVALUATION. Medical journal, Armed Forces India. 1998 Apr:54(2):131-133. doi: 10.1016/S0377-1237(17)30502-6. Epub 2017 Jun 26 [PubMed PMID: 28775446]
Level 2 (mid-level) evidenceHoltkamp HC, Verhoef NJ, Leijnse B. The difference between the glucose concentrations in plasma and whole blood. Clinica chimica acta; international journal of clinical chemistry. 1975 Feb 22:59(1):41-9 [PubMed PMID: 1122647]
Sonagra AD, Zubair M, Motiani A. Hexokinase Method. StatPearls. 2025 Jan:(): [PubMed PMID: 36512662]
Ginsberg BH. Factors affecting blood glucose monitoring: sources of errors in measurement. Journal of diabetes science and technology. 2009 Jul 1:3(4):903-13 [PubMed PMID: 20144340]
Munekawa C, Okada H, Hamaguchi M, Habu M, Kurogi K, Murata H, Ito M, Fukui M. Fasting plasma glucose level in the range of 90-99 mg/dL and the risk of the onset of type 2 diabetes: Population-based Panasonic cohort study 2. Journal of diabetes investigation. 2022 Mar:13(3):453-459. doi: 10.1111/jdi.13692. Epub 2021 Oct 23 [PubMed PMID: 34624178]
Eom YS, Wilson JR, Bernet VJ. Links between Thyroid Disorders and Glucose Homeostasis. Diabetes & metabolism journal. 2022 Mar:46(2):239-256. doi: 10.4093/dmj.2022.0013. Epub 2022 Mar 24 [PubMed PMID: 35385635]
Møller N, Jørgensen JO. Effects of growth hormone on glucose, lipid, and protein metabolism in human subjects. Endocrine reviews. 2009 Apr:30(2):152-77. doi: 10.1210/er.2008-0027. Epub 2009 Feb 24 [PubMed PMID: 19240267]
Mouri M, Badireddy M. Hyperglycemia. StatPearls. 2025 Jan:(): [PubMed PMID: 28613650]
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010 Jan:33 Suppl 1(Suppl 1):S62-9. doi: 10.2337/dc10-S062. Epub [PubMed PMID: 20042775]
Sydney GI, Michalakis K, Nikas IP, Spartalis E, Paschou SA. The Effect of Pituitary Gland Disorders on Glucose Metabolism: From Pathophysiology to Management. Hormone and metabolic research = Hormon- und Stoffwechselforschung = Hormones et metabolisme. 2021 Jan:53(1):16-23. doi: 10.1055/a-1258-8625. Epub 2020 Oct 12 [PubMed PMID: 33045752]
Nakhleh A, Shehadeh N. Hypoglycemia in diabetes: An update on pathophysiology, treatment, and prevention. World journal of diabetes. 2021 Dec 15:12(12):2036-2049. doi: 10.4239/wjd.v12.i12.2036. Epub [PubMed PMID: 35047118]
Kinns H, Pitkin S, Housley D, Freedman DB. Internal quality control: best practice. Journal of clinical pathology. 2013 Dec:66(12):1027-32. doi: 10.1136/jclinpath-2013-201661. Epub 2013 Sep 26 [PubMed PMID: 24072731]
Level 2 (mid-level) evidence